When you take a pill for high blood pressure, an antibiotic for a sinus infection, or even a daily vitamin, you’re not just getting the intended benefit. Your body reacts in ways you might not expect-sometimes mildly, sometimes dangerously. These unexpected reactions are called drug side effects. They’re not mistakes. They’re part of how drugs work. And understanding them isn’t just helpful-it can be life-saving.
What Exactly Is a Drug Side Effect?
A drug side effect is any effect that happens when you take a medication, other than the one you’re taking it for. The U.S. Food and Drug Administration (FDA) defines them as "unwanted, undesirable effects that are possibly related to a drug." That’s broad, and it’s meant to be. Side effects can be harmless, annoying, or serious. Some even turn out to be helpful.
For example, minoxidil was originally developed as a blood pressure medication. Doctors noticed patients taking it grew thicker hair. That’s how Rogaine was born. The hair growth wasn’t the goal-it was a side effect. And for many, it became the reason they kept using it.
Not all side effects are bad. But they’re still side effects. The technical definition from StatPearls (2024) says they’re "a predictable or dose-dependent effect of a drug that is not the principal effect for which the drug was used." That means: if it’s not the main purpose, and it’s caused by the drug, it’s a side effect-even if it’s good.
This is different from an allergic reaction. An allergy involves your immune system and can cause swelling, hives, or anaphylaxis. A side effect? That’s your body just reacting chemically to the drug’s action. Confusing the two leads people to stop medications unnecessarily.
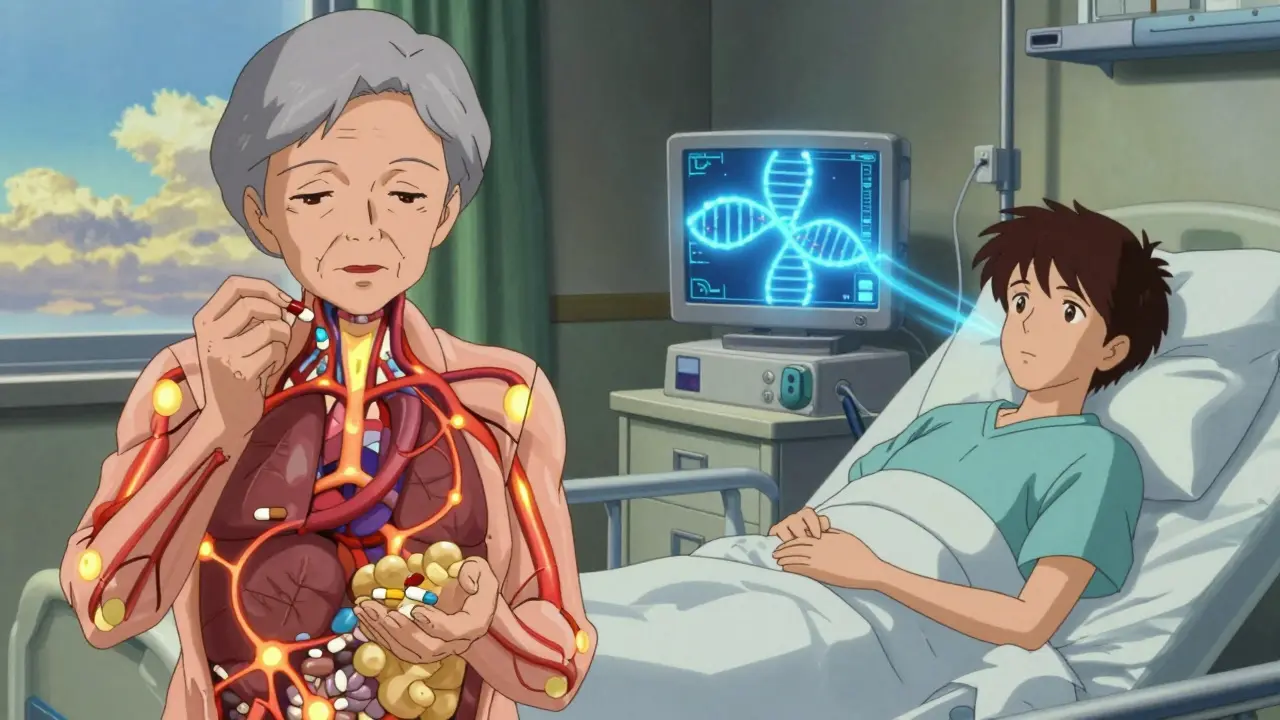
Why Do Side Effects Happen?
Drugs don’t target just one part of your body. They move through your bloodstream, interact with cells, and affect systems you didn’t even know they could touch. That’s why side effects happen.
Take beta-blockers, used for heart conditions. They slow your heart rate-that’s the goal. But they also act on receptors in your lungs. In people with asthma, that can cause wheezing or shortness of breath. As Dr. Jerry Avorn from Harvard puts it: "Many side effects represent therapeutic effects in the wrong tissue."
There are two main types of side effects:
- Type A: Predictable, dose-dependent, and common. These make up 85-90% of all side effects. Think nausea from antibiotics or dizziness from blood pressure meds. They happen because the drug’s chemistry affects more than just the target.
- Type B: Unpredictable, rare, and not tied to dose. These are often immune-related or genetic. For example, a person might develop a severe skin rash from a drug that 99% of others tolerate fine. These are harder to spot before they happen.
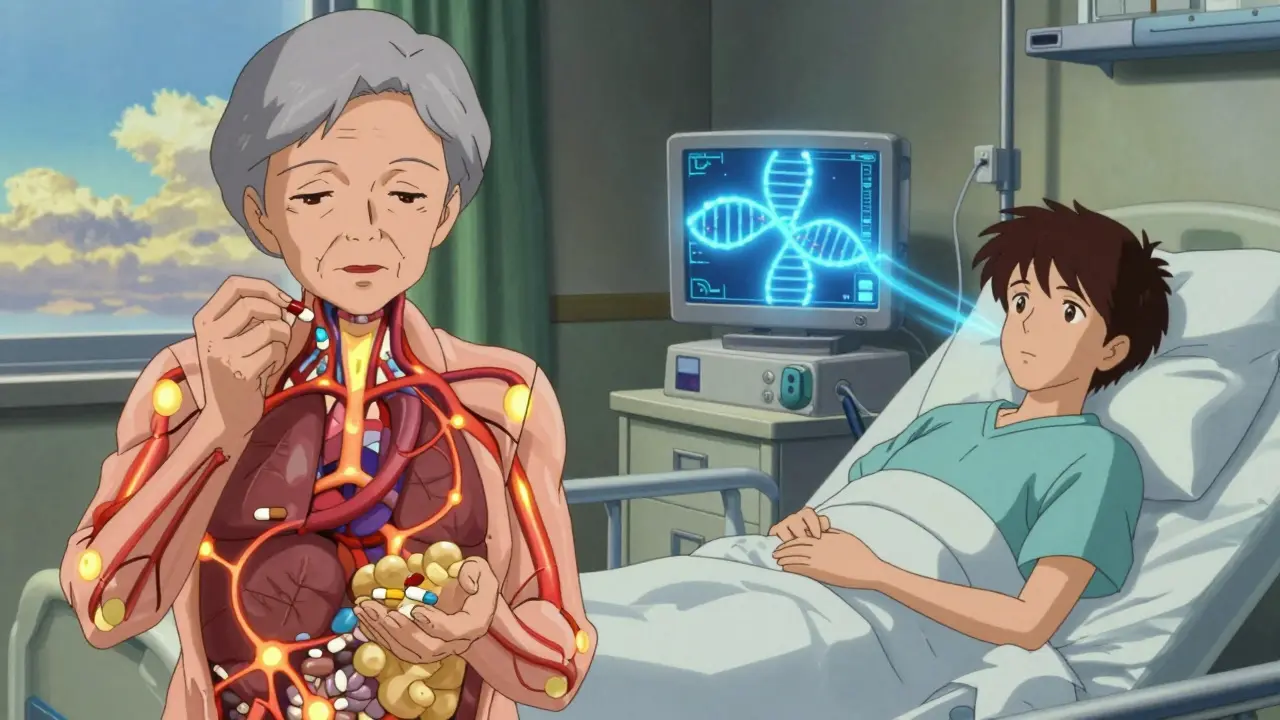
What Makes Some People More Likely to Have Side Effects?
Not everyone reacts the same way. Some people get side effects easily. Others don’t. Why?
- Age: People over 65 are 3 to 5 times more likely to experience serious side effects. Their bodies process drugs slower. They often take multiple medications. And their organs-liver, kidneys-aren’t as efficient.
- Multiple medications: Taking five or more drugs at once increases your risk of side effects by 88%. Each drug can interact with another, changing how they’re absorbed, broken down, or eliminated.
- Chronic health conditions: If you have kidney disease, your body can’t clear drugs as well. That means drugs build up, increasing side effect risk. People with kidney disease have 4.2 times more medication-related side effects than those with healthy kidneys.
- Genetics: Your genes control how your body breaks down drugs. About 40-95% of people have genetic variations in enzymes like CYP450 that affect drug metabolism. For example, if you have a CYP2C19 variant, clopidogrel (a blood thinner) won’t work well for you-and you’re at higher risk of a heart attack. That’s why pharmacogenetic testing is now recommended before starting certain drugs.
- Drug interactions: Grapefruit juice can block the enzymes that break down statins, leading to dangerous muscle damage. St. John’s Wort can make birth control pills fail. Even over-the-counter painkillers like ibuprofen can raise your blood pressure if you’re already on hypertension meds.
Common Side Effects and Real Examples
Some side effects are so common, you’ve probably heard of them. But how common are they really?
- NSAIDs (like ibuprofen or naproxen): About 15-30% of regular users develop stomach irritation or ulcers. That’s why doctors often prescribe a stomach-protecting drug alongside them for long-term users.
- Antibiotics (like amoxicillin or ciprofloxacin): 5-30% of people get diarrhea. That’s because antibiotics kill good bacteria in your gut along with the bad ones. In rare cases, this leads to a dangerous infection called C. diff.
- Doxycycline: A common antibiotic for acne and infections. About 10% of users develop severe sunburns because it makes skin extra sensitive to UV light.
- Chemotherapy drugs: Nausea and vomiting affect 30-90% of patients, depending on the drug. New anti-nausea drugs have improved this, but many still struggle.
- Immune checkpoint inhibitors (cancer immunotherapy): These drugs help the immune system fight cancer-but they can also turn it against healthy organs. About 60-85% of patients get some kind of immune-related side effect: colitis, thyroid problems, or even inflammation of the lungs.
- SGLT2 inhibitors (for type 2 diabetes): These drugs help lower blood sugar, but the FDA added a boxed warning in 2022 after studies showed a 1.77-fold increased risk of lower limb amputations.
Even vaccines have side effects. The CDC found that mRNA COVID-19 vaccines caused myocarditis (heart inflammation) in about 40.6 cases per million second doses in young men aged 12-29. That sounds scary-but the risk of heart damage from COVID-19 itself is far higher.
Side Effects vs. Nocebo Effects
Not every symptom you feel after taking a pill is caused by the drug. Sometimes, it’s your brain.
A nocebo effect is when you expect a side effect, so you feel it-even if you’re taking a sugar pill. A 2022 Mayo Clinic study found that 62% of patients who stopped statins due to muscle pain had no real symptoms when given a placebo. Their brains were tricking them.
This matters because people stop life-saving medications based on fear, not fact. One survey showed 57% of people believed every side effect listed on the label would definitely happen to them. That’s not how it works. Side effects are listed with frequencies: common, uncommon, rare. Most people won’t get most of them.
What Should You Do If You Experience a Side Effect?
Don’t panic. Don’t quit cold turkey. Do this:
- Write it down. When did it start? How bad is it? Does it get worse with food or activity?
- Check the frequency. Is it listed as "common" or "rare"? If it’s common, your doctor likely knows how to manage it.
- Call your doctor. Don’t assume it’s "just normal." Some side effects need quick action-like swelling, chest pain, or sudden confusion.
- Don’t switch or stop on your own. Stopping blood pressure or antidepressant meds suddenly can be dangerous.
- Report it. Use the FDA’s MedWatcher app or report to MedWatch. Every report helps improve drug safety.

How Are Side Effects Monitored and Regulated?
Drug safety doesn’t end when a pill hits the market. It’s a lifelong process.
The FDA’s FAERS database has over 22 million reports of side effects. The European Union’s EudraVigilance system processed 1.7 million reports in 2022 alone. These systems catch patterns: if 50 people report the same rare reaction, regulators investigate.
New tools are making this faster. The FDA’s Sentinel Initiative uses electronic health records from 200 million Americans to detect side effects 18-24 months faster than old methods. Machine learning models now predict NSAID-related stomach bleeding with 82% accuracy by analyzing patient history.
Drug labels are updated constantly. In 2022, the FDA added 9 new boxed warnings-the strongest safety alert-to drug labels based on side effect data. These warnings appear on the front of the package, like the one for SGLT2 inhibitors and amputation risk.
What Can You Do to Reduce Your Risk?
You’re not powerless. Here’s how to protect yourself:
- Know your meds. Ask your pharmacist: "What are the most common side effects? What should I watch for?" Don’t just take the pill-understand it.
- Use the Beers Criteria. If you’re over 65, ask your doctor if any of your meds are on this list of drugs to avoid in older adults.
- Get pharmacogenetic testing. If you’re on antidepressants, blood thinners, or cancer drugs, ask if genetic testing is right for you. It could prevent a bad reaction.
- Use the FDA’s Medication Guides. These are simple, plain-language sheets that come with 185 high-risk drugs. They’re required by law. Read them.
- Keep a side effect journal. Note when symptoms start, what you took, and how long they last. Bring it to appointments.
Final Thought: Side Effects Aren’t the Enemy
They’re a sign that drugs are working-just not only where you want them to. The goal isn’t to avoid all side effects. It’s to understand them, manage them, and weigh them against the benefits.
A 2023 study found that 65% of patients with chronic illness care more about side effects than about how well the drug works. That’s understandable. But the best treatment isn’t the one with zero side effects-it’s the one where the benefits clearly outweigh the risks.
If you’re unsure, talk to your doctor. Ask: "What’s the most likely side effect? How serious is it? Is there a safer alternative?" You’re not being difficult. You’re being smart.
Drug side effects aren’t something to fear blindly. They’re something to understand. And once you do, you take back control.