Every year, over 36 million older adults in the U.S. fall - and for many, the cause isn’t just slippery floors or poor lighting. It’s something sitting in their medicine cabinet: sedating antihistamines. Drugs like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine are still widely used by older adults for allergies, colds, or even sleep. But the risks? They’re real, serious, and often ignored.
Why These Medications Are Dangerous for Older Adults
First-generation antihistamines were designed decades ago to block histamine and relieve allergy symptoms. But unlike modern alternatives, they don’t stop at the nose or throat. They cross the blood-brain barrier, hitting the central nervous system hard. This causes drowsiness, dizziness, slowed reaction times, and poor balance - all of which directly increase the chance of falling.
In older adults, these effects are worse. As people age, their liver and kidneys don’t process drugs as quickly. Diphenhydramine, for example, has a half-life of about 8.5 hours in healthy adults, but in someone over 65, it can linger for over 13 hours. That means if someone takes it at night, they’re still feeling foggy the next morning - when they’re most likely to get up, walk to the bathroom, or step off a curb.
A 2025 study tracking nearly 200,000 older adults found that 32% of those who filled a prescription for a vestibular suppressant - a category that includes these antihistamines - had a fall requiring medical care within 60 days. The risk didn’t stop there. Another analysis showed first-generation antihistamines increase the risk of injurious falls by 54% and fractures by 43%.
The American Geriatric Society has labeled these drugs as “potentially inappropriate” for older adults in their Beers Criteria. Why? Because they don’t just cause falls. They also trigger confusion, memory problems, dry mouth, constipation, and even delirium during hospital stays. One study found older adults on these meds were 2.3 times more likely to develop delirium in the hospital - a condition that often leads to longer stays and more falls.
Second-Generation Antihistamines: A Safer Choice?
Not all antihistamines are created equal. Second-generation options like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were developed to avoid the brain. They’re designed to stay outside the central nervous system, which means far less drowsiness and dizziness.
The numbers tell the story:
- Diphenhydramine causes drowsiness in 15-20% of users; fexofenadine causes it in only 6%.
- First-gen antihistamines score 3-4 on the Anticholinergic Cognitive Burden Scale - the highest risk level.
- Second-gen drugs score 0-1 - nearly zero risk.
A 2025 study directly compared fall rates between users of first- and second-generation antihistamines. Those on diphenhydramine or similar drugs had an 87% higher risk of falling. Those on loratadine or fexofenadine? No increase at all. Even cetirizine, which is sometimes called “mildly sedating,” only caused drowsiness in 14% of older adults - still better than diphenhydramine’s 20%.
That’s why experts say: if you need an antihistamine, pick one that doesn’t make you sleepy. Fexofenadine is often the safest bet. Loratadine is close behind. Cetirizine? Use it cautiously - especially if the person already has balance issues.
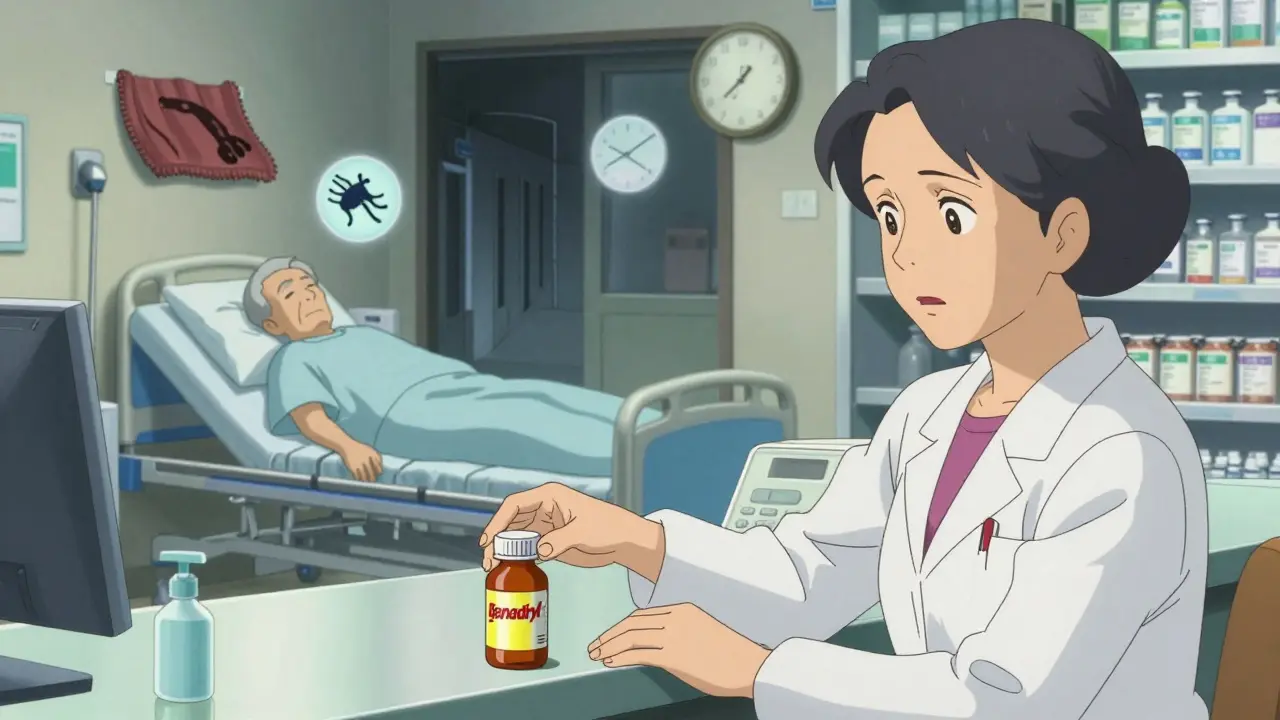
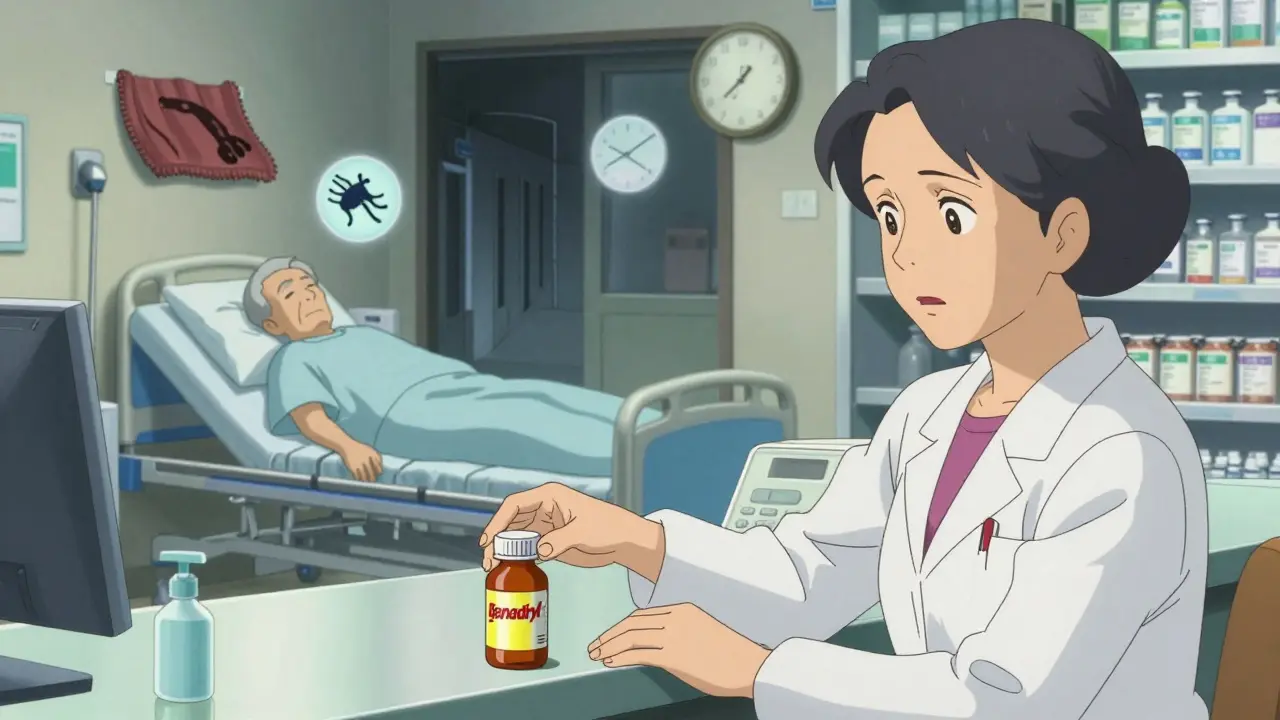
What’s Really Going On in Pharmacies and Doctor’s Offices
Here’s the uncomfortable truth: even though we know these drugs are risky, they’re still everywhere. Diphenhydramine is the third most popular OTC sleep aid in the U.S. for people over 65. Over 28 million units were sold in 2024 alone. Why? Because it’s cheap, it’s easy to find, and most people don’t realize it’s dangerous.
Pharmacists see it every day. An older adult walks in, says they’re having trouble sleeping, and walks out with a bottle of Benadryl. No one asks about their balance. No one checks if they’ve fallen before. No one mentions the CDC’s STEADI guidelines - which specifically warn against these drugs.
A 2019 study found that first-generation antihistamines were prescribed at nearly the same rate to older and younger patients - even though the risks for seniors are far higher. That’s not just outdated practice. It’s dangerous.
Even more troubling? Many primary care doctors still write these prescriptions. One study showed primary care offices prescribed them 15.2% of the time - higher than dermatology offices. That means people with allergies aren’t the only ones getting hit. Seniors taking them for sleep, motion sickness, or even nausea are being put at risk.
How to Prevent Falls: Three Simple Steps
The good news? Falls from these medications are preventable. The CDC’s STEADI initiative gives us a clear, practical plan: STOP, SWITCH, REDUCE.
- STOP - If the antihistamine isn’t truly necessary, stop it. Many older adults take these for mild allergies or occasional sleep. But non-drug options often work just as well. Nasal saline rinses reduce allergy symptoms by 35-40%. Allergen-proof bedding cuts dust mite exposure by 83%. HEPA filters remove 99.97% of airborne allergens. For sleep? Sleep hygiene - consistent bedtime, no caffeine after noon, dim lights - is more effective than any pill.
- SWITCH - If you need an antihistamine, switch to a second-generation one. Fexofenadine (Allegra) is the top recommendation. Loratadine (Claritin) is a solid second choice. Avoid cetirizine (Zyrtec) if balance is already an issue.
- REDUCE - If you can’t stop or switch, use the lowest possible dose. Instead of 25mg of diphenhydramine, try 12.5mg. Take it at night, not in the morning. Never combine it with alcohol, benzodiazepines, or opioids - that tripled the fall risk.
What You Can Do Right Now
If you or a loved one is over 65 and taking an antihistamine, here’s what to do:
- Look at the label. If it says “diphenhydramine,” “chlorpheniramine,” or “brompheniramine,” it’s high-risk.
- Ask your pharmacist for a “brown bag review.” Bring every pill, capsule, and supplement you take. Pharmacists can spot dangerous combinations - and they’re trained to flag sedating meds.
- Ask your doctor: “Is this the safest option for someone my age?” If they say yes without checking the Beers Criteria, ask for a second opinion.
- Watch for signs: stumbling, confusion, daytime drowsiness, blurred vision. These aren’t normal aging - they’re red flags.

More Than Just Medication: Environmental Changes Save Lives
Even if you switch meds, the home environment still matters. Falls aren’t just caused by drugs - they’re caused by drugs
plus a dark hallway, a loose rug, or a missing handrail.
Simple fixes make a huge difference:
- Install grab bars in the bathroom - reduces fall risk by 28%.
- Improve lighting - especially in hallways and staircases - cuts falls by 32%.
- Remove clutter, rugs, and extension cords.
- Use non-slip mats in the shower.
- Keep a flashlight by the bed.
Combine safer meds with a safer home, and you’re not just reducing risk - you’re preventing disaster.
The Future Is Happening - But Not Fast Enough
There’s hope on the horizon. Two new antihistamines - AGS-2025-01 and FEX-AGE-101 - are in late-stage trials. Early results show they cause 89% less drowsiness than diphenhydramine. They’re designed specifically for older adults.
But they’re still years away. In the meantime, we have what we need: better alternatives, clear guidelines, and proven strategies. The problem isn’t lack of knowledge. It’s lack of action.
Medicare now requires fall risk assessments during annual wellness visits - and that includes reviewing all medications, including OTC antihistamines. That’s a big step. But it only works if doctors and patients actually talk about it.
The numbers don’t lie. Every year, over 32,000 older adults die from falls. Many of those deaths are preventable. The fix isn’t complicated. It’s not expensive. It just requires paying attention.
Are over-the-counter antihistamines safe for older adults?
No, not if they contain first-generation antihistamines like diphenhydramine or chlorpheniramine. These drugs significantly increase fall risk, confusion, and delirium in older adults. Even though they’re sold without a prescription, they’re not safe for people over 65. Second-generation options like fexofenadine (Allegra) or loratadine (Claritin) are much safer alternatives.
Why is diphenhydramine still so common in older adults?
It’s cheap, easy to find, and many people still believe it’s a harmless sleep aid or allergy remedy. Manufacturers don’t have to warn consumers about fall risks on OTC labels. Many older adults aren’t aware of the Beers Criteria or CDC guidelines. Doctors sometimes prescribe it out of habit. The result? A dangerous gap between evidence and practice.
Can I just lower the dose instead of switching medications?
Reducing the dose helps - for example, using 12.5mg of diphenhydramine instead of 25mg - but it doesn’t eliminate the risk. Even low doses can impair balance in older adults. The safest approach is to switch to a non-sedating alternative like fexofenadine. If you must use a first-gen antihistamine, only use it at night, and never combine it with other sedatives.
What are some non-drug ways to manage allergies in older adults?
Nasal saline irrigation reduces allergy symptoms by 35-40%. Using allergen-proof bedding cuts dust mite exposure by 83%. HEPA air filters remove 99.97% of airborne allergens. Avoiding outdoor exposure during high-pollen days and showering before bed can also help. These methods are safer, cheaper, and just as effective as sedating antihistamines.
How can I talk to my doctor about stopping my antihistamine?
Say: “I’ve read that first-gen antihistamines like Benadryl increase fall risk in older adults. I’d like to stop it - what’s the safest way to do it? Are there non-drug options I can try instead?” Bring your medication list. Ask if they’ve reviewed your drugs using the Beers Criteria. A good doctor will help you taper safely and offer alternatives.