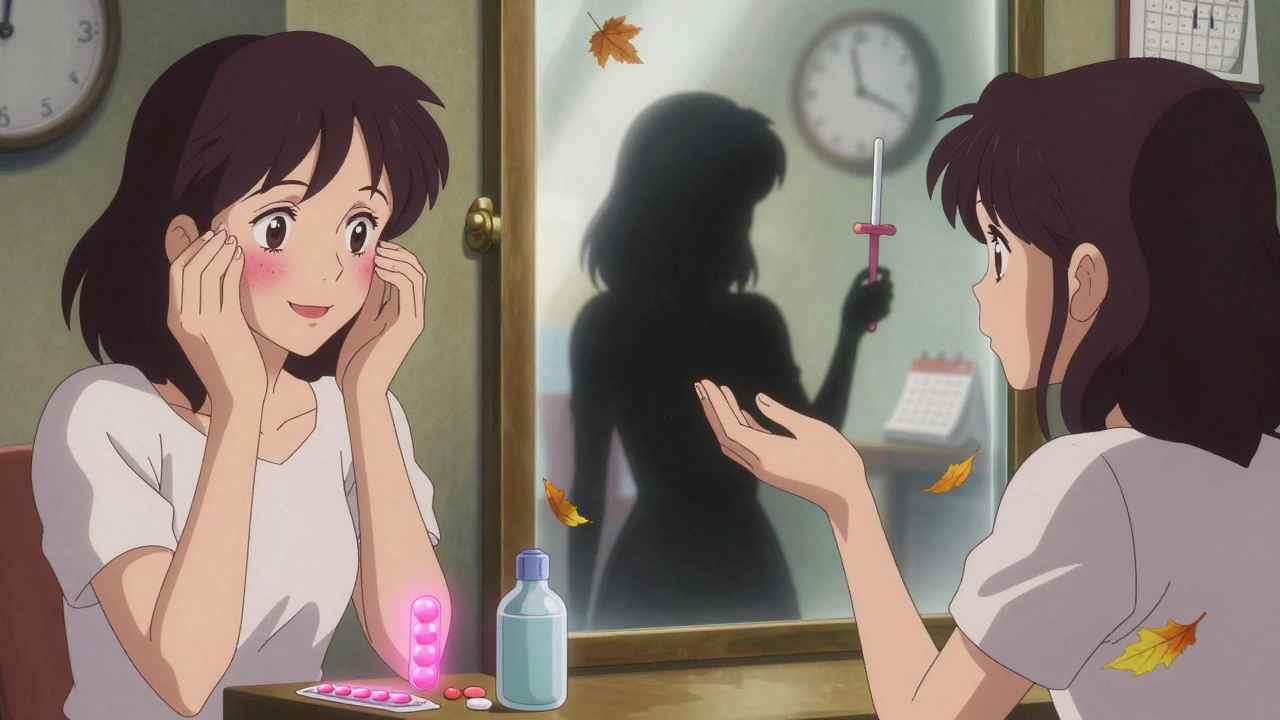
Birth control pills are one of the most common ways women prevent pregnancy-but they’re not as simple as popping a pill every day and forgetting about it. Many people assume the pill is 99% effective, but that number only applies if you take it at the same time, every single day, without missing a single dose. In real life, that’s harder than it sounds. For most users, the actual effectiveness drops to about 93%, meaning 7 out of every 100 women using the pill will get pregnant in a year-not because the pill doesn’t work, but because life happens. Missed doses, late pills, or interactions with other meds can undo its protection.

Most modern birth control pills don’t cause significant weight gain. Any increase is usually temporary water retention, not fat. Studies comparing users and non-users show no consistent difference in body weight over time. If you notice persistent weight gain, it might be due to other factors like diet, stress, or an underlying condition-not the pill itself.
Yes. If you start the pill on any day other than the first day of your period, you should use condoms or avoid sex for the first 7 days. Even if you start on day one, some providers still recommend backup for the first week as a safety measure. The pill takes time to build up hormone levels in your system to fully suppress ovulation.
If you miss one pill, take it as soon as you remember-even if that means taking two pills in one day. If you miss two or more, take the most recent missed pill and skip the others. Use backup contraception (like condoms) for the next 7 days. If you had unprotected sex in the past 5 days, consider emergency contraception. For progestin-only pills, the window is tighter: if you’re more than 3 hours late, take it as soon as possible and use backup for 48 hours.
Combined pills (with estrogen) are not recommended in the first 6 weeks after birth because estrogen can reduce milk supply. After that, they’re usually safe if breastfeeding is well established. Progestin-only pills (mini-pills) are the preferred choice for nursing mothers, as they don’t affect milk production and are safe from day one.
No. Birth control pills only prevent pregnancy. They offer zero protection against sexually transmitted infections like chlamydia, gonorrhea, HIV, or HPV. If you’re not in a mutually monogamous relationship, always use condoms alongside the pill.
If you start on the first day of your period, you’re protected immediately. If you start later, it takes up to 7 days for the pill to become fully effective. During that time, use another method like condoms. For progestin-only pills, protection begins after 48 hours, but you need to take them at the same time every day without delay.
Yes. Four FDA-approved birth control pills for acne treatment are: Ortho Tri-Cyclen, Estrostep, Beyaz, and Yaz. They contain a mix of estrogen and progestin (like drospirenone or norgestimate) that reduce oil production and inflammation. These pills are often prescribed for women 14 and older who want both contraception and clearer skin.
Yes. Most pill packs have placebo pills to trigger a withdrawal bleed. You can skip them and start a new pack right away. This is safe and commonly done for medical reasons (like endometriosis) or personal preference. Some extended-cycle pills like Seasonale or Lybrel are designed specifically for fewer or no periods per year.
I took the pill for years and never had an issue until I started taking turmeric supplements. Didn't realize it could interfere until I got pregnant. Lesson learned: always check with your pharmacist. Even 'natural' stuff can mess with hormones.
The real issue isn't the pill-it's the system that makes you responsible for a biological process while ignoring your life circumstances. Why should a 19-year-old student be penalized for missing a pill because they were working two jobs and sleeping four hours a night? Contraception should be about access, not perfection.
I once took my pill at 3am because I was drunk and then forgot the next day. Got pregnant. Not the pill’s fault. My bad. 🤦♂️
I stopped the pill and my skin cleared up. Took 6 months. No one tells you that.
I’ve been on the same pill for 12 years and I’ve never missed a day. I set a reminder for 8pm every night like clockwork. But I also know people who forget because they’re dealing with depression or chronic pain or just life. The 7% failure rate isn’t about laziness-it’s about how little support we give people to manage their health in a world that doesn’t stop for anyone. We need better systems, not just better reminders.
So let me get this straight. You’re telling me I can’t trust my body to not get pregnant unless I’m a robot who takes a pill at the exact same minute every day? And if I’m not? I’m just dumb. Right. Because clearly the solution is more discipline, not better options.
The statistical failure rate is misleading. The true failure rate is 100% for individuals who do not adhere to the protocol. This is not a medical issue-it is a behavioral one. The pill is a tool, not a guarantee. Those who fail are not victims of biology; they are victims of inconsistency. Discipline is not optional in reproductive health.
Bro I took the mini pill while breastfeeding and my milk dried up. Everyone says it’s fine but my body said no. I switched to the copper IUD and now I’m chill. Don’t just trust the internet.
I started the pill for acne and ended up with anxiety so bad I couldn’t leave my apartment. My doctor said it was 'probably coincidence.' I said no, it’s the pill. She shrugged. Took me 8 months to find a doctor who listened. Don’t let them gaslight you.
You say IUDs are better? Cool. IUDs cost $1000 upfront. Pills are $15 a month. Who are you to tell someone on minimum wage to 'just get an IUD'? Your privilege is showing.
I’ve been on the pill for 8 years. My period is lighter, my skin is better, and I’ve never had a scare. I’m not a robot, I just use the app. If you can’t manage a daily pill, maybe you shouldn’t be on it. Simple.
I used to forget my pill all the time until I started keeping it next to my toothbrush. Now I never miss. Small habits > big pressure. 🌱
The pill is like a really good playlist-works wonders if you’re in the right headspace. But if you’re drowning in chaos, even the best song won’t save you. That’s why I switched to the implant. No thinking. No reminders. Just vibes. And now I can sleep through the night without worrying if I took it.
The notion that hormonal contraception is a panacea for reproductive autonomy is fundamentally flawed. The pharmacological suppression of endogenous physiological processes constitutes a form of medicalized control, predicated upon the assumption of female compliance as a precondition for bodily sovereignty. The discourse surrounding efficacy must therefore be reframed as a sociopolitical inquiry into structural accessibility, rather than an individualized moral calculus.