
This calculator helps determine your risk of having G6PD deficiency based on your ethnic background and gender. G6PD deficiency can cause severe hemolytic anemia when taking nitrofurantoin and other oxidizing drugs.
Enter your information to see your risk level
Take a simple urinary tract infection (UTI). It’s common, treatable, and for most people, nitrofurantoin works fast and well. But for some, that same pill can trigger a life-threatening reaction - not because of an allergy, but because of a hidden genetic condition most never know they have: G6PD deficiency.
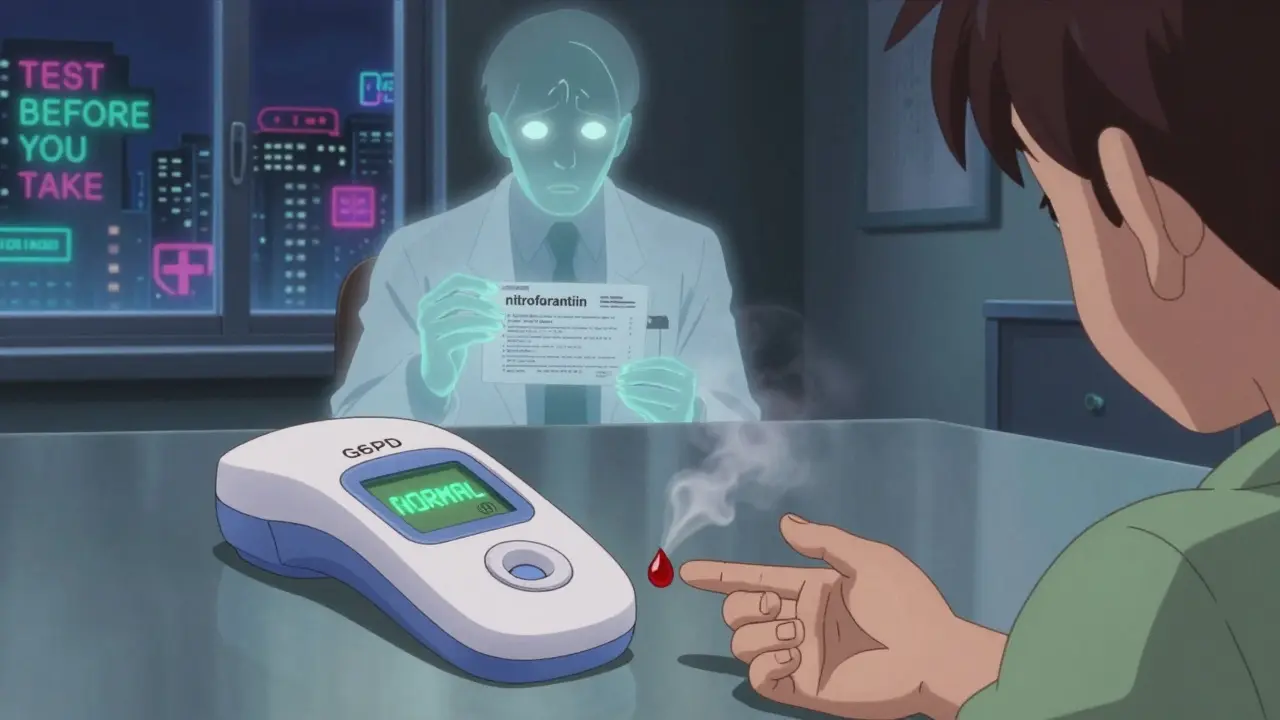
Yes. About 50-60% of people with G6PD deficiency are undiagnosed until they take a drug like nitrofurantoin. The first sign of deficiency might be a sudden drop in hemoglobin, dark urine, or jaundice after starting the antibiotic. There’s no warning - it happens fast.
No. A standard G6PD blood test costs $35-$50 in the U.S. and is often covered by insurance. Many clinics offer rapid point-of-care tests that give results in under 10 minutes. You can get tested during a routine visit - no special appointment needed.
No. Once you’ve had a reaction, or even if you’re diagnosed with G6PD deficiency, you should avoid nitrofurantoin for life. Even small doses can trigger another episode. There are many other antibiotics for UTIs that are just as effective and completely safe.
Yes. Other oxidizing drugs include sulfonamides (like Bactrim), dapsone, primaquine, and methylene blue. Always check with your doctor or pharmacist before taking any new medication. Even some over-the-counter pain relievers like aspirin can pose a risk in high doses.
Yes. G6PD deficiency is an X-linked genetic condition. If you’re male and have it, you’ll pass the gene to all your daughters (who become carriers) but not your sons. If you’re female and carry the gene, each son has a 50% chance of inheriting it, and each daughter has a 50% chance of being a carrier. Testing your children is recommended if you or your partner are from a high-risk population.
Because guidelines aren’t always enforced. Many doctors rely on habit, not data. Nitrofurantoin is cheap, widely available, and works well - so it’s easy to default to. But when the cost of a $50 test prevents a $10,000 hospital stay, skipping it is a false economy. Awareness is growing, but change is slow.
Just got prescribed this for my UTI yesterday 😳 I’m Black American and had no idea about G6PD. I’m calling my doc first thing tomorrow to get tested. Thanks for posting this-could’ve been a nightmare.
My mom had a bad reaction to nitrofurantoin back in the 90s. They didn’t test her either. She ended up in the ER with jaundice and was so weak she couldn’t walk for weeks. Still sucks to think it was preventable.
It’s not just about testing-it’s about doctors taking responsibility. If you’re prescribing a drug with a known risk, you should be required to check. This isn’t ‘maybe’-it’s a documented danger. Stop being lazy.
Everyone’s acting like this is some new revelation. It’s been in the FDA label since the 80s. People just don’t read. Also, why are we acting like G6PD is some exotic condition? It’s common. Stop acting surprised.
As someone from a South Asian background, I never knew I had G6PD deficiency until I got sick after a course of Bactrim. I was 28. I wish I’d been tested as a child. The point-of-care tests are a game-changer. Hospitals should make them standard for UTI prescriptions, especially in diverse populations. It’s not just cost-it’s care. And yes, I typo’d ‘care’ on purpose because I’m tired of perfectionism masking neglect.
Think about it: we live in a world where we can sequence your genome from a spit sample, but we still hand out antibiotics like candy. Nitrofurantoin isn’t the villain. It’s the system. The system that treats medicine like a checklist, not a relationship between human biology and human care. We’re not just treating infections-we’re negotiating with evolution. And sometimes, evolution wins. And it doesn’t ask permission.
India has over 100 million people with G6PD deficiency. Why does the US act like it’s a mystery? We’ve had rapid tests in rural clinics since 2015. Doctors here still give nitrofurantoin to kids without testing. It’s not ignorance-it’s neglect. And it’s killing people.
My cousin in Delhi got sick after taking nitrofurantoin for a UTI. She was fine until day two-then her eyes turned yellow. Took her 3 days to recover. We got her tested after. Turned out she had mild deficiency. Now every family member got tested. Cheap. Easy. Don’t wait for a crisis. Just do it.
They’re hiding something. Why is G6PD testing not mandatory? Why is nitrofurantoin still on the WHO list? Big Pharma knows most people won’t get tested. They profit from hospitalizations. The CDC knows this. The FDA knows this. This isn’t negligence-it’s business. And the next time you get a UTI, ask yourself: who really benefits if you get sick?
