Every year, thousands of patients in the UK and US are put at risk not because of wrong dosages or allergic reactions, but because two drug names look too similar on a label. Look-alike drug names-like hydroCODONE and hydroHYDRAZINE, or doXEPamine and doBUTamine-cause mix-ups that lead to overdoses, missed treatments, and even deaths. The problem isn’t rare. About 1 in 4 medication errors comes from names that are visually or phonetically confusing. And it’s not just a pharmacy issue-it happens in hospitals, clinics, and even at home when patients misread their own labels.
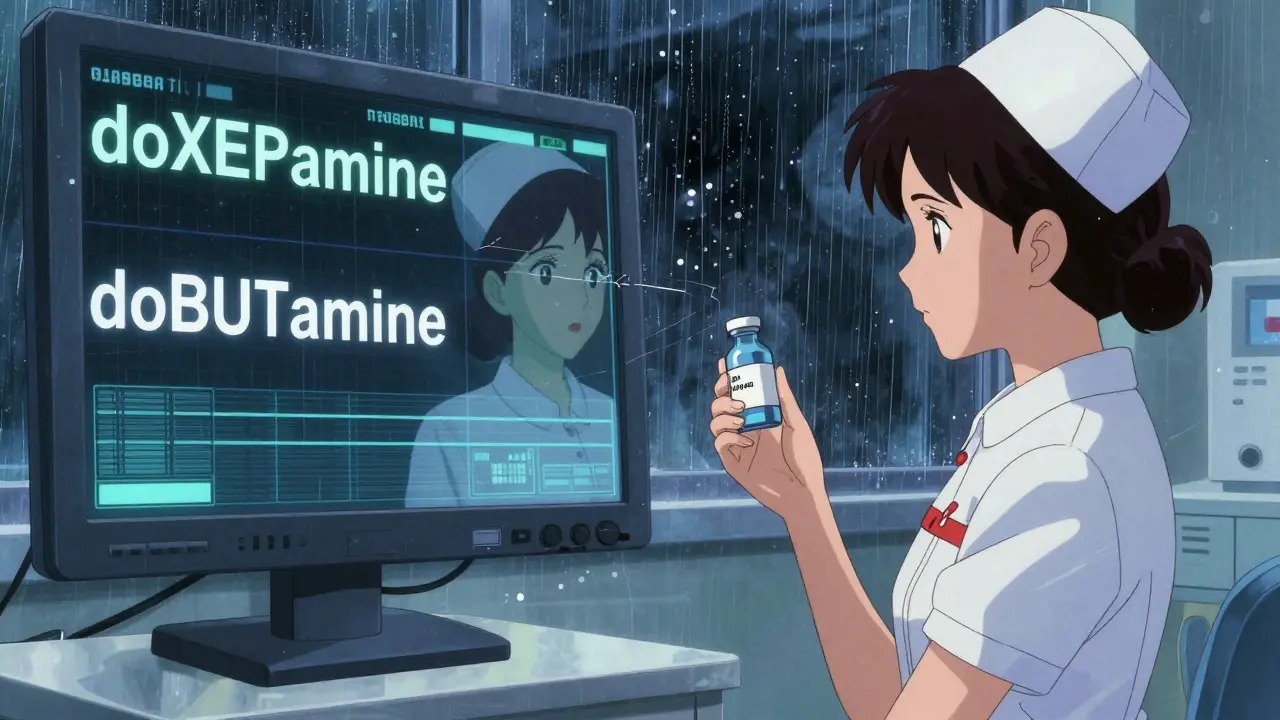
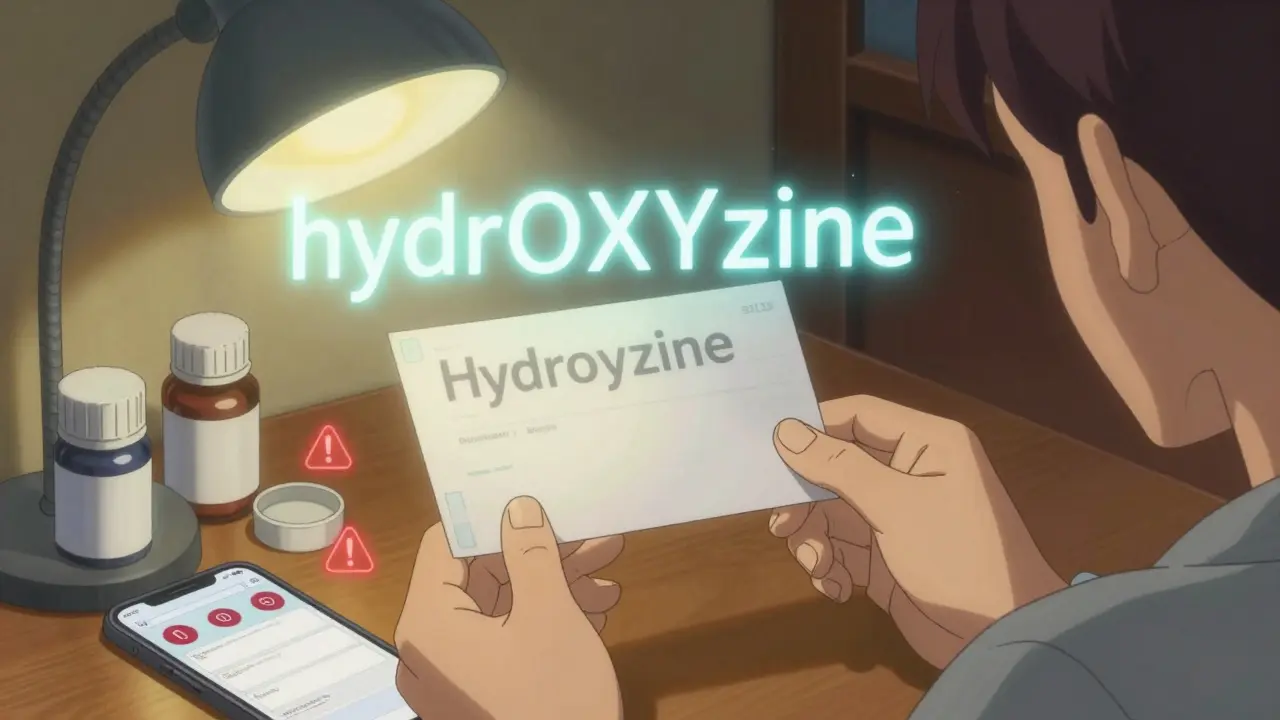
Look-alike and sound-alike (LASA) drug names are medications with spelling or pronunciation that are so similar they can be easily confused. Examples include hydroxyzine and hydralazine, or doxepine and dobutamine. These mix-ups can lead to serious medication errors, even when the correct dosage is given, because the wrong drug is administered.
Tall man lettering uses uppercase letters to highlight the parts of drug names that differ, making visual distinctions clearer. For example, vinBLAstine and vinCRIStine use capitalization to show where the names diverge. This reduces confusion by 32% and is required by the FDA for 35 high-risk drug pairs in electronic and printed labels.
Errors persist because tall man lettering isn’t always applied consistently. Handwritten prescriptions often lack it, printed labels may be too small or faded, and electronic systems sometimes display names differently across platforms. Staff fatigue, time pressure, and alert overload also contribute. It’s not just about the label-it’s about the whole system.
Barcode scanning prevents 86-89% of errors at key points like dispensing and administration. But it doesn’t catch everything. If the wrong drug is scanned in the first place-like if a nurse picks the wrong vial from the shelf-barcodes won’t help. It works best when combined with tall man lettering, training, and double-checking.
Patients should always check the label against their prescription, ask if the drug name has any capitalized letters (tall man lettering), and confirm the reason they’re taking it. If the name looks similar to a previous medication, ask the pharmacist to explain the difference. Never assume the medicine is correct just because it’s in a familiar-looking bottle.
Yes. AI tools like Google’s Med-PaLM 2 can predict confusing drug names with 89% accuracy before they’re approved. Some hospitals are testing smartphone apps with computer vision that can scan pill bottles and flag potential look-alike matches. The FDA now requires all new drug names to be tested using orthographic and phonetic algorithms to prevent future confusion.
I work in a small clinic and we don't even have tall man lettering on our printer. One time I almost gave a patient hydralazine instead of hydroxyzine. Scared the hell out of me. We just started using color-coded stickers now. Small fix, big difference.
OMG I JUST REALIZED MY PHARMACY DOESN'T USE TALL MAN LETTERING ON MY INSULIN LABEL 😱 I ASKED THEM LAST WEEK AND THEY SAID "IT'S JUST HOW IT PRINTS". I'M GOING BACK TOMORROW WITH THIS ARTICLE. THIS ISN'T JUST ANNOYING-IT'S LETHAL.
So we spend millions on AI and barcodes but still rely on nurses squinting at faded labels like they're decoding ancient hieroglyphs? 🤦♂️ We need better systems, not better eyes. Also, why is the FDA only mandating 35 pairs? There are hundreds more that could kill someone.
People need to stop being lazy. If you can't read the label, don't take the pill. It's not the pharmacy's fault you're too tired to look at the whole word. I've seen patients grab morphine thinking it's hydromorphone and then wonder why they passed out. Self-responsibility, people!
This whole thing is a symptom of American healthcare's brokenness. We outsource everything to software and then blame the workers when it fails. The real fix? Hire more pharmacists. Stop cutting staff. No algorithm replaces a human who's not running on 3 hours of sleep.
I'm from India and we don't have the same resources, but we do have something better-community. My aunt is diabetic and her neighbor, who's a retired nurse, checks her labels every time she picks up meds. No tech, no barcode, just someone who cares. Maybe we need more of that, not just more capital letters.
It's funny how we think technology solves human problems. You can put tall man letters on every label, but if the person reading it is stressed, distracted, or just thinks 'it's probably fine'-it doesn't matter. Safety isn't a design feature. It's a habit. And habits take culture, not code.
In my hospital in Mumbai, we use handwritten labels because EHRs are unreliable. But we teach every new nurse to say the drug name out loud twice before handing it over. One says it, the other repeats it. Simple. Human. Works better than any AI. Maybe we should stop importing American tech and start exporting our quiet wisdom.
I used to be a nurse. I saw a patient get the wrong drug because the EHR showed 'doXEPamine' but the MAR printed 'doxepine'. The nurse didn't notice because she was rushing to clock out. We had a 30-second window where someone could have died. And now we're talking about AI? Let's fix the damn workflow first. Tech doesn't fix bad systems. People do.
I just checked my last prescription. No tall man letters. Didn't notice until now.
You know what's wild? The same people who scream about 'big pharma' never complain about the $150k barcode systems hospitals can't afford. We want cheaper drugs but also want every label to be perfect. Pick a side. Or better yet-pay your taxes so the FDA can actually do its job.
The epistemological foundation of pharmaceutical safety is predicated upon the ontological distinction between orthographic fidelity and perceptual cognition. The implementation of tall man lettering constitutes a semiotic intervention intended to mitigate cognitive dissonance induced by lexical similarity. However, its efficacy is contingent upon the structural integrity of the dispensing apparatus and the epistemic vigilance of the operator. In the absence of systemic coherence, isolated orthographic modifications remain epiphenomenal.
If you're a patient and you don't check your meds, you're part of the problem. I don't care if your pharmacist is tired or the printer is broken. If you're too lazy to read the whole name, you deserve what you get. This isn't a tech issue-it's a moral failure.