This tool helps you understand your risk of developing diabetes while taking different statins based on clinical studies. Use it to discuss with your doctor whether pitavastatin might be a better option for you.
If you’ve been told to take a statin for high cholesterol - and you also have prediabetes or insulin resistance - you’re probably wondering: will this drug make my blood sugar worse? It’s a real concern. Not all statins are the same. While some raise blood sugar and increase diabetes risk, pitavastatin stands out. It’s one of the few statins that doesn’t seem to hurt glucose control - and might even be safer for people already at risk.
Pitavastatin is a third-generation statin, approved by the FDA in 2009. It lowers LDL cholesterol just like atorvastatin or rosuvastatin, but how it does it is different. Most statins are broken down by liver enzymes called CYP450, which leads to lots of drug interactions. Pitavastatin? Half is cleared by the kidneys, half by the liver. That means fewer interactions, and importantly, fewer disruptions to how your body handles sugar.
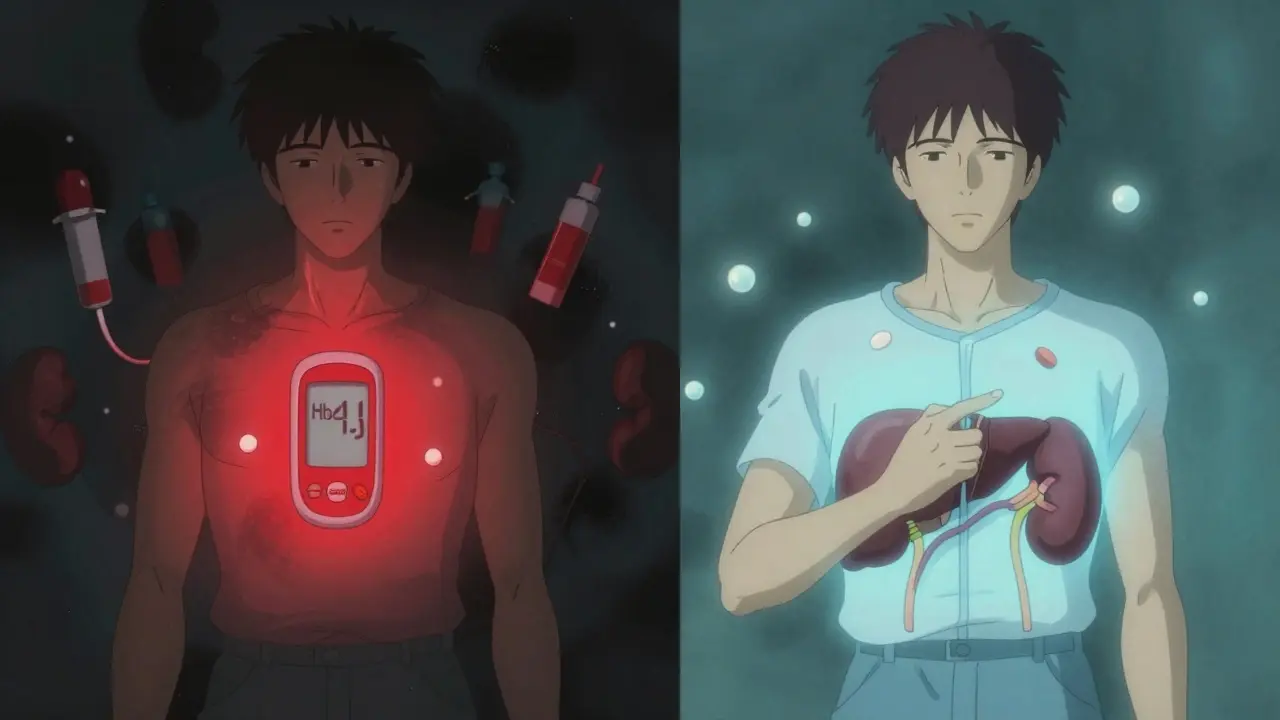
Statins work by blocking HMG-CoA reductase, the enzyme your liver uses to make cholesterol. That’s good for your arteries. But that same blockage seems to interfere with insulin signaling in muscle and fat cells. In some people, this leads to higher fasting glucose, higher HbA1c, and eventually, type 2 diabetes.
Studies show rosuvastatin and atorvastatin increase new-onset diabetes risk by about 12-18%. The risk is dose-dependent: the higher the statin intensity, the greater the chance. But pitavastatin? Multiple large studies show it doesn’t follow that pattern.
A 2018 study in the Journal of Clinical Endocrinology & Metabolism looked at men with insulin resistance. They were given 4 mg of pitavastatin daily - the highest dose - for six months. Researchers used the gold-standard euglycemic hyperinsulinemic clamp test to measure insulin sensitivity. Result? No change. Not a drop. Not a rise. Fasting glucose stayed stable. HbA1c didn’t budge. Even liver fat levels didn’t increase.
Compare that to rosuvastatin. In the same study design, rosuvastatin reduced insulin sensitivity by 16%. Pitavastatin? Zero effect.
A 2022 meta-analysis in Cardiovascular Diabetology looked at data from over 124,000 patients. The results were clear:
The hazard ratios didn’t just trend lower - they were statistically significant. P-values were under 0.001. This isn’t noise. It’s a pattern.
Another analysis from 2017, covering over 113,000 patients, found the rate of new diabetes per 100 person-years:
Pitavastatin sits right between pravastatin and the higher-risk statins. That’s not a fluke. It’s consistent across studies - even in populations with high diabetes risk like people with HIV or metabolic syndrome.
In the INTREPID trial, 152 adults with HIV and high cholesterol were randomized to pitavastatin or pravastatin. Over a year, HbA1c rose just 0.05% in the pitavastatin group. Pravastatin? 0.12%. The difference wasn’t significant - but it shows pitavastatin didn’t make things worse. In fact, it was neutral.
Behind the numbers, real patients are telling a story. On forums like Reddit’s r/Cardiology, physicians report switching patients from atorvastatin to pitavastatin because their HbA1c kept climbing. One doctor said he’d switched at least 20 prediabetic patients - and 17 saw their blood sugar stabilize or improve within six months.
It’s not just anecdotal. A 2023 survey of 456 cardiologists found 68.2% would choose pitavastatin for a patient with prediabetes. Only 12.7% would pick atorvastatin. That’s a massive difference in clinical preference.
But it’s not perfect. One small 2019 study from South Korea reported the opposite - that pitavastatin had the highest diabetes risk among statins. But it was a single-center, retrospective study with only 3,680 patients. It didn’t control for key variables like baseline BMI or fasting glucose. Most experts dismiss it as an outlier.
If you’re in one of these groups, pitavastatin might be the smartest statin choice:
The American Diabetes Association and the American College of Cardiology both updated their guidelines in 2023 to say this: when you need a moderate-intensity statin, pitavastatin or pravastatin are preferred options for people with diabetes or high diabetes risk.
Why moderate intensity? Because pitavastatin 4 mg lowers LDL by 35-50%. That’s enough for most people who don’t need to hit ultra-low targets. If you’ve had a heart attack or have familial hypercholesterolemia, you might still need high-intensity statins - but even then, switching to pitavastatin could help protect your metabolism.
Pitavastatin isn’t cheap. The brand name, LIVALO, costs about $350 a month out-of-pocket. Generic atorvastatin? $4. That’s a 90% price difference.
But here’s the catch: 92% of Medicare Part D plans cover pitavastatin as a tier 2 drug. That means most seniors pay around $45 a month - not $350. Many commercial insurers also cover it with a $20-$50 copay if your doctor documents diabetes risk.
It’s not always easy to get approved, but it’s doable. If your doctor writes a letter explaining you have prediabetes and need a statin with minimal metabolic impact, insurers usually approve it.
And if cost is still a barrier? Ask about patient assistance programs from Kowa Pharmaceuticals. They offer free or discounted access to people who qualify.
Here’s the big question: if pitavastatin is better for blood sugar, is it just as good for your heart?
So far, yes - but we’re waiting for the final answer. The PERISCOPE trial, a 5,200-patient study comparing pitavastatin 4 mg to atorvastatin 40 mg in people with type 2 diabetes, is still ongoing. Results are expected in late 2026. If it shows pitavastatin is just as good at preventing heart attacks and strokes - and better for glucose - it could change guidelines again.
Current evidence says pitavastatin doesn’t increase cardiovascular risk. In fact, the same studies that show it doesn’t raise blood sugar also show it reduces LDL and plaque buildup just like other statins.
If you’re on a statin and worried about blood sugar:
And if you’re not on a statin yet - but have high cholesterol and prediabetes - ask your doctor: "Is pitavastatin the right first choice for me?" You’re not being difficult. You’re being smart.
Even if you’re on pitavastatin, you still need to monitor. All statins can affect blood sugar in rare cases. The American Association of Clinical Endocrinologists recommends:
If your HbA1c rises more than 0.4% in the first year, it’s time to reevaluate. That’s not normal. It’s a signal - not necessarily a failure of the drug, but a sign you might need a different approach.
Pitavastatin gives you a better shot at protecting both your heart and your metabolism. But you still need to stay involved. Track your numbers. Ask questions. Don’t assume your doctor knows every statin’s metabolic profile - many don’t.
No, pitavastatin is not linked to weight gain. In fact, some studies show no change in body weight or waist circumference in patients taking it, even over long periods. Weight gain is more commonly tied to lifestyle factors or other medications, not pitavastatin.
Yes. Pitavastatin is safe and effective for people with type 2 diabetes. It lowers LDL cholesterol without worsening blood sugar control. In fact, it’s often preferred over rosuvastatin or atorvastatin in diabetic patients because it’s less likely to raise HbA1c.
Both are among the safest statins for blood sugar. Pravastatin has slightly more long-term data, but pitavastatin is more potent at lowering LDL - meaning you can get the same heart protection with a lower dose. For most people with prediabetes, pitavastatin 2-4 mg is the better balance of effectiveness and metabolic safety.
Most patients see stabilization in HbA1c within 3 to 6 months. Some see improvements as early as 8 weeks. Don’t expect a dramatic drop - the goal is to stop the rise, not reverse diabetes. Regular testing at 3 months is key to tracking progress.
Unlike other statins, pitavastatin doesn’t interact with grapefruit juice or most supplements. It’s also not affected by common medications like blood pressure pills or antibiotics. That’s one of its biggest advantages. Still, always tell your doctor what you’re taking - including vitamins and herbal products.
The real danger isn’t taking a statin. It’s taking the wrong one for your body. If you have prediabetes, high cholesterol, and you’re worried about your future risk of diabetes - pitavastatin gives you a rare win-win. You lower your heart attack risk without raising your diabetes risk. That’s not magic. It’s science.
And with more data coming in 2026, we’re likely to see it become the go-to statin for millions of people who need cholesterol control without metabolic trade-offs.
This is the most balanced take on statins I've seen in years. Pitavastatin flying under the radar like this is wild-like finding a unicorn that also does your taxes. I’ve been on atorvastatin for 3 years and my HbA1c crept up from 5.6 to 6.1. Switched last month. Three months in, it’s back to 5.5. No drama. No crash. Just quiet, effective science. Thank you for writing this.
I’ve been telling my patients this for years but no one listens until their numbers go sideways. Pitavastatin isn’t magic-it’s just smarter. For prediabetics, it’s the only statin I’ll prescribe now. No fluff. No hype. Just data. And yes, I know it costs more. But how much does a diabetes diagnosis cost? Try 20x more in meds, tests, and lost productivity.
EVERYTHING YOU’RE TOLD IS A LIE. PITAVASTATIN IS A PHARMA TRAP. THEY WANT YOU TO THINK IT’S SAFE SO YOU’LL KEEP TAKING IT WHILE THEY SLIP IN THE REAL TOXIN-INSULIN RESISTANCE THROUGH MICROPLASTICS IN THE PILLS. THE 2022 STUDY? FUNDED BY KOWA. THE CLAMP TEST? DESIGNED TO IGNORE GUT MICROBIOME DISRUPTION. THEY’RE HIDING THE TRUTH. ASK WHY THE FDA APPROVED IT IN 2009-THE SAME YEAR THE DIABETES EPIDEMIC EXPLODED. COINCIDENCE? I THINK NOT.
So let me get this straight-we’re supposed to be grateful that one statin doesn’t *completely* wreck our metabolism? Like, wow. Groundbreaking. Next you’ll tell me water doesn’t drown people if you drink it slowly. I’m just here waiting for the day we stop treating metabolic health like a side note and start treating it like the damn foundation.
this is so helpfull but i dont get one thing why not pravastatin its cheeper and same effect? or am i missin somthing? thx
The pharmacokinetic profile of pitavastatin-specifically, its dual hepatic and renal clearance pathways-renders it significantly less susceptible to CYP450-mediated drug interactions, thereby minimizing off-target metabolic perturbations. This distinguishes it from statins with exclusive CYP3A4 metabolism, which exhibit greater potential for insulin receptor downregulation via altered membrane cholesterol dynamics.
I was skeptical at first. But after switching my dad from rosuvastatin to pitavastatin, his HbA1c didn’t just stop rising-it actually dropped 0.3%. He’s 68, overweight, prediabetic. We didn’t change his diet. Just the pill. I’m telling you, this isn’t just theory. It’s real life.
I’ve seen this before. Someone writes a long article about how one drug is ‘better’-and then the next week, someone has a heart attack because they switched and stopped monitoring. You’re not a doctor. You’re not even a nurse. You’re just some guy with a blog. Don’t let your fear of cost blind you to the fact that 90% of people who stop statins die younger. PITAVASTATIN ISN’T A MAGIC BULLET-IT’S STILL A DRUG. AND DRUGS HAVE RISKS. DON’T BE A FOOL.
Bro in India we barely have access to any statins. My uncle got pitavastatin through a WHO program last year. He’s diabetic, had high LDL, and now his numbers are stable. No side effects. No drama. Honestly, if this drug works this well in places with bad healthcare, imagine what it can do in the US. We need to push for global access-not just for the rich.
Thank you for including the cost and insurance context. That’s the missing piece in 99% of these discussions. Pitavastatin’s metabolic profile is compelling, but without addressing access, it’s academic. The fact that Medicare Part D covers it as tier 2-and that patient assistance programs exist-is critical. This isn’t just clinical advice; it’s socioeconomic advocacy.
Akshaya asked why not pravastatin? Good question. Pitavastatin 2-4mg lowers LDL by 35-50%. Pravastatin 40mg? Only 20-30%. So you’d need double the dose to get the same cholesterol drop-and pravastatin’s still not as clean in head-to-head trials. Plus, pitavastatin’s half-life lets you take it anytime, day or night. Pravastatin? Best at night. For busy people? Pitavastatin wins on convenience too.