
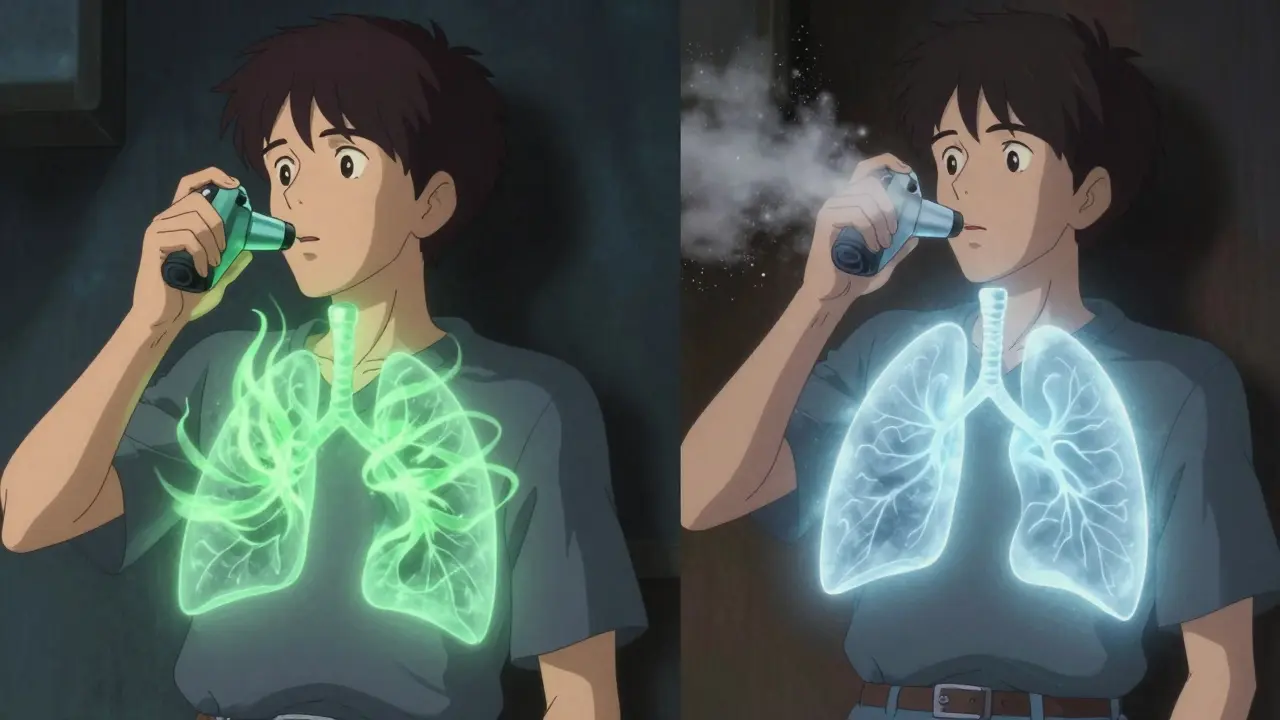
Switching from a branded respiratory inhaler to a generic version might seem like a simple cost-saving move-until it isn’t. For millions of people with asthma or COPD, the device you use to breathe in your medication isn’t just a container. It’s part of the treatment. And when that device changes, even if the drugs inside are the same, your lungs might not get what they need.
There are two main types of inhalers: pressurized metered-dose inhalers (pMDIs) and dry powder inhalers (DPIs). pMDIs require you to press the canister and breathe in slowly at the same time. DPIs? You need to take a sharp, deep breath to pull the powder out. If you get the timing wrong, or breathe too lightly, most of the medicine stays in your mouth or throat. That means less reaches your lungs, and your symptoms don’t improve.
Generic versions often come in different devices than the original. For example, Symbicort Turbohaler uses a twisting motion to load each dose. Its generic alternative, DuoResp Spiromax, uses a side slider. Sounds minor? It’s not. A 2020 study found that 76% of patients switched to Spiromax without training used it incorrectly. That’s not because they were careless-it’s because the device felt unfamiliar.
In the UK, the National Institute for Health and Care Excellence (NICE) warns that switching inhaler devices without a consultation can lead to worse asthma control. A 2021 study showed patients switched from Symbicort Turbohaler to Spiromax without training had a 22% increase in asthma exacerbations within six months. That’s not a small uptick-it’s a clear risk.
On Drugs.com, users gave Symbicort Turbohaler a 6.2 out of 10. The generic Spiromax? Only 4.8. Common complaints? “Harder to use,” “feels less effective,” “I didn’t know I had to breathe harder.” One patient wrote: “I ended up in hospital because I didn’t realize the new inhaler needed a different technique.”
A survey of 1,247 people by Asthma UK found that 57% felt confused after being switched to a different device. One in three had visited an emergency department within three months. That’s not just bad for patients-it’s bad for the system. A 2023 report estimated that inappropriate inhaler substitutions cost healthcare systems $1.2 billion a year in avoidable hospitalizations.
In Europe, the European Medicines Agency (EMA) takes a stricter approach. They require proof that the generic works just as well as the original-not just in labs, but in actual patients. That means comparing lung deposition, clinical outcomes, and even patient-reported symptoms. Even then, they don’t assume automatic substitution is safe.
The UK and many European countries now recommend prescribing inhalers by brand name-not by generic drug name-so patients don’t get switched without warning. The European Respiratory Society’s 2023 guidelines say clearly: “Inhaled medications should be prescribed by brand name with specific device instructions to prevent substitution errors.”
The U.S. is starting to catch on. In May 2023, the FDA issued a draft guidance asking manufacturers to prove therapeutic equivalence through clinical studies-not just chemical tests. That’s a big shift. It means regulators are finally recognizing that device matters.
When you switch devices, that number drops even lower. The American Association for Respiratory Care recommends the “teach-back” method: you show your provider how you use it, and they correct you right then. That method boosts correct technique from 35% to 82%.
But in most community pharmacies in the U.S., only 28% consistently offer device training when switching inhalers. Why? Time. Pharmacists are busy. Training takes 10 to 15 minutes. Most don’t have it.
Meanwhile, general practitioners need nearly 13 minutes of training just to learn how to demonstrate both Turbuhaler and Spiromax correctly. If your doctor doesn’t know how to use the new device, how can they teach you?

Don’t assume it’s the same. Even if the name on the box says “budesonide/formoterol,” the device could be completely different. If you’re not shown how to use it properly, ask for a referral to a respiratory nurse or pharmacist who specializes in inhaler technique.
And if you feel worse after the switch-more wheezing, more puffs needed, more nighttime symptoms-don’t brush it off. Go back. Say: “This new inhaler isn’t working like the old one.” That’s not complaining. That’s being your own best advocate.
But there’s hope. Smart inhalers with sensors that track how you use them are becoming more common. One study showed that when patients got real-time feedback on their technique, asthma exacerbations dropped by 33%. These devices can catch mistakes before they lead to hospital visits.
The FDA has also allocated $25 million to research best practices for inhaler substitution. That money is going toward training programs, device comparisons, and patient education tools. It’s a start.
For now, the message is clear: generic doesn’t mean interchangeable. The device is part of the medicine. And if you’re switching, you need to know how to use the new one-or your lungs will pay the price.
No, you shouldn’t. Generic inhalers often come in different devices, and using them incorrectly can reduce how well your medicine works. Even if the drug is the same, the way you breathe in might need to change. Always talk to your doctor or pharmacist before switching.
It’s usually not because the medicine is weaker-it’s because the device is different. For example, switching from a Turbuhaler to a Spiromax means you now have to slide a lever instead of twist the base. If you don’t learn the new technique, you won’t get the full dose. Many patients report feeling like it’s “less effective,” but they’re actually just using it wrong.
Yes, they’re cheaper-sometimes by 50% or more. But if the switch leads to more asthma attacks, emergency visits, or hospital stays, the cost savings disappear. A 2023 report found that bad substitutions cost healthcare systems $1.2 billion a year. For you, the risk isn’t just money-it’s your breathing.
Ask for a “teach-back” session. Your provider shows you how to use it, then asks you to demonstrate it back to them. If you can do it right the first time, great. If not, they correct you. Studies show this method improves technique from 35% to 82%. You can also ask for a video or printed guide. Never assume you’re doing it right-most people aren’t.
Contact your doctor or asthma nurse immediately. Don’t wait. Bring your new inhaler with you. Say clearly: “I’ve been using this new one, and my symptoms have gotten worse.” They may switch you back or give you proper training. Many people don’t realize their worsening symptoms are due to device confusion-not their disease getting worse.
So many people think generic = same, but inhalers aren’t pills. You can’t just swap a wrench for a screwdriver and expect the engine to run the same. The device is the delivery system-mess that up, and you’re basically breathing in air with a side of medicine.
I’ve seen patients switch and then show up in the ER wheezing like a broken bellows, convinced their asthma got worse. Nope. They just didn’t know how to use the new one. No training. No demo. Just a box and a shrug.
It’s not the drug’s fault. It’s the system’s. Pharmacies are cash registers with stethoscopes. They’re not equipped to teach technique. Doctors don’t have time. And patients? They assume they’re doing it right because they’ve used one before.
Teach-back isn’t optional. It’s survival. If your provider doesn’t ask you to demonstrate, ask them why. And if they look confused? That’s your sign to find someone who actually knows how the damn thing works.
My cousin switched to a generic and started coughing all night. Thought it was the allergy season. Turned out she was puffing like she was trying to blow out birthday candles. Didn’t even know she had to breathe HARD.
Took her to a respiratory nurse, showed her the difference-twist vs. slide-and within a week she was sleeping again. No drama. No panic. Just someone who knew how to use the tool.
If you’re switching, don’t just take it. Ask for a demo. Right then. In the pharmacy. If they say no, walk out and call your doctor. Your lungs don’t care about cost savings.
Let’s cut through the pseudoscience. The FDA doesn’t care about your breathing technique. They care about molecular equivalence. If the active ingredient is the same, legally, it’s interchangeable. The fact that patients mess up the device is a behavioral problem, not a regulatory one.
Stop treating inhalers like magic wands. People can’t tie their shoes properly-why should we expect them to master a complex inhaler without training? That’s not the manufacturer’s fault. It’s not the doctor’s. It’s society’s failure to teach basic health literacy.
And yes, the 22% increase in exacerbations? Correlation isn’t causation. Maybe those patients were noncompliant before. Maybe they stopped taking it. Maybe they started smoking again. But no, let’s blame the generic. Classic victim-blaming wrapped in medical jargon.
Interesting how the US pushes for interchangeability while Europe treats this like a life-or-death matter. But then again, the UK has a national health system that can afford to care about long-term outcomes. Here? We optimize for the next quarter’s profit margins.
That $1.2 billion cost? That’s not a statistic. That’s 1.2 billion reasons why American healthcare is broken. We reward volume over value. We incentivize substitution over safety. And we wonder why people end up in ICU because they were given a device they couldn’t operate.
It’s not a failure of the patient. It’s a failure of the system that treats lungs like they’re disposable.
They’re lying. The generics are weaker. I’ve used both. The new one doesn’t hit the same. I can feel it. And don’t tell me it’s technique-my technique hasn’t changed. I’ve used inhalers since I was 8. This one feels… hollow. Like it’s just air with a fancy label.
They’re cutting corners. And you’re all pretending it’s fine because the price is lower. But your lungs aren’t cheap. They’re not replaceable. You think the FDA cares? They’re on the payroll.
I switched last year and was terrified. I thought I was going to suffocate. But my pharmacist sat with me for 12 minutes. Showed me the slide, had me mimic it three times, even gave me a QR code to watch a video later.
It’s not hard. It just takes a second. And that second saved me. I’m not some medical expert-I’m a teacher who forgets to take her meds on Tuesdays. But I know how to use my inhaler now.
Ask for help. Seriously. No one’s gonna judge you. We’ve all been there.
My dad’s COPD got worse after his switch. We thought it was progression. Turned out he was using the new one like the old one-twisting instead of sliding. He didn’t realize it was different.
My sister printed out a comparison chart. We sat down, watched the video, and he practiced with a placebo device for a week. Now he’s stable again.
It’s not about the brand. It’s about the instruction. If your pharmacy doesn’t offer that, find one that does. Or call your clinic. Someone will help. They just need to be asked.
Oh, so now we’re pretending that Americans can’t handle complexity? We can’t use a sliding inhaler but we can stream 4K on our phones and navigate GPS through 17 states? Please.
This isn’t a device issue. It’s a cultural one. We’ve been conditioned to expect everything to be effortless. You don’t read the manual. You don’t ask questions. You just swipe and expect magic.
And now we’re blaming the FDA because your inhaler didn’t come with a TikTok tutorial? Grow up.
Meanwhile, in the UK, they teach inhaler technique in school. We teach kids how to use a vape. Which society is more responsible? Exactly.
I got switched last month. Thought I was fine. Then I started waking up gasping. Thought I was dying. Went to urgent care. Nurse asked me to show her how I use it. I did. She said, ‘You’re not inhaling deep enough.’ Turns out the new one needs a sharp breath. I was puffing like I was blowing a balloon.
She showed me. I practiced. I’m good now. No drama. No panic. Just… a little education.
Don’t be like me. Ask. Even if you think you know. You don’t.
The argument that generic inhalers are interchangeable ignores the fundamental principle of pharmacokinetics: delivery method alters bioavailability. Even with identical active ingredients, the particle size distribution, aerosol velocity, and oropharyngeal deposition differ significantly between devices.
Regulatory bodies that equate chemical equivalence with therapeutic equivalence are operating under a 20th-century paradigm. The 21st century demands evidence of clinical equivalence-not just in vitro, but in vivo, under real-world conditions.
It is not unreasonable to require manufacturers to demonstrate equivalence in patient outcomes before labeling a product as interchangeable. The science is clear. The policy is lagging.
USA thinks money is more important than breathing. Nigeria? We don’t have generics because we can’t afford the originals. We pray. We use herbs. We walk miles for a doctor who might have one inhaler left.
And you’re arguing about whether sliding or twisting matters? You people have no idea what real scarcity looks like.
Maybe if you spent less time arguing about devices and more time making sure people have ANY inhaler at all, we wouldn’t be having this conversation.
Also, your FDA is corrupt. I know people who work there. They take bribes from Big Pharma to approve junk. Don’t believe the propaganda.
❤️
So let me get this straight: the solution to a $1.2 billion problem is… more paperwork?
Instead of fixing the system-like, I don’t know, paying pharmacists to train patients-we just make them fill out a form that says ‘I showed the patient how to use it.’
And we wonder why people hate healthcare.
It’s like trying to fix a leaking roof by giving the tenant a pamphlet titled ‘How to Hold an Umbrella.’
Also, the FDA’s $25 million? Cute. That’s less than what they spent on a single celebrity endorsement last year.
Wait… so the FDA is finally admitting they were wrong? After 20 years of ignoring patient reports? After thousands of ER visits? After billions spent on avoidable hospitalizations?
And now they’re ‘allocating’ $25 million? That’s less than the cost of one corporate jet.
Who really controls the FDA? Who profits from these switches? Who benefits when people can’t breathe?
And why is no one asking why the SAME drug, in the SAME dose, suddenly becomes ‘ineffective’ the moment the device changes?
It’s not coincidence. It’s control. It’s profit. It’s manipulation.
And they’re still letting you switch without training.
Wake up.
They’re not saving you money.
They’re saving themselves.
You’re all wrong. The new one doesn’t work. Period. I’ve used both. I know my body. I know my technique. It’s the drug. They cut the dose. They changed the filler. It’s all the same lie.
Don’t trust the system. They’re lying to you.