
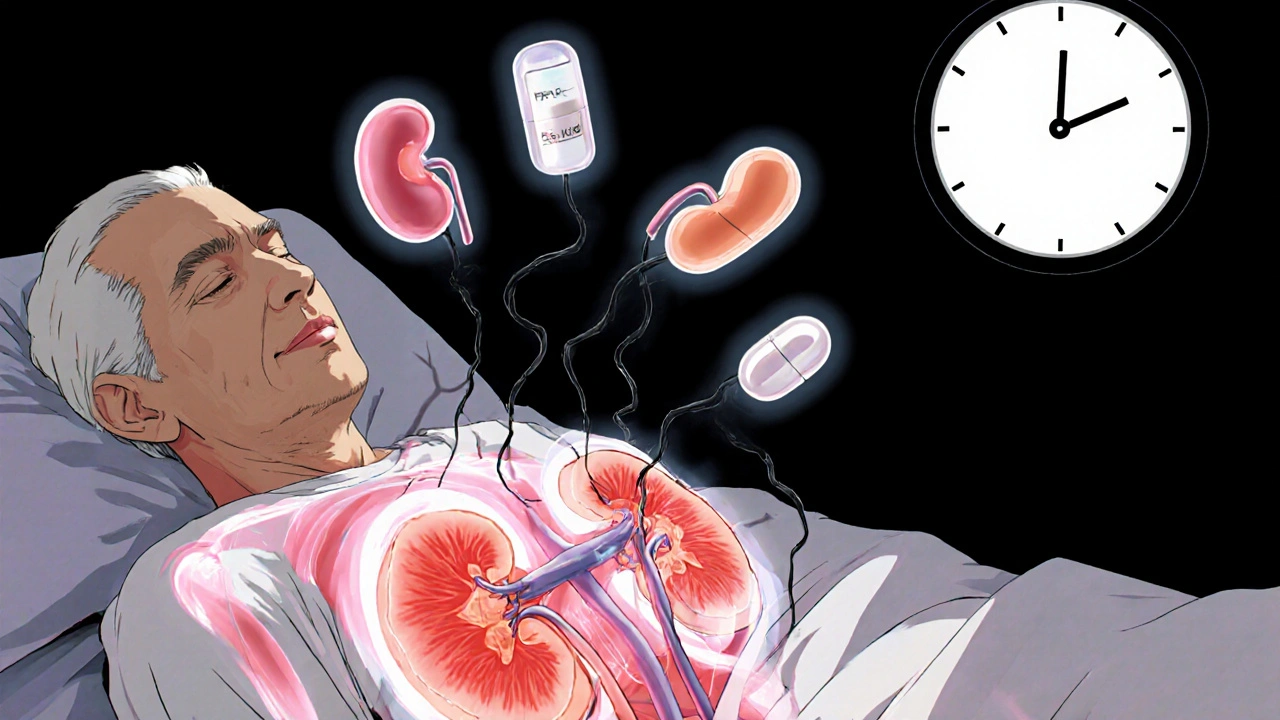
When your kidneys start acting up-swelling, fatigue, little urine output-it’s easy to blame a bad diet or dehydration. But what if the real culprit is something you took every day for months? Acute interstitial nephritis (AIN) is one of the most underrecognized causes of sudden kidney failure, and it’s often triggered by medications you’d never think could harm your kidneys. Unlike infections or stones, AIN doesn’t show up on routine blood tests with obvious red flags. It creeps in silently, especially in older adults on multiple pills. And by the time it’s diagnosed, the damage might already be lasting.
Acute interstitial nephritis is inflammation in the spaces between the kidney’s tubules-the parts that filter waste and balance fluids. This isn’t a disease you catch; it’s a reaction. Your immune system mistakes a drug for a threat and sends immune cells into your kidneys. These cells swell the tissue, block filtration, and reduce kidney function fast. The result? Acute kidney injury. Blood creatinine spikes. Urine output drops. You feel tired, nauseous, maybe even have a low fever.
It’s not rare. About 5 to 15% of people admitted for sudden kidney failure have AIN. And in most cases-60 to 70%-it’s caused by a drug. The problem? Doctors don’t always connect the dots. Symptoms mimic urinary tract infections, dehydration, or even the flu. Many patients wait weeks before getting the right diagnosis. By then, the kidneys have been under siege.
Over 250 medications have been linked to AIN. But three classes stand out today:
Other triggers include immune checkpoint inhibitors (used in cancer treatment), diuretics, and even some herbal supplements. The risk goes up sharply if you’re over 65, taking five or more medications, or already have reduced kidney function.
Medical textbooks still teach the "hypersensitivity triad": rash, fever, and eosinophilia. But in reality, less than 10% of AIN patients have all three. Even just one of these signs shows up in fewer than half of cases. Relying on this triad to diagnose AIN is like waiting for a hurricane to hit before you close the windows.
More common are vague symptoms: feeling off, loss of appetite, mild nausea, joint aches, or just persistent fatigue. Many patients are misdiagnosed with a UTI or viral illness. One Reddit thread from r/kidneydisease showed 28 posts where people were told they had a bladder infection-when their kidneys were inflamed. The delay? Often 2 to 4 weeks. And every day without stopping the drug makes recovery less likely.
There’s no blood test that confirms AIN. Urine tests might show white blood cells, eosinophils, or protein-but these aren’t reliable. A 67-gallium scan or eosinophiluria test? Not accurate enough for clinical use.
The only definitive way to diagnose AIN is a kidney biopsy. A tiny sample of kidney tissue is taken under local anesthesia and looked at under a microscope. Pathologists look for immune cell buildup, swollen tissue, and signs of tubule damage. It sounds scary, but it’s a quick outpatient procedure. And it’s worth it. Without it, you might miss AIN-or mistake it for something else entirely, like glomerulonephritis or acute tubular necrosis.
Doctors now use a "clinical suspicion" approach. If you’ve recently started a new drug and your kidney function drops, AIN is on the list-even if you don’t have a rash or fever. The American Society of Nephrology says this mindset is non-negotiable.
Once AIN is suspected, the first and most critical step is stopping the offending drug. Guidelines say this should happen within 24 to 48 hours. In one Medscape survey of 120 patients, 65% felt better within 72 hours of quitting the medication.
But stopping the drug doesn’t guarantee full recovery. Here’s what you can expect based on the cause:
For severe cases-where eGFR drops below 30 mL/min/1.73m² or kidney function keeps worsening after 72 hours-doctors may prescribe corticosteroids. The typical protocol is methylprednisolone (0.5-1 mg/kg/day) for 2-4 weeks, followed by a slow taper of prednisone over 6-8 weeks. There’s no large trial proving steroids work, but experts like Dr. Ronald J. Falk from UNC say they help when given early. The European Renal Association agrees: early steroids improve outcomes in severe AIN.
Some patients need dialysis. About 15-20% do, usually for 2 to 6 weeks. One patient case from the American Kidney Fund described a 63-year-old woman who needed dialysis for three weeks after taking omeprazole for 18 months. A year later, her eGFR was still only 45-down from 85 before the AIN.

Most people assume if their creatinine drops back to normal, they’re fine. But that’s not always true. About 30% of AIN patients develop chronic kidney disease (CKD) stage 3 or higher within a year. That means their kidneys never fully recover. The damage becomes permanent.
NSAID-induced AIN has the highest progression rate-42% go on to CKD. PPIs aren’t far behind. Even if you feel fine after stopping the drug, your kidneys may still be scarred. A 2022 study from the University of North Carolina found that urinary CD163, a protein released by damaged kidney cells, can predict long-term outcomes. It’s not yet standard, but it’s a promising tool to replace biopsies in the future.
For older adults on long-term PPIs or NSAIDs, the risk keeps growing. Between 2010 and 2020, drug-induced AIN cases rose by 27%. By 2025, experts predict a 15% increase if prescribing habits don’t change. The FDA issued a safety warning about PPIs in 2021 after 1,248 cases were reported over a decade. That’s not a small number-it’s a public health signal.
If you’re on long-term PPIs, NSAIDs, or multiple medications, here’s what matters:
AIN is preventable. It’s treatable. But only if you catch it early. The longer you wait, the less likely your kidneys will bounce back.
Yes, in many cases-if caught early. Stopping the triggering drug is the most important step. About 70-80% of patients with antibiotic-induced AIN recover fully. But for NSAID or PPI-induced cases, recovery is less certain. About 30-50% of patients end up with permanent kidney damage, especially if diagnosis is delayed beyond two weeks.
No. Antibiotics typically cause milder, more reversible inflammation. NSAIDs and PPIs are more likely to cause lasting harm, especially with long-term use. The key factor isn’t the drug alone-it’s how long the inflammation goes untreated. Early removal of the drug gives kidneys the best shot at healing.
No. Re-exposure to the same drug can trigger AIN again-and faster, and more severely. Once you’ve had AIN from a PPI, you should avoid all drugs in that class permanently. Your doctor can recommend alternatives like H2 blockers (ranitidine, famotidine) or lifestyle changes to manage acid reflux.
In clinical practice, yes. While doctors may suspect AIN based on symptoms and timing, no blood or urine test can confirm it. A biopsy is the only way to see the immune cell buildup in the kidney tissue. Skipping it risks misdiagnosis. Most nephrologists agree: if AIN is suspected, biopsy is the standard of care.
Recovery time depends on the drug. Antibiotic-induced AIN often improves in 10-14 days. NSAID cases take 3-4 weeks. PPI-induced AIN can take 5 weeks or longer. Dialysis may be needed for 2-6 weeks in severe cases. Full recovery can take months, and some patients never regain their original kidney function.
Researchers are working on biomarkers. A 2022 study found that urinary CD163, a protein released by damaged kidney cells, detected AIN with 89% accuracy. It’s not yet available in most clinics, but it’s the most promising non-invasive tool on the horizon. For now, biopsy remains the gold standard.
Just had my third biopsy in 18 months because my creatinine kept creeping up. Turns out it was omeprazole. I took it for 5 years for "heartburn." No rash, no fever. Just exhaustion and swelling. Docs said "maybe dehydration." I almost died waiting for them to connect the dots.
Stop PPIs if you’re over 60 and on more than 3 meds. It’s not a harmless pill. It’s a silent killer.
Oh wow. So this is why Big Pharma doesn’t want you to know about this. They’ve been pushing PPIs like candy since the 90s. And now? Kidney failure on a subscription.
They even made them OTC so you’d never see a doctor. That’s not an accident. That’s a profit scheme. I’ve seen 7 people in my town with this. All on Prilosec. All told it was "just aging."
Someone’s making billions off our ruined kidneys. And we’re just supposed to be grateful for the heartburn relief? 😒
PPIs are a trap. NSAIDs too. Doctors dont care. They just write scripts. You take it for years then boom kidney gone. No one warned me. Now I need dialysis. Its all corporate greed
It’s wild how we treat meds like they’re vitamins. You wouldn’t take vitamin C for 10 years straight without checking if it’s still helping. But we just keep popping PPIs like they’re mints.
My grandma took omeprazole for 12 years. She never had a kidney test. At 78, her eGFR was 38. She thought it was just "getting old."
We need to stop normalizing chronic drug use. Especially when the side effects are this quiet and deadly.
Been off NSAIDs for 6 months since my biopsy. Took 10 weeks to feel normal again.
Worth it. My creatinine went from 2.1 to 1.0.
Don’t wait till you’re dizzy and swollen. Check your numbers before you take another pill. Seriously. Your kidneys don’t scream. They just… stop.
If you’re on long-term meds, you’re not just a patient-you’re a data point for a drug company.
But you’re also the only one who knows your body. If you feel off, don’t let a doctor dismiss it as "stress" or "aging."
Ask for an eGFR. Ask if your meds could be doing this. Bring a list. Be the squeaky wheel.
Your kidneys can’t yell. But you can. And you should.
How is it possible that a drug class responsible for over 38% of acute kidney injury cases is still sold over-the-counter? This is not a medical oversight. This is a regulatory failure of catastrophic proportions.
Every single PPI on the market should be reclassified as prescription-only. The FDA’s inaction is indefensible. And the fact that people are still taking them daily like candy? Unforgivable.
My dad had AIN from naproxen. Took him 4 months to recover. Now he’s on a 30mg daily prednisone taper.
He still gets tired after walking 2 blocks. His eGFR is 52.
He says he’ll never take NSAIDs again. But he still takes Tylenol like it’s safe.
Guess what? Acetaminophen can cause AIN too. Just… slower.
There’s no safe pill. Just less dangerous ones.
My nephrologist told me if I had waited two more weeks after my creatinine spiked, I’d be on dialysis permanently.
They found AIN from a 3-month course of cipro. No fever. No rash. Just fatigue and weird swelling.
Doctors don’t test for this unless you push.
So push. Bring this article. Ask for a biopsy.
It’s not scary. It’s a 20-minute outpatient procedure. It saved my kidneys.
PPIs are for lazy people who won't change their diet. Now their kidneys are trash. Typical.
For anyone considering steroid treatment: I was prescribed methylprednisolone after my biopsy confirmed PPI-induced AIN.
My eGFR was 28. After 4 weeks of steroids and tapering, it climbed to 55.
Not perfect. But better than 30.
Don’t fear steroids if your kidney function is crashing. They’re not magic-but they’re often the bridge between recovery and permanent damage.
Discuss timing with your nephrologist. Early intervention matters more than you think.
My cousin in Delhi got AIN from a herbal supplement she bought online. "Natural kidney cleanse."
Turned out it had hidden nimesulide. Same as NSAIDs.
She’s 42. Now on dialysis 3x a week.
There’s no such thing as "safe" if it’s not regulated.
Global pharma doesn’t care where you live. They sell the same poison everywhere.
I took omeprazole for 8 years. Got a biopsy. Had AIN. Now my kidneys are garbage. But hey at least my heartburn is gone lol. 🤡
As a nurse practitioner who has managed over 120 patients with drug-induced kidney injury, I can confirm: early recognition saves lives.
Patients who stop the offending agent within 72 hours of symptom onset have a 92% chance of partial or full renal recovery.
Those who delay beyond 14 days? Only 38%.
Education is not optional. It is urgent.
Every primary care provider should be trained to ask: "What medications are you taking? How long? Have you noticed swelling or fatigue?"
It takes 90 seconds. It could save a kidney.
Just got my 1-year eGFR back. 68. Not back to 90, but better than 42.
Still can’t take NSAIDs. Still avoid PPIs.
My doc gave me a letter for my pharmacy: "DO NOT DISPENSE ANY PROTON PUMP INHIBITOR. PATIENT HAS HISTORY OF AIN."
Best thing I ever did.
Don’t trust your pharmacist to remember. Protect yourself.