
Antibiotics can kill probiotics if taken together. To maximize effectiveness, take probiotics 2-3 hours after your antibiotic dose. This spacing allows antibiotics to work without destroying beneficial bacteria.
Important: Take probiotics 2-3 hours after your antibiotic dose for best results. Continue taking probiotics for at least 1-2 weeks after finishing antibiotics.
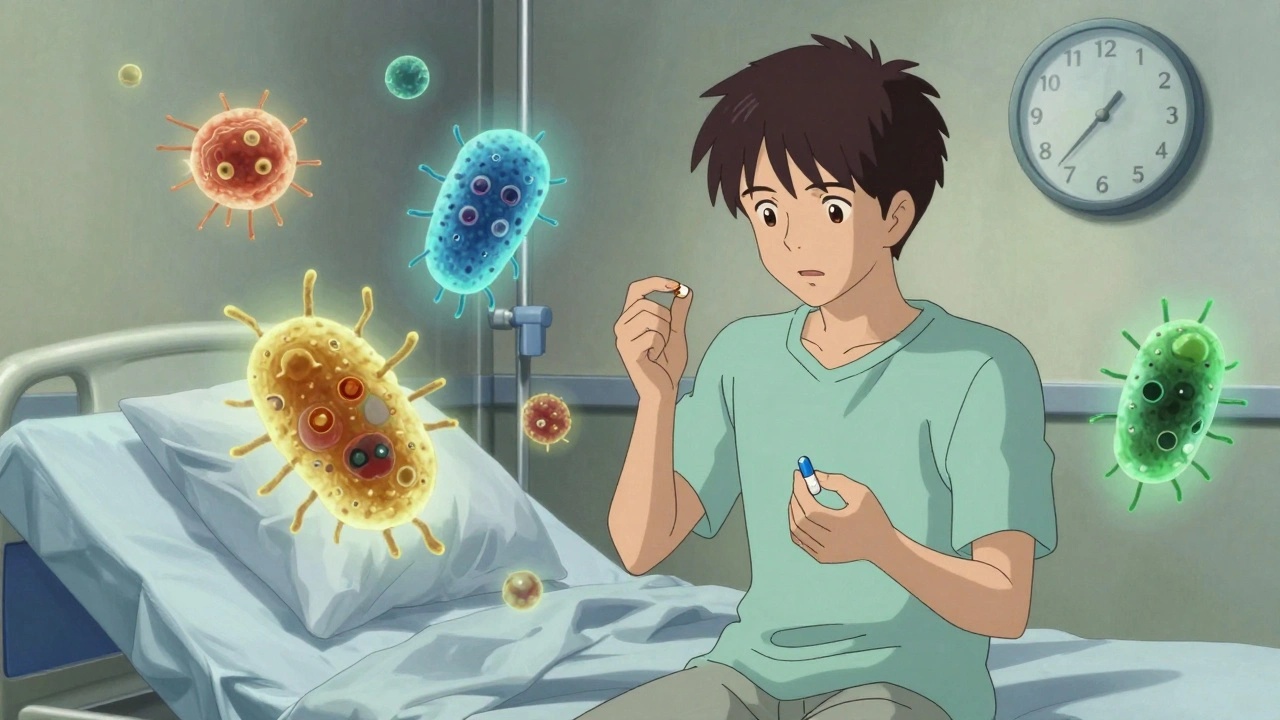
When you’re on antibiotics, you might expect to feel better - but instead, you get stomach cramps, bloating, or worse, watery diarrhea. It’s not just bad luck. Antibiotics don’t just kill the bad bacteria; they wipe out the good ones too. And that’s where your gut pays the price. About one in five people on antibiotics end up with antibiotic-associated diarrhea. For some, it’s mild. For others, it’s a dangerous infection like Clostridioides difficile - a serious gut bug that can land you in the hospital.
Multi-strain products make up 40% of the market, but don’t assume more strains = better. Some combinations haven’t been tested. Stick to the ones with real data behind them.
Don’t wait until diarrhea starts. Start the probiotic on day one of your antibiotic course. Prevention works better than repair.
These aren’t signs it’s not working - they’re signs your gut is adjusting. Your body’s been through a microbial war. The new bacteria are settling in, and they’re producing gases as they eat. Most people feel better within 3 to 5 days. If symptoms last longer or get worse, stop and talk to your doctor.
People with IBS or sensitive guts sometimes report flare-ups. That doesn’t mean probiotics are bad - it means you might need a different strain or lower dose. Try reducing to 1-2 billion CFUs and see how you respond.
These risks are rare, but real. And they’re often overlooked because probiotics are sold as supplements - not medicine. That means no FDA review. No safety testing required before they hit the shelf.
Popular brands like Culturelle (L. GG) and Florastor (S. boulardii) have strong consumer reviews and clinical backing. Amazon ratings are helpful, but don’t trust them blindly. Look for reviews that mention “prevented diarrhea while on antibiotics” - those are the most reliable.

Probiotics aren’t a cure-all. But for most people, they’re one of the few proven ways to avoid the worst part of antibiotic treatment: a ruined gut.
It’s not recommended. Antibiotics can kill the live bacteria in probiotics if taken together. To avoid this, wait 2 to 3 hours after your antibiotic dose before taking your probiotic. This gives the antibiotic time to work without interfering with the beneficial microbes.
No. Only certain strains have been proven effective. The strongest evidence supports Lactobacillus rhamnosus GG and Saccharomyces boulardii. Many multi-strain products and generic brands lack clinical proof. Always check the label for the exact strain name and CFU count.
Continue for at least 1 to 2 weeks after finishing your antibiotic course. Your gut microbiome takes time to recover. Stopping too soon may leave you vulnerable to diarrhea or reinfection. Some experts recommend continuing for up to 4 weeks, especially if you had severe side effects.
Yes, for most children and healthy older adults. L. rhamnosus GG is even approved for use in kids to prevent antibiotic diarrhea. But older adults with weakened immune systems, chronic illness, or recent surgery should talk to their doctor first. The same safety warnings apply: avoid probiotics if you’re immunocompromised.
Rarely, but yes. There have been documented cases of probiotic strains entering the bloodstream and causing sepsis, especially in people with weakened immune systems, central lines, or recent surgery. These events are extremely uncommon in healthy people, but if you have any immune-related condition, always consult your doctor before starting.
In the U.S., probiotics are sold as dietary supplements under the DSHEA law. That means manufacturers don’t have to prove they work or are safe before selling them. The FDA only steps in if a product is found to be harmful after it’s on the market. This creates a wild west of quality - some products are excellent, others contain nothing but filler. Always look for third-party testing seals like USP or NSF.
No. While yogurt contains beneficial bacteria, it typically has far fewer live organisms than a probiotic supplement - often under 1 billion CFUs per serving. You’d need to eat multiple cups daily to reach the dose shown to be effective in studies. Yogurt is good for general gut health, but for preventing antibiotic side effects, a targeted supplement is more reliable.
Let’s be clear: the Cochrane review is the gold standard, and its 70% reduction in C. diff incidence isn’t just statistically significant-it’s clinically transformative. Most people treat probiotics like dietary candy, but this isn’t about ‘boosting immunity’; it’s about ecological restoration. L. rhamnosus GG and S. boulardii aren’t just ‘good strains’-they’re the only ones with replicated, double-blind, placebo-controlled validation. Everything else is marketing dressed as science.
India has been using fermented foods for 5,000 years-why are we now importing expensive Western supplements? Curd, kanji, idli batter-they’re all probiotics! You don’t need a $30 bottle from Amazon when your grandmother’s kitchen had better microbiome wisdom. This whole ‘CFU count’ obsession is colonial nonsense.
Probiotics are just the gut’s way of saying ‘I need a new roommate after the antibiotic eviction.’
Of course you’re going to get diarrhea. You took antibiotics like candy and now you want a magic pill to fix it? You didn’t think this through. Your gut isn’t a broken phone-you can’t just download a patch. Stop looking for shortcuts and start respecting your biology.
For anyone considering probiotics during antibiotics: timing is everything. Taking them too close to your antibiotic dose renders them useless. I’ve seen patients waste hundreds on products that never had a chance. Stick to 2–3 hours post-dose. And yes-refrigerated is better, but if you can’t get it, look for enteric-coated capsules. They survive stomach acid. Also: check expiration dates. Many brands list CFUs at manufacture, not at use. That’s misleading.
Thank you for this incredibly thorough and well-researched breakdown. As someone who’s spent years managing chronic GI issues, I can say with confidence that the distinction between strain-specific efficacy and generic ‘probiotic’ claims is absolutely critical. I’ve tried dozens of products, and only two-Culturelle and Florastor-made a measurable difference. The rest? Just sugar and starch with fancy labels. I’m glad to see science finally catching up to what patients have known anecdotally for years.
probiotics? more like probi-who? i mean, i took amoxi and just ate a ton of kimchi and i was fine? maybe the real fix is just not being a hypochondriac? also, who even uses CFUs? sounds like a sci-fi unit
Wait so you’re telling me I can’t just chug yogurt and call it a day? I already spent $20 on that fancy kefir. Now you want me to buy another bottle? This is ridiculous. I’m just gonna skip it and hope I don’t poop my pants. Seriously, why is everything so complicated now?
There’s a quiet poetry in this, isn’t there? We’ve spent centuries trying to conquer microbes-through antibiotics, sterilization, fear-and now we’re learning to coexist. The gut isn’t a battlefield; it’s a symphony. Antibiotics are the conductor who forgot the score. Probiotics? They’re the musicians who quietly return, note by note, to restore the harmony. We don’t need to dominate nature-we need to listen to it.
So… you’re saying I should spend $30 on a pill that might not even work, just to avoid diarrhea? Meanwhile, I could’ve just stayed home for a week and avoided antibiotics altogether. Who even needs to take antibiotics in the first place? This whole system is a scam. Big Pharma, big probiotic, same playbook. I’m not falling for it.
Hey, I just wanted to say thanks for writing this. I’m a dad with two kids on antibiotics right now, and I was so lost. I read all the labels, but I didn’t know what to pick. Your breakdown on L. rhamnosus GG and spacing the doses? Lifesaver. My 6-year-old didn’t get a single stomach ache. And yeah, I bought the refrigerated Culturelle-even though it cost more. Worth every penny. You saved us from a week of misery. Seriously, thank you.
What fascinates me isn’t just the strain specificity-it’s the emerging data on microbiome resilience. A 2023 NIH study found that certain probiotics may actually delay native microbiota recovery by suppressing the gut’s own regenerative signals. That’s why blanket recommendations are fading. The future isn’t ‘take probiotics’-it’s ‘take the right probiotic, at the right time, for your unique microbial fingerprint.’ Imagine a future where your gut microbiome is sequenced before antibiotics, and your probiotic is custom-tailored. We’re not just restoring balance-we’re becoming co-authors of our own internal ecosystems.