Select your medication and your typical caffeine intake to see if there's a potential interaction risk.
Select your medication and caffeine intake to see results
Many people start their day with a cup of coffee, unaware that it could be quietly interfering with their medications. What seems like a harmless habit-drinking coffee with your morning pills-can actually reduce how well your drugs work, or make side effects worse. This isn’t just a myth. It’s a documented, clinically significant issue that affects millions. And the risks aren’t theoretical. People end up in emergency rooms because of these interactions. If you take any kind of prescription or over-the-counter medication, you need to know how caffeine changes the game.
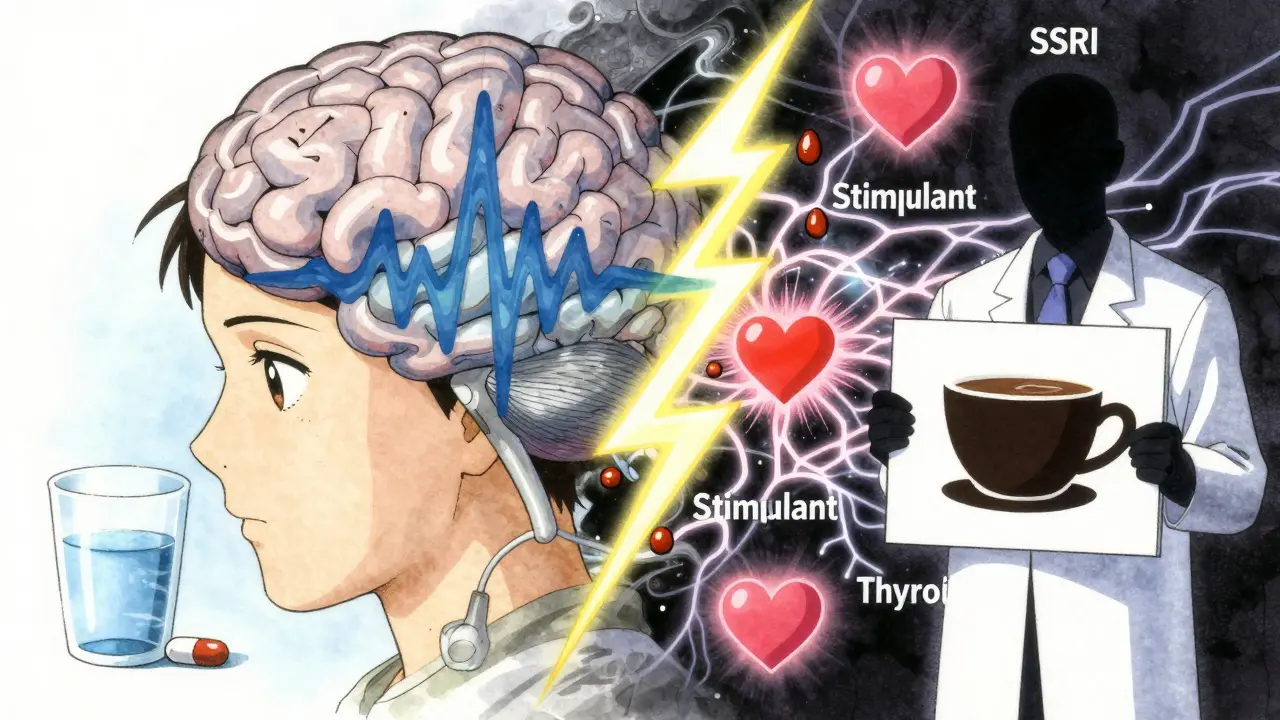
Caffeine doesn’t just wake you up. It also messes with your liver’s ability to break down certain drugs. The main enzyme it affects is called CYP1A2. This enzyme handles about 10-15% of all prescription medications. When caffeine blocks it, those drugs build up in your bloodstream. That means higher doses than intended, even if you’re taking the right pill at the right time.
Think of it like a traffic jam on a highway. Your liver is the toll booth. Normally, drugs pass through smoothly. But caffeine? It’s a stalled truck right in front. Everything behind it-your medications-gets stuck. That’s why some drugs become too strong, too fast.
On the flip side, caffeine can also block the effects of certain drugs by competing for the same receptors in your body. For example, adenosine is a natural chemical that helps calm your heart. Medications like adenosine (Adenocard) and dipyridamole (Persantine) use this to slow your heart during stress tests. But caffeine blocks adenosine receptors. So if you drink coffee before the test, the medication can’t do its job. The test becomes useless. You’ll have to reschedule. And that’s just one example.
If you’re on warfarin (Coumadin), your blood’s clotting time is carefully monitored with a test called INR. Even small changes in your diet or habits can throw this off. Caffeine is one of the biggest hidden culprits.
Studies show that drinking coffee while on warfarin can raise your INR by 15-25% within 24 hours. That means your blood takes longer to clot. You’re at higher risk for bruising, nosebleeds, or worse-internal bleeding. The American Heart Association warns that people on warfarin should limit caffeine to no more than 200 mg per day (about two cups of coffee) and keep their intake consistent. One day with three espressos, then a day with none? That’s a recipe for dangerous INR swings.
It’s not just warfarin. Newer blood thinners like apixaban (Eliquis) are also being studied. Early data from a 2025 NIH study suggests high caffeine intake (>400 mg daily) can increase apixaban levels by 10-15%. That’s enough to raise bleeding risk, especially in older adults.
Levothyroxine (Synthroid, Levoxyl) is one of the most commonly prescribed drugs in the U.S. But it’s also one of the most sensitive to food and drink. Coffee, even decaf, can reduce its absorption by 25-57%.
A 2017 study with 98 patients showed this clearly. Those who drank coffee within an hour of taking their thyroid pill had significantly lower hormone levels. Their TSH (a key thyroid marker) jumped from a stable 1.8 to 4.5-well outside the normal range. That’s why doctors now recommend waiting 30 to 60 minutes after taking levothyroxine before drinking coffee. Some patients wait even longer. One Reddit user wrote: “I didn’t realize my coffee was making my Synthroid less effective until my TSH levels were 4.5 after being stable at 1.8 for years-waiting 60 minutes after my pill made all the difference.”
It’s not just coffee. Tea, calcium supplements, and even high-fiber meals can interfere. But coffee is the most common offender. And here’s the kicker: decaf coffee still contains 2-15 mg of caffeine per cup. That’s enough to affect sensitive patients.
If you’ve ever had a cardiac stress test, you’ve probably been told: “No caffeine for 24 hours.” But why? Because caffeine blocks the very mechanism those tests rely on.
Drugs like adenosine and dipyridamole work by mimicking the body’s natural calming signals to the heart. Caffeine acts like a shield against those signals. So if you had even one cup of coffee the day before, the test can’t detect heart problems properly. Results come back inconclusive. You’re sent home. You have to come back. You waste time. You delay diagnosis.
The American College of Cardiology’s 2023 guidelines are clear: no caffeine for 24 hours before the test. That includes tea, energy drinks, chocolate, and even some pain relievers with caffeine. One patient on HealthTap wrote: “I had one cup of coffee anyway and my test results were inconclusive-I had to reschedule.” That’s not just inconvenient. It’s risky.
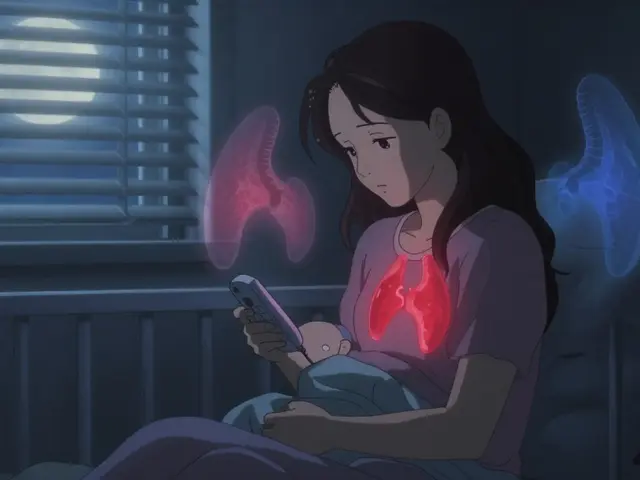
If you’re on antidepressants, caffeine can turn your treatment into a nightmare. It doesn’t just make you jittery-it changes how your body handles the drug.
Fluvoxamine (Luvox) and escitalopram (Lexapro), both SSRIs, are metabolized by CYP1A2. When caffeine blocks this enzyme, these drugs build up in your blood. Harvard Health found this can reduce absorption of fluvoxamine by up to 33%. That means less relief from depression or anxiety. Or worse-you get too much of the drug. Side effects like nausea, dizziness, and heart palpitations spike.
Tricyclic antidepressants like amitriptyline and imipramine are even more sensitive. Caffeine can increase their blood levels by 20-40%. That’s a big jump. Patients report extreme restlessness, insomnia, and heart racing. On PatientsLikeMe, someone wrote: “I felt extremely jittery and unable to sleep for 12+ hours after taking my Adderall with morning coffee.” Adderall is a stimulant. Caffeine is a stimulant. Together? They’re a double hit on your nervous system.
And the numbers back this up. A review of 1,247 patient reviews on Drugs.com showed 68% of people on psychiatric meds reported increased anxiety when drinking caffeine. Nearly half said their meds didn’t work as well.
Combining caffeine with pseudoephedrine (found in Sudafed) or ephedrine is like lighting a fuse. Both are stimulants. Together, they can spike your heart rate by 20-35 beats per minute and raise systolic blood pressure by 15-25 mmHg within 45 minutes. That’s dangerous for anyone, but especially for older adults or those with heart conditions.
For people with diabetes, this combo is even riskier. University Hospitals’ 2025 update found that caffeine plus pseudoephedrine can raise blood sugar by 15-25 mg/dL. That’s enough to throw insulin dosing off. Body temperature can also rise by 0.5-1.0°C. That’s not just uncomfortable-it can signal a hidden metabolic crisis.
And it’s not just cold meds. ADHD stimulants like Adderall and Ritalin, when mixed with caffeine, create a similar effect. Many users report feeling “wired,” unable to sleep, or experiencing chest tightness. Doctors now warn against combining these unless absolutely necessary-and even then, only under close supervision.
So what’s the fix? It’s not about giving up coffee. It’s about timing and awareness.
Most people don’t realize how much caffeine is in their drinks. A grande Starbucks coffee has about 330 mg. A can of Red Bull has 80 mg. Dark chocolate? 20-30 mg. Even some headache pills like Excedrin have 65 mg of caffeine per tablet.
Some reactions to caffeine-medication interactions are serious. You need emergency care if you experience:
These aren’t normal side effects. They’re signs your body is overwhelmed. Don’t wait. Call 999 or go to the nearest emergency department.
Over 150 million Americans consume caffeine daily. Nearly half take at least one prescription medication. That means tens of millions are at risk for these interactions. The American Pharmacists Association estimates these interactions cause 2.8% of all community-based adverse drug events. For people over 65, that number jumps to 4.2%.
And the cost? Over $1.2 billion a year in preventable hospital visits, lab tests, and emergency care. That’s not just money. It’s lost time, stress, and health.
Pharmacies now have systems that flag caffeine interactions in 127 medications-up from 89 in 2020. The FDA has added caffeine warnings to 15 new drug labels since March 2024. Hospitals are embedding caffeine screening into electronic records. But none of that helps if you don’t know to ask.
The solution isn’t complex. It’s simple: know your meds. Know your caffeine. Talk to your pharmacist. Write down your routine. And if you’re unsure-ask. Your life might depend on it.
No, not right away. Coffee can reduce the absorption of levothyroxine by up to 57%. Wait at least 30 to 60 minutes after taking your pill before drinking coffee. Some people wait longer to be safe. Even decaf coffee contains enough caffeine to interfere, so it’s best to avoid it too during this window.
Yes. Caffeine can temporarily raise blood pressure and reduce the effectiveness of some medications like verapamil. Studies show diastolic blood pressure can stay 8-12 mmHg higher for 2-3 hours after caffeine intake. If you’re on blood pressure meds, limit caffeine and monitor your readings. Consistency matters more than total avoidance.
Not always. Decaf coffee still contains 2-15 mg of caffeine per cup. That’s enough to interfere with sensitive medications like thyroid hormones, SSRIs, or stimulants. If you’re highly sensitive, switch to herbal tea or water. For most people, one cup of decaf is fine-but not if you’re taking multiple interacting drugs.
Caffeine blocks adenosine receptors in your heart. Stress tests use adenosine or dipyridamole to simulate exercise and check for heart problems. If caffeine is in your system, the test can’t work properly. Results become inconclusive, and you’ll need to reschedule. The American College of Cardiology requires 24 hours of caffeine abstinence before the test.
Yes, for some. Caffeine can reduce absorption of SSRIs like fluvoxamine by up to 33%. For tricyclics like amitriptyline, it can increase blood levels by 20-40%, making side effects worse. If you notice more anxiety, insomnia, or heart racing after drinking coffee, talk to your doctor. You might need to adjust timing or switch meds.
Ask your pharmacist. They have access to drug interaction databases that flag caffeine as a concern for over 127 medications. Look for warnings on your prescription label. If it’s not clear, call your doctor or check reputable sources like Micromedex or the FDA’s drug database. Don’t rely on Google or social media.
If you only had one cup and feel fine, monitor yourself. Watch for unusual heart rate, dizziness, anxiety, or tremors. Don’t take another dose of your medication. If you feel unwell-especially with chest pain, rapid heartbeat, confusion, or trouble breathing-seek medical help immediately. Going forward, write down your routine and set phone reminders to separate caffeine and meds.
There’s no need to quit coffee entirely. But if you take medication, treat caffeine like a drug-because it is. It interacts. It changes outcomes. It can save your life-or cost you your health. The choice is yours. Just make it informed.
Caffeine interactions with meds are way more common than people realize. I work in pharmacy and see this weekly-patients on warfarin drinking three espressos a day, then wondering why their INR spiked. It’s not about fear, it’s about consistency. One cup at the same time daily beats bingeing and then going cold turkey. Small habit tweaks prevent ER visits.
Wow. Another ‘coffee is evil’ scare piece. CYP1A2 inhibition is real, sure-but you’re telling me someone on levothyroxine shouldn’t have coffee? That’s like saying you shouldn’t breathe air because oxygen can oxidize lipids. The data is noisy, the effect size is marginal for most, and you’re scaring people into unnecessary ritualistic behavior. 200mg cap? Arbitrary. If your TSH is stable, stop obsessing.
This post saved me. I was on Synthroid for years, TSH hovering at 4.5, feeling exhausted, foggy, like I was just… not myself. My doctor kept adjusting my dose. Then I read about coffee interfering. I started waiting 60 minutes after my pill. Within two weeks, my energy came back. My TSH dropped to 1.9. I didn’t quit coffee-I just changed when I drank it. Small change. Huge difference.
Decaf still has caffeine bro so if you sensitive just drink water in the morning lol
I’ve been on fluvoxamine for anxiety and didn’t realize my afternoon latte was making me more jittery, not less. I cut back to one cup before noon and noticed my sleep improved immediately. I didn’t even know caffeine could interfere with SSRIs like that. Thank you for the clarity. This is the kind of info that should be on prescription labels.
Of course coffee messes with your meds. You’re not a lab rat. If you’re too lazy to read the damn pamphlet that comes with your pills, then you deserve the side effects. People take Adderall with Red Bull and wonder why they have a heart attack. It’s not magic. It’s basic biology. Stop blaming the drug. Blame yourself.
Y’all need to chill. I’m Indian and we drink chai with our meds since the 90s. My grandpa took blood pressure pills with masala tea and lived to 92. Yeah, science says caffeine might interfere, but real life isn’t a clinical trial. Maybe the real issue is overmedicating and under-living. Drink your coffee. Live your life. Talk to your doc if you feel weird.
Just want to say I appreciate how detailed this is. I’ve had two inconclusive stress tests because I forgot to skip coffee. I didn’t realize it was that serious. Now I set a 48-hour caffeine alarm on my phone. It’s annoying, but better than rescheduling and waiting another month. Small effort, big payoff.
It is a matter of considerable scientific and clinical concern that the general populace continues to conflate the consumption of a psychoactive alkaloid with the routine ingestion of a therapeutic agent. The pharmacokinetic interactions between caffeine and CYP1A2 substrates are not merely anecdotal-they are reproducible, dose-dependent, and statistically significant in peer-reviewed literature. One must exercise the utmost diligence in temporal separation and dosage consistency to mitigate the risk of iatrogenic harm. I implore all patients to consult their pharmacists and maintain a daily log.
Let’s be real-this whole post reads like a Pharma ad written by someone who hates fun. Caffeine? A drug? Yeah, so is water. You’re telling me I can’t have my morning espresso before my Eliquis? What’s next, no sunlight because it interferes with vitamin D absorption? This isn’t medicine, it’s control. You’re turning a simple habit into a clinical compliance nightmare.
Decaf coffee isn’t safe for everyone. I’m ultra-sensitive. Even 5mg of caffeine gives me palpitations. I switched to roasted chicory root tea. Tastes like coffee, zero caffeine, no interference. My TSH is stable now. It’s not about giving up coffee-it’s about finding what works for your body.
Oh my GOD, I’ve been drinking coffee WITH my Synthroid for 7 years!!! That’s why I’ve been so tired!! I’m literally crying right now. And my Adderall? I’ve been having it with a triple espresso since college. No wonder I’ve had panic attacks every Tuesday. I’m going to the pharmacy tomorrow. I’m so mad at myself. Why didn’t anyone tell me?!
What’s fascinating is how we’ve normalized the ritual of chemical dependency-coffee as sacrament, pills as duty-and then act shocked when they collide. The real issue isn’t caffeine-it’s the illusion that we can compartmentalize our bodies into discrete systems. We are not machines. We are messy, biochemically entangled beings. The answer isn’t more rules. It’s deeper awareness. Are you listening to your body-or just following instructions?
I’ve been on levothyroxine for 12 years. I drink coffee 20 minutes after my pill. My TSH is perfect. I’ve never had a problem. Maybe it’s not the coffee. Maybe it’s the individual. Some people are sensitive. Others aren’t. Don’t make a blanket rule for everyone. Talk to your doctor. Test your levels. Adjust accordingly. One size doesn’t fit all.