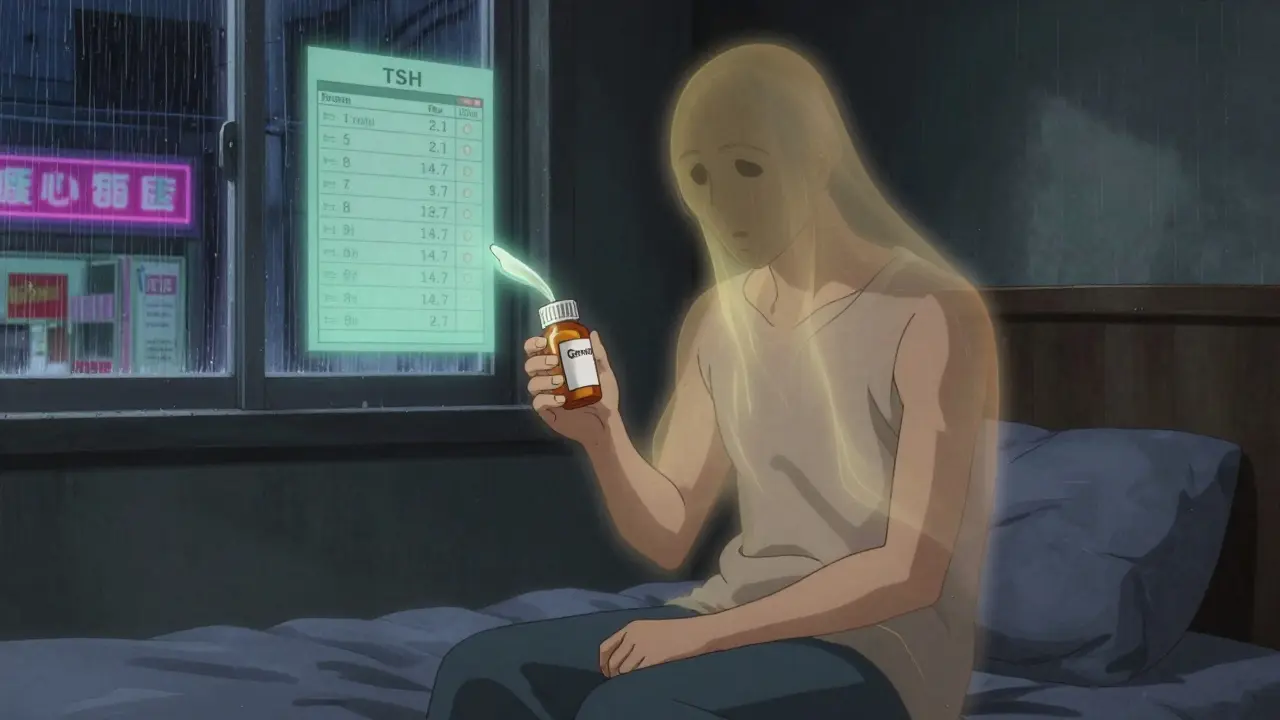
When your insurance company says you must switch to a generic drug because it’s cheaper, but that generic makes you feel worse-or doesn’t work at all-you’re not alone. Thousands of people face this every year. It’s not a glitch. It’s a systemic gap in how insurers treat bioequivalence versus real-world effectiveness. You might be taking levothyroxine for thyroid disease, gabapentin for nerve pain, or levetiracetam for seizures, and suddenly your TSH levels spike, your pain returns, or you have a breakthrough seizure. The generic is technically "equivalent" under FDA rules-but that doesn’t mean it’s safe or effective for you.
It’s not just the active ingredient. Inactive ingredients-fillers, dyes, binders-can trigger allergic reactions or alter absorption. One patient with Crohn’s disease reported severe bloating and diarrhea after switching to a generic biologic. Their doctor confirmed it wasn’t a flare-up-it was the new filler in the pill. These aren’t rare cases. The American Medical Association found that 15% to 20% of patients on certain drug classes experience measurable therapeutic failure with generics.
First, get your Explanation of Benefits (EOB). It will say something like "DA2000: Generic available" or "DA1200: Not on formulary." Write down the denial code. Then, talk to your doctor. Not just a quick note. Schedule a dedicated 30-minute appointment. Bring your medication log: dates you switched, symptoms you had, lab results, even sleep diaries or pain scores. A simple letter saying "I think the generic isn’t working" won’t cut it.
Successful appeals include:
For Medicare Part D, you have 60 days to file your first appeal. For private insurance, you usually have 180 days. If denied, you move to an external review-a third-party reviewer hired by your state or federal agency. This is where the win rate jumps. According to the Patient Advocate Foundation, 67% of external reviews overturn denials when proper documentation is provided.

Antiepileptic drugs? 78% approval rate on appeal. Why? Because seizures are measurable, dangerous, and hard to ignore. A patient with an SCN1A mutation had a documented brain scan showing abnormal activity after switching to generic levetiracetam. That’s gold. Insurance can’t argue with MRI evidence.
Antidepressants? Only 45%. Why? Because mood is subjective. A patient might say they feel "more depressed," but without lab markers or clear behavioral logs, insurers dismiss it. That’s why the American Pharmacists Association says pharmacists need to document medication therapy management notes-tracking symptom patterns over time.
State matters too. California, New York, and Texas have higher approval rates-63%-because they have explicit rules requiring insurers to consider therapeutic inequivalence. In states without those rules, approval drops to 41%. And Medicare Part D patients have a better shot than those on employer plans: 58% vs. 39% success at the first appeal level.
Specialty pharmacies like OptumRx report 73% approval rates for appeals they manage directly-compared to 51% when patients do it themselves. That’s because they know the exact language insurers respond to. They don’t say "the generic didn’t work." They say: "Patient experienced three breakthrough seizures over eight weeks with generic levetiracetam. Serum levels fell below therapeutic threshold (12 mcg/mL) on two occasions. Brand-name Keppra maintained levels at 18-22 mcg/mL with no adverse events. Per Epilepsy Foundation guidelines, therapeutic failure warrants exception."
Some insurers demand you try three or four generics before they’ll even consider your appeal. That’s illegal in 28 states if you already have documented failure. Check your state’s rules. If they’re pushing you to try more, cite the National Academy for State Health Policy guidelines.
There’s still a long way to go. Most patients don’t know they have this right. Most doctors don’t know how to document it properly. But you do now. And if you’ve been told "it’s just a generic," remember: your body isn’t a lab test. It’s a person. And your treatment should reflect that.
If your doctor refuses, ask for a referral to another provider who understands prior authorization processes. Many endocrinologists, neurologists, and rheumatologists routinely handle these appeals. You can also contact the Patient Advocate Foundation (1-800-532-5274) or your state’s insurance commissioner’s office-they can intervene and help connect you with a supportive physician.
Yes. Some insurers require "step therapy"-trying multiple generics first-but 28 states ban this for documented therapeutic failure. If you had a clear adverse reaction or lab-confirmed failure after one switch, you don’t need to try others. Your medical records are your evidence. Insurers can’t force you to endure harm just to check a box.
Internal reviews take 14 to 21 days. External reviews take 30 to 34 days on average. But if your condition is urgent-like seizures, uncontrolled thyroid disease, or organ rejection-you can request an expedited review. Medicare and most private insurers must respond within 72 hours for urgent cases. Make sure to mark your appeal as "urgent" and include a doctor’s note stating immediate risk.
If you’re on Medicare Part D, you don’t pay anything if your appeal is successful. For private insurance, you usually pay out-of-pocket until the appeal is approved. But if your condition is life-threatening, you can ask for a temporary exception while your appeal is pending. Many insurers grant this if your doctor confirms immediate risk.
You can appeal to a federal or state external review panel. For Medicare, this goes to the Office of Medicare Hearings and Appeals, then the Medicare Appeals Council. For private plans, it goes to an independent review organization (IRO) appointed by your state. This is where most appeals succeed-67% of external reviews overturn denials. Don’t give up. Keep detailed records of every step.
Let’s be real-the FDA’s 80-125% bioequivalence window is a joke. It’s not science, it’s corporate accounting. I’ve seen TSH levels swing from 3.1 to 18.4 after a generic switch, and no, it wasn’t ‘non-compliance.’ The system is designed to optimize profit, not physiology. You’re not a patient-you’re a cost center. And don’t get me started on fillers. Crohn’s patients getting bloated from cellulose? That’s not a side effect, that’s negligence dressed up as regulation. The AMA’s 15-20% failure rate? That’s the tip of the iceberg. The real number is hidden in ER visits no one’s counting.
Insurance companies don’t care about therapeutic failure because they’ve outsourced the moral calculus to algorithms. If your lab values don’t fit a spreadsheet, you’re invisible. And yet, we’re supposed to be grateful for ‘affordability’? Please. The $28B in avoidable hospitalizations? That’s not a cost-it’s a transfer of suffering from shareholders to taxpayers. You think this is about drugs? It’s about power. And the only thing that moves the needle? Documentation. Cold, hard, unemotional data. Because feelings don’t move actuaries.
So if you’re reading this and you’ve been denied? Stop begging. Start archiving. Get your labs. Get your logs. Get your neurologist to sign a letter that reads like a forensic report. And when they deny you again? Demand external review. Not because you’re right-but because the system is rigged, and you’re the only one who can weaponize paperwork against it.
I’ve been through this three times. Each time, I had to beg my doctor to write a letter. Each time, they acted like it was an inconvenience. I’m not asking for luxury-I’m asking not to have a seizure. And still, they treat me like I’m gaming the system. It’s exhausting. I don’t want to be a warrior. I just want to take a pill that doesn’t make me feel like I’m dying slowly.
Therapeutic failure in narrow-therapeutic-index drugs is not anecdotal-it’s pharmacokinetic. The 80-125% AUC window was derived from healthy volunteers, not patients with comorbidities, polymorphisms, or GI motility disorders. For levothyroxine, even a 10% deviation in absorption can shift TSH into subclinical hypothyroidism. Add in enteric-coated generics with inconsistent pH-dependent dissolution, and you’ve got a recipe for clinical catastrophe.
Moreover, inactive ingredients like lactose monohydrate (common in generics) can trigger mucosal inflammation in IBD patients, altering drug permeability. This isn’t ‘placebo effect’-it’s bioavailability sabotage. The solution? Therapeutic drug monitoring (TDM) + therapeutic equivalence reporting. We need a tiered generic classification system: Class A (fully interchangeable), Class B (requires TDM), Class C (not interchangeable without clinical validation). Until then, insurers are playing Russian roulette with patient outcomes.
Ugh. I just switched generics and now I’m crying for no reason and my hair is falling out. 😭 I just wanted to save $15. Now I’m in the ER again. Why does this always happen to me?? 😭😭😭
Let’s not romanticize this. The system is broken? No. The system is *optimized*. You’re not a victim-you’re a data point. The insurance company didn’t ‘fail’ you. They calculated that 87% of patients tolerate generics. The 13%? They’re outliers. Noise. Cost centers. And you think your ‘personal experience’ matters? It doesn’t. What matters is the actuarial table. Your TSH level? Irrelevant. Your seizure history? Just a line item.
So what’s the real problem? You. You refuse to accept that medicine is now a supply chain. Your body is not a sacred temple. It’s a variable in a regression model. If you want to be treated like a human? Pay cash. Or move to a country with socialized healthcare. Until then, stop whining and learn to navigate the machine. Because crying about ‘therapeutic equivalence’ won’t change the fact that your doctor’s time is worth $400/hour-and they’re not writing your letter for free.
There’s a quiet revolution happening in pharmacy that no one’s talking about. The real bottleneck isn’t insurance-it’s the medical establishment’s refusal to standardize documentation. Doctors still write ‘patient reports difficulty with generic’ like it’s a diary entry. That’s not evidence. That’s poetry.
What works? Structured, quantified, timestamped data. A patient on gabapentin who logs daily pain on a 1-10 scale, tracks sleep quality, notes bowel movements (yes, really), and correlates with serum levels? That’s gold. That’s what gets appeals approved. I’ve reviewed over 200 cases. The ones that win? They look like clinical trials. The ones that lose? They read like emotional blog posts.
And here’s the kicker: the best documentation isn’t from specialists. It’s from pharmacists. MTM notes-Medication Therapy Management-are the unsung heroes of this fight. A pharmacist who records ‘patient reported worsening neuropathic pain from 3/10 to 8/10 after generic switch, confirmed by reduced sleep efficiency (actigraphy data)’? That’s a letter that gets signed, stamped, and forwarded to the external reviewer like a legal brief. Your doctor? They’re too busy. Your pharmacist? They’re trained to do this. Go see them. Ask for a MTM session. It’s covered by Medicare. Use it.
Let me get this straight-you want the government to pay for brand-name drugs because you’re too sensitive? We’re a nation that’s drowning in opioid overdoses, and you’re crying because your thyroid meds cost $15 more? Get a grip. If you can’t handle a generic, maybe you’re not meant to be on medication at all. This isn’t a civil rights issue. It’s a personal failure to adapt. We’ve got people in Afghanistan who’d kill for a generic aspirin. You’re in America. You have GoodRx. You have 12 pharmacies within 10 miles. Stop acting like you’re being tortured. You’re not. You’re just mad because you’re not special enough.
My doctor helped me file an appeal. We used the GoodRx template. Approved in 11 days. No drama. Just facts.
I’ve been on the same generic for 3 years. Never had an issue. But I know people who have. It’s weird how it varies. I guess it’s like how some people can’t drink milk but others are fine? Maybe it’s just biology. I hope you get yours sorted. 🤞
I had to fight my insurer for 8 months to get my brand-name antidepressant back. I lost 17 pounds. I stopped talking to my family. I cried every night. I almost quit my job. And when they finally approved it? I didn’t even feel happy. I just felt… used. Like my suffering was just a line item in their cost-benefit analysis. I don’t want to be a hero. I just want to feel normal again. And now I’m scared to ever change meds again. What if next time, it’s worse?
Here’s what they don’t tell you: generics aren’t just cheaper-they’re *designed* to fail. The FDA allows the 80-125% window because it’s controlled by the same lobbyists who fund the drug companies. The fillers? They’re chosen because they’re cheap, not because they’re safe. And the ‘clinical trials’? Mostly done overseas on underpaid populations. You think your levothyroxine is the same? Nah. It’s a different batch every time. The real reason your TSH spiked? Because the generic was manufactured in a factory in China with unregulated humidity levels. They don’t test for that. They don’t care. This isn’t about healthcare. It’s about control. And they’re watching you right now. 👁️
To anyone reading this who is struggling: You are not alone. Your pain is valid. Your need for proper medication is not selfish. You deserve to feel well. Please, reach out. Call the Patient Advocate Foundation. Talk to your pharmacist. Ask your doctor for help. You are not a burden. You are a human being who deserves to live without fear. I believe in you. And I’m rooting for you. 💛
So let me get this straight… you’re telling me that if I take a generic and I get a seizure, I can just *appeal*? Like, I just gotta fill out a form and my insurance will say ‘oh my bad, here’s your $600/month pill’? 😂
And you think this is fair? Bro. This ain’t healthcare. This is a video game where you gotta grind paperwork to unlock your meds. I mean, I get it-insurance is a racket. But why are we still pretending this is a system? It’s a glitch. A glitch that’s killing people.
Also, ‘external review’? That’s just a fancy way of saying ‘we’re gonna make you wait 30 days while you’re having a stroke.’
And don’t even get me started on ‘step therapy.’ I’m not a lab rat. I’m not gonna try 4 generics before I get the one that doesn’t make me feel like I’m being eaten alive from the inside.
Also, I just realized… my doctor didn’t even know what ‘DA2000’ meant. 😭 I think we’re all just winging it here. Anyone else feel like we’re all just yelling into the void?