When you have chronic kidney disease (CKD), what you eat isn’t just about taste or preference-it’s about survival. Too much protein can overload your kidneys. Too little can leave you weak, hungry, and at risk of wasting away. The truth? There’s no one-size-fits-all number. Your protein target depends on how far your kidneys have declined, your age, your muscle mass, and whether you have diabetes or other health issues. This isn’t guesswork. It’s science-and it’s personal.
Your kidneys filter waste from your blood. When you eat protein, your body breaks it down into nitrogen waste, mostly urea. Healthy kidneys handle this easily. But when they’re damaged, that waste builds up. That’s why doctors have long advised cutting back on protein in CKD. The goal isn’t to starve you-it’s to slow down the damage. Studies show that keeping protein intake in the right range can delay the need for dialysis by 6 to 12 months. That’s not a small win. It’s extra time to live well, without tubes and machines.
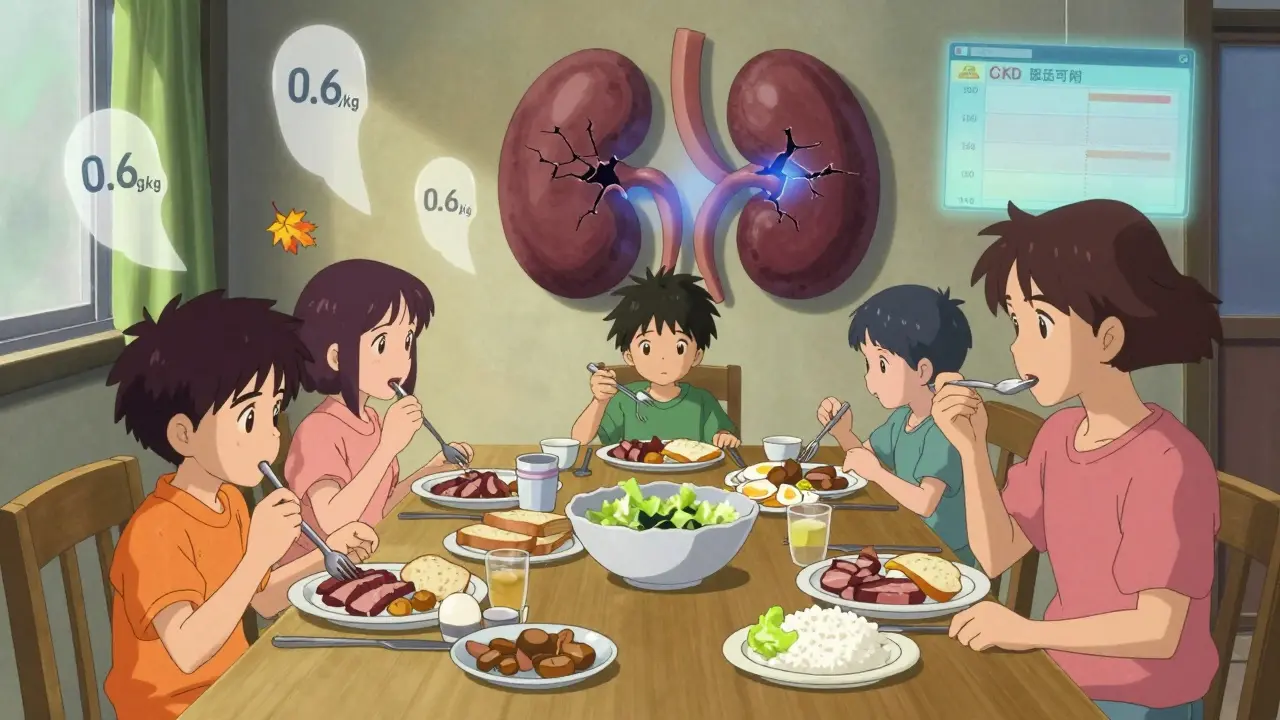
But here’s the twist: not all protein is the same. Animal proteins-like beef, chicken, eggs, and dairy-produce more waste per gram than plant proteins like beans, lentils, tofu, and nuts. They also pack more phosphorus and create more inflammatory compounds called AGEs. Plant proteins? They’re gentler on the kidneys. One major study found that replacing just 30% of animal protein with plant protein cut the risk of kidney failure by 14%. That’s a big deal.
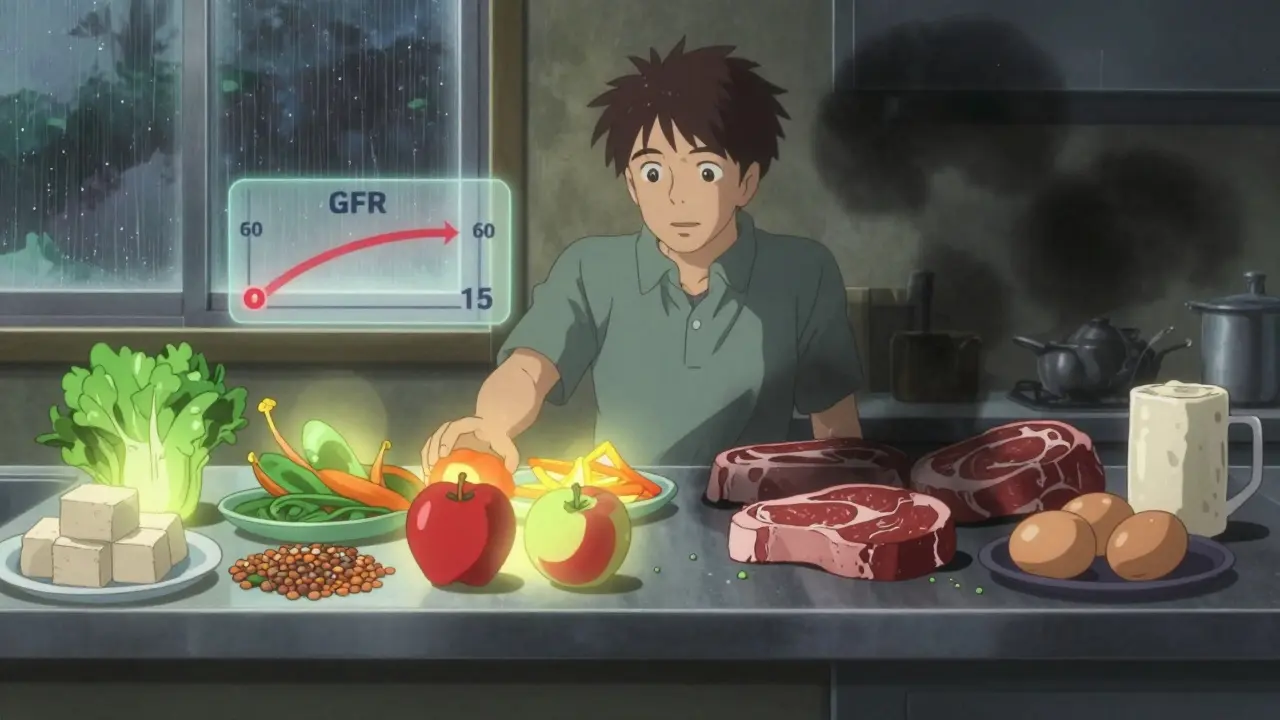
CKD is broken into five stages, based on how well your kidneys filter blood (measured by GFR). Your protein needs change at each stage.
Diabetics with CKD need special attention. The American Diabetes Association recommends 0.8-0.9 g/kg to protect both kidneys and blood sugar. Too little protein can make insulin harder to control. Too much can speed up kidney damage. It’s a tightrope walk.
Not all protein sources are created equal when it comes to kidney health.
Animal proteins-red meat, chicken, cheese, eggs-give you all the amino acids your body needs. But they also produce 20-30% more urea and phosphate than plant proteins. They’re also loaded with advanced glycation end products (AGEs), which trigger inflammation and oxidative stress. Over time, that can make kidney damage worse.
Plant proteins-lentils, chickpeas, tofu, quinoa, nuts-produce less waste. They’re also rich in fiber and antioxidants. But they’re incomplete. They lack enough lysine and methionine. That means you can’t just swap chicken for beans and call it a day. You need to combine them. Eat rice with beans. Have hummus with whole grain pita. Mix soy with nuts. This way, you get the full amino acid profile without overloading your kidneys.
One catch: plant foods are often high in potassium. That’s fine for early-stage CKD. But if you’re in stage 4 or 5 and need to limit potassium, you’ll have to choose carefully. Avoid bananas, potatoes, spinach, and oranges. Opt for apples, cabbage, cauliflower, and berries instead.
Even with the best advice, sticking to a low-protein diet is hard. A 2024 survey of over 1,200 CKD patients found that 74% felt constantly hungry. 62% said they felt weak. 58% avoided eating with family because they couldn’t eat what everyone else was having.
Tracking protein is another nightmare. Most people don’t realize how much protein is in a sandwich, a soup, or a protein bar. One study found that 87% of patients struggle to estimate protein in mixed meals. A chicken breast might seem like a safe choice-but add a slice of bread, a spoon of peanut butter, and a glass of milk, and you’ve hit your daily limit before lunch.
And here’s the sad part: only 35% of nephrologists refer patients to renal dietitians, even though guidelines say they should. That’s a huge gap. Patients who work with a dietitian are 3.2 times more likely to stick to their plan.
It’s not about perfection. It’s about smart, sustainable changes.
Some patients use keto acid analogues like Ketosteril. These are prescription supplements that provide essential amino acids without the nitrogen waste. They’re used in about 15% of stage 4-5 CKD patients in Europe. Not available everywhere, but worth asking your doctor about if you’re struggling to meet targets.
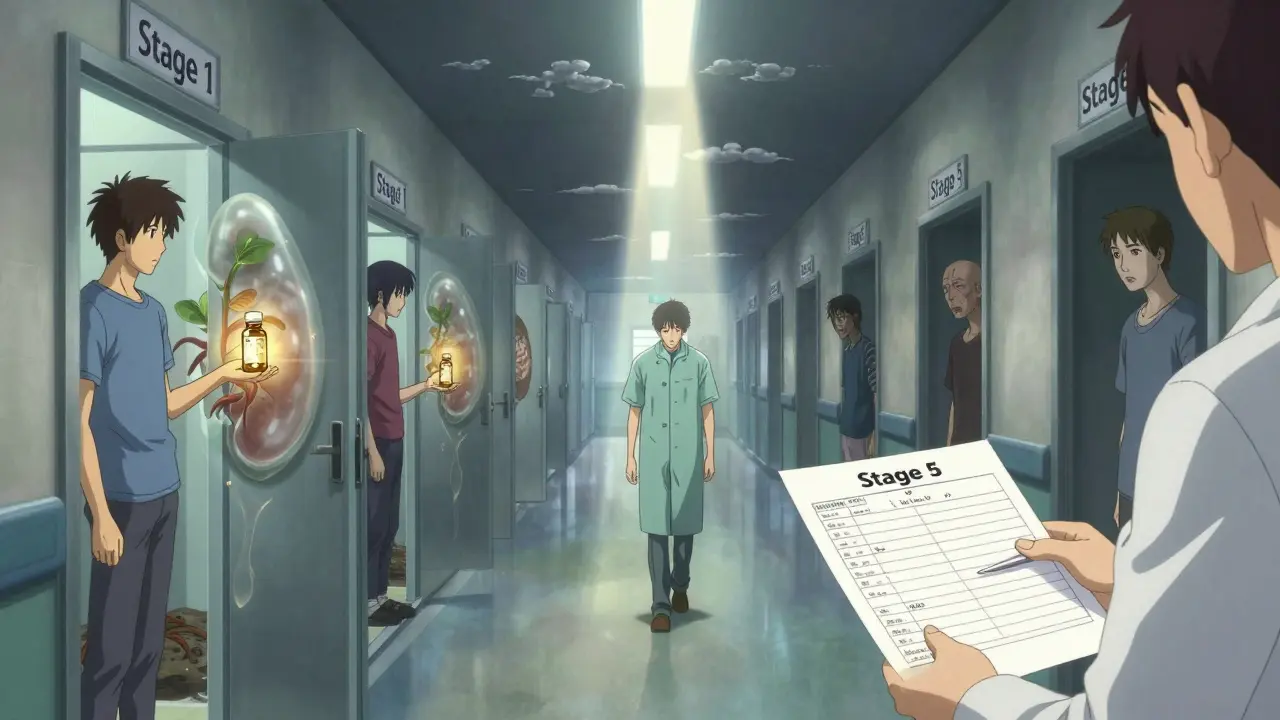
Protein restriction isn’t a magic bullet. It’s one tool in a bigger toolkit. You also need to control blood pressure, manage blood sugar, limit sodium, and watch phosphorus and potassium. But protein is the foundation.
Experts now agree: the future of renal nutrition isn’t just about how much protein you eat-it’s about what kind. Plant-based diets are gaining ground. Precision nutrition-using your genetics, urea levels, and metabolic rate to tailor your protein target-is being tested in NIH trials right now.
And here’s the good news: 92% of nephrologists believe personalized protein management will remain key through 2030. The goal isn’t to make you miserable. It’s to help you live longer, feel stronger, and avoid dialysis as long as possible.
For stage 3 CKD (GFR 30-59 mL/min), aim for 0.6 to 0.8 grams of protein per kilogram of your ideal body weight. For a 150-pound person, that’s about 40-54 grams per day. Half of that protein should come from high-quality sources like eggs, fish, poultry, and soy. Always check with your dietitian-your needs may change if you’re diabetic, older, or losing weight.
Yes, and it’s often better for your kidneys. Plant proteins like beans, lentils, tofu, and nuts produce less waste and inflammation than animal proteins. But they’re incomplete-they lack some essential amino acids. Combine them: rice with beans, hummus with whole grain bread. Watch potassium levels if you’re in stage 4 or 5. Avoid high-potassium plants like spinach, potatoes, and bananas. Choose lower-potassium options like apples, cabbage, and cauliflower.
It can-if you don’t get enough calories or the right kind of protein. Many CKD patients feel weak because they cut protein too low without replacing calories from carbs and healthy fats. You need enough energy to use the protein you do eat. If you’re losing weight or feeling tired, talk to your dietitian. You may need to add more rice, pasta, or oils to your meals to keep your energy up while staying within protein limits.
Most people don’t need protein powders or shakes-they often have too much phosphorus and nitrogen. But some stage 4-5 patients use keto acid analogues like Ketosteril. These are prescription supplements that give your body the amino acids it needs without adding waste. They’re not for everyone, but they can help if you’re struggling to meet protein targets without overloading your kidneys. Ask your nephrologist if they’re right for you.
Use apps like MyFitnessPal with the renal database turned on. Look up foods by name and serving size. When eating out, choose simple dishes: grilled fish, steamed vegetables, white rice. Avoid sauces, gravies, and processed meats-they hide protein. If you’re unsure, ask for the nutrition info. Most chain restaurants have it online. And don’t be afraid to ask your dietitian for a cheat sheet of common restaurant meals and their protein content.
It’s complicated. For older adults, especially over 65, very low protein can increase the risk of muscle loss and death from heart disease. A 2024 study found that higher protein intake (up to 0.8-1.0 g/kg) was linked to lower mortality in this group. The key is balance: don’t go too low. Aim for 0.6-0.8 g/kg, prioritize high-quality protein, and make sure you’re eating enough calories. Work with your doctor to find your personal sweet spot.
No. Diet can’t repair damaged kidney tissue. But it can slow down further damage. Controlling protein, sodium, phosphorus, and blood pressure can delay progression to dialysis by years. In some cases, especially in early stages, kidney function can stabilize. But that’s not the same as reversal. The goal is to protect what’s left and live well for as long as possible.
If you’re managing CKD, you’re not alone. But you need the right support. Start by asking your nephrologist for a referral to a renal dietitian. Use free tools like the NKF Protein Calculator. Learn to read food labels-not just for protein, but for phosphorus additives like “phos” or “calcium phosphate.”
Don’t wait until you’re desperate. Start now. Even small changes-swapping beef for tofu, choosing white rice over brown, cutting out processed snacks-add up. You’re not just eating to survive. You’re eating to live.
So let me get this straight-we’re supposed to starve ourselves to keep our kidneys from failing, but not so much that we turn into walking skeletons? This isn’t nutrition. It’s a fucking hostage negotiation with your own body.
And don’t even get me started on the plant protein ‘solution.’ Beans give me gas so bad I’ve been kicked out of three yoga classes. If my kidneys are failing, the last thing I need is to be banned from public spaces because my gut betrayed me.
Also, who decided 0.55g/kg is the magic number? Some guy in a lab coat who’s never eaten a meal with his family? My grandma ate a whole roast chicken every Sunday and lived to 92. Her kidneys were fine. Coincidence? Or are we just being manipulated by overcomplicated science that doesn’t care about real life?
It’s wild how we treat food like a math problem when it’s so deeply human. Protein isn’t just grams-it’s memory. The smell of eggs frying on Sunday. The comfort of a bowl of lentil stew after a long day.
I used to think cutting protein meant giving up joy. But I switched to tofu and chickpeas and realized I didn’t lose flavor-I just learned new ways to love what I eat.
It’s not about restriction. It’s about listening. Your body’s not your enemy. It’s trying to tell you something.
Per KDIGO guidelines, protein intake in CKD stages 3-5 should be 0.6–0.8 g/kg/day for non-dialysis patients, with emphasis on high biological value proteins. Plant-based proteins reduce acid load and phosphorus retention, which correlates with slower GFR decline in longitudinal studies (JASN 2020;31:2345–2356).
For a 70kg individual, this equates to 42–56g daily. Animal protein should not exceed 50% of total intake. Soy is an exception-it has comparable amino acid profile to animal protein and lower phosphate bioavailability. Always consult a renal dietitian before making dietary changes.
Doctors say cut protein but then say eat good protein what even is that
Why do we need a whole chart for this
Just eat less meat and more beans and stop overthinking it
My uncle had stage 4 and he ate steak twice a week and lived five years longer than the prognosis
Science is just guesses with fancy words
Wow. So we’re supposed to be grateful for a 6–12 month delay in dialysis? That’s like being told you can keep your house for six more months before the foreclosure. Congrats, I guess.
Meanwhile, the food industry is selling us ‘renal-friendly’ protein powders that cost $40 a tub. Someone’s making bank off our fear.
I’m not mad. I’m just… tired. Of being told what to eat like I’m a pet with a special diet.
Let me be clear: this isn’t a suggestion. It’s a lifeline. I’ve seen patients in stage 4 who ignored protein limits and ended up on dialysis six months later-with no energy, no appetite, no quality of life.
Plant-based doesn’t mean bland. Try lentil curry with turmeric, roasted eggplant with tahini, quinoa bowls with avocado and pumpkin seeds. Flavor isn’t the enemy. Neglect is.
If you’re reading this and you’re scared-you’re not alone. But you’re also not powerless. Small changes, daily, add up to years.
And yes, it’s hard. But so is breathing through a tube.
People think they’re being ‘healthy’ by eating tofu and kale like it’s some kind of moral victory. Newsflash: your kidneys don’t care about your Instagram diet board.
You think you’re saving yourself by avoiding meat? What about the processed soy isolate in your ‘renal protein bar’? It’s full of additives, sodium, and chemicals that your kidneys didn’t sign up for.
Real food isn’t packaged. Real food doesn’t have a ‘kidney-friendly’ label. Eat real. Eat simple. Eat what your ancestors ate before Big Pharma invented ‘CKD diets.’
And stop letting doctors scare you into buying supplements.
Just eat. And breathe. And stop pretending nutrition is a religion.
I used to think kidney disease meant giving up everything I loved. Then I tried making a creamy mushroom and barley stew with a splash of tamari and a poached egg on top. It was the most comforting thing I’d eaten in years.
Turns out, you don’t have to lose flavor to protect your body. You just have to get creative.
My GFR’s been stable for two years now. Not because I followed a chart-but because I started cooking like I was feeding someone I loved.
And yeah, I still eat chicken. Just less of it. And I savor every bite.
My mom’s in stage 3b. She eats a grilled salmon filet every other day, a handful of almonds, and calls it a day. No spreadsheets. No apps. Just food she likes.
Her numbers are better than the guy in her nephrology group who counts every gram and still looks like a ghost.
Maybe the answer isn’t in the numbers. Maybe it’s in the quiet moments-eating slowly, without guilt.