Insulin isn’t like other medications. If it’s stored wrong, it stops working - and that can be dangerous. People with diabetes rely on insulin to keep their blood sugar stable. When insulin loses potency, blood sugar levels spike or crash without warning. That’s not just inconvenient - it can lead to hospital visits, diabetic ketoacidosis, or worse. The FDA, American Diabetes Association, and other health groups agree: proper storage isn’t optional. It’s part of your daily diabetes management.
Insulin is a protein. Heat, cold, and light break it down. Once that happens, your body doesn’t get the full dose. You might think you’re taking 10 units, but you’re really getting 7. That’s why people report unexplained high blood sugars - and often, the culprit is old or mishandled insulin.
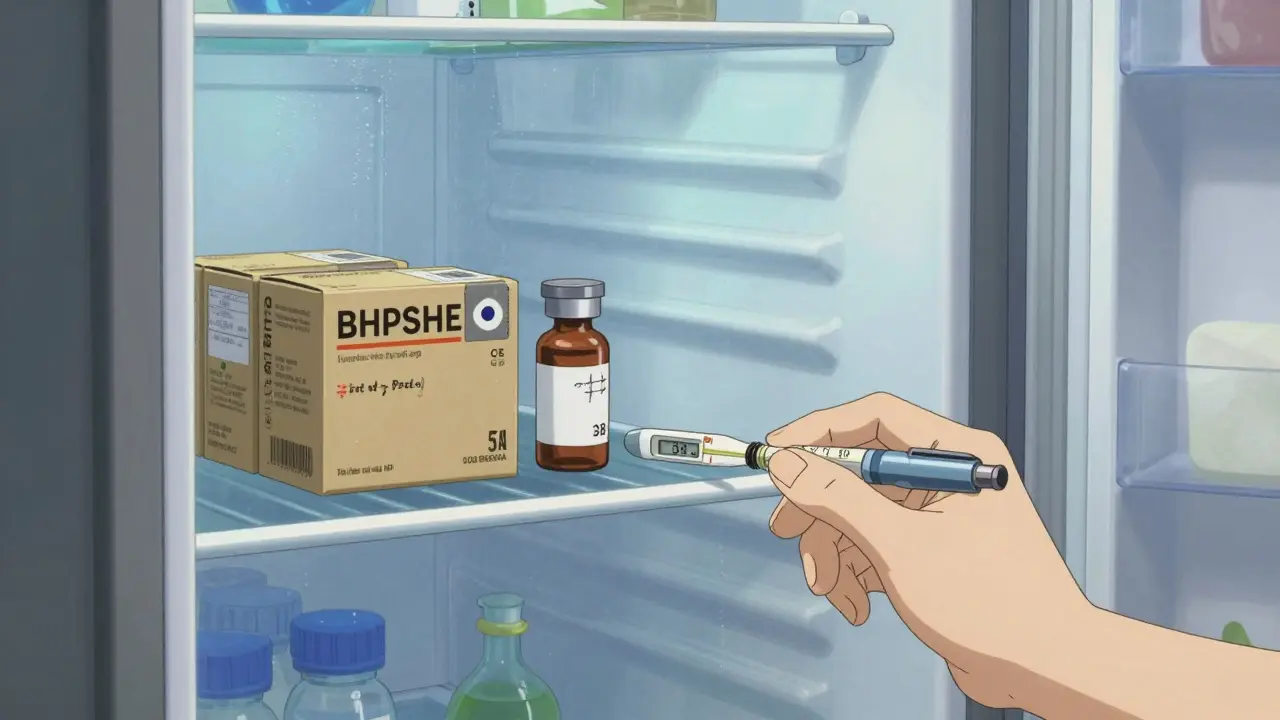
Before you open a new vial, pen, or cartridge, it needs to stay refrigerated. The sweet spot is between 36°F and 46°F (2°C to 8°C). That’s the temperature of your fridge’s main compartment - not the door, not the freezer. Storing insulin on the fridge door exposes it to temperature swings every time you open it. Freezing it is even worse. Frozen insulin forms crystals inside. Once that happens, no amount of thawing brings it back. You’ll see clumps or particles. If you notice that, throw it out.
Check your fridge’s temperature with a small thermometer. About 12% of home fridges have spots colder than 32°F, especially near the back wall or freezer compartment. Move insulin to the middle shelf, away from ice makers or cooling vents. Always keep unopened insulin in its original box. The cardboard protects it from light, which can also degrade the medication.
Once you start using insulin, you can keep it at room temperature. Most types last 28 days at 59°F to 86°F (15°C to 30°C). That’s true for most pens and vials from Eli Lilly, Novo Nordisk, and Sanofi. But there are exceptions.
Don’t guess. Check the package insert or ask your pharmacist. If you’re unsure, assume 28 days. Mark the date you opened it on the pen or vial with a permanent marker. A University of Michigan study found this simple step cut usage beyond expiration by 68%.
If you use an insulin pump, your rules change. Once you fill the reservoir, the insulin inside must be replaced every 72 hours - no exceptions. Even if it’s still within the 28-day window, pump insulin degrades faster because it’s exposed to air and movement. The same goes for the tubing and infusion set.
And if the pump or reservoir gets too hot - say, left in a car on a summer day - throw it out immediately. The American Diabetes Association says pump insulin exposed to temperatures above 98.6°F (37°C) loses effectiveness fast. You can’t rely on time limits here. Heat = trash.

You might not notice right away. But over time, your blood sugar becomes harder to control. You’ll need more insulin to get the same effect. Or worse - you get high blood sugar with no obvious reason.
Dr. Robert Gabbay of the American Diabetes Association says improperly stored insulin causes about 17% of unexplained blood sugar swings in insulin users. In one Reddit thread, a user lost $380 worth of insulin after their fridge broke. Their blood sugar went wild for days. They didn’t realize the problem until they checked the fridge thermometer.
Cloudy insulin that’s supposed to be clear? Toss it. Visible particles? Toss it. Insulin left in a hot car? Toss it. It’s not worth the risk.
Traveling doesn’t mean giving up safe storage. Airplanes, cars, and hotels can be extreme environments. Never pack insulin in checked luggage. The cargo hold can drop below freezing or soar above 100°F.
Use an insulated case. Popular options like the Frio Wallet use evaporative cooling - no batteries needed. They keep insulin below 86°F for up to 45 hours, even in 100°F heat. Other brands use phase-change gel packs. These cost $25 to $50, but they’re cheaper than replacing spoiled insulin.
If you’re flying, carry a doctor’s note and keep insulin in your carry-on. TSA allows insulin and supplies through security without restriction. Keep it in its original packaging with labels visible.
Power outages, natural disasters, or travel mishaps happen. The FDA updated its emergency guidance in August 2023: if refrigeration isn’t available, most insulin stays effective for up to 28 days at 86°F or lower. But after that, potency drops fast. At 95°F, insulin loses 35% of its strength in just 7 days.
Don’t wait until it’s too late. If you’re in a heatwave or without power, use insulin as soon as possible. Prioritize using the oldest opened vial or pen first. If you’re unsure whether it’s still good, err on the side of caution. Get a replacement as soon as you can.
A 2022 survey by the American Association of Diabetes Educators found that 33% of insulin users store it in places like glove compartments or nightstands - spots that get too hot. And 41% don’t check expiration dates regularly. These habits cost lives - and money. In the U.S. alone, improper storage leads to $1.2 billion in wasted insulin and related healthcare costs each year.
Most insulin should look clear and colorless. Some types, like NPH, are cloudy but should be uniformly mixed - no clumps or floating particles. If you see:
…then it’s damaged. Don’t use it. Even if it’s within the 28-day window, if it looks off, throw it away.
Also, pay attention to your body. If you’re taking the same dose but your blood sugar is higher than usual, suspect bad insulin. Test with a new vial or pen to confirm.
Never toss used insulin pens, needles, or vials in the regular trash. Most states require sharps disposal in approved containers. Many pharmacies and hospitals offer free sharps disposal programs. You can also buy FDA-cleared sharps containers online for under $15.
For unused insulin that’s expired or damaged: don’t pour it down the drain. Return it to a pharmacy that takes expired medications. Some cities have drug take-back events. Check with your local health department.
Good news: newer insulins are more stable. Sanofi’s Toujeo can last 56 days at room temperature. Biocon and other manufacturers are developing formulations that can handle heat better - some even staying effective at 104°F for 14 days. By 2027, most new insulins will have 35+ days of room temperature stability.
This isn’t just convenience. It’s access. In low-income countries, 53% of insulin distribution lacks temperature control. More stable insulins could save lives where refrigeration is rare.
Store insulin like you store your phone - with care and consistency. Make a checklist:
It’s not about being perfect. It’s about being aware. One mistake can throw off your blood sugar for days. But with a few simple habits, you can avoid the risks and keep your insulin working exactly as it should.
No. The fridge door gets too warm and cold with each opening. Store insulin on a middle shelf where the temperature stays steady between 36°F and 46°F.
Most insulin lasts 28 days at room temperature (59°F to 86°F). But check the label - NPH lasts 14 days, Tresiba lasts 8 weeks, and Toujeo lasts 56 days. When in doubt, use 28 days.
Throw it out. Freezing damages the insulin’s structure permanently. Even if it thaws and looks normal, it won’t work correctly. Never use frozen insulin.
No. Inside a car on a 75°F day can reach over 100°F in 30 minutes. Insulin exposed to temperatures above 86°F begins losing potency. If it’s been in a hot car, discard it - even if it’s still within the 28-day window.
Yes. Cold insulin can hurt more when injected. Let refrigerated insulin sit at room temperature for 30 minutes before use. It won’t affect how long it lasts - just how comfortable the shot feels.
Place used needles and pens in a sharps container - not the regular trash. Many pharmacies offer free disposal programs. You can also buy FDA-approved containers online. Never recycle or flush them.
No. Even if refrigerated, insulin loses effectiveness after the printed expiration date. Don’t risk it. Use only insulin within its labeled shelf life.
Switch to a new, unopened vial or pen. If your blood sugar improves, the old insulin was likely damaged. Check storage conditions, look for cloudiness, and note if it was exposed to heat or cold. Report it to your doctor.
I can't believe people still leave insulin in the car. That's not negligence, that's a death sentence waiting to happen. You wouldn't leave baby formula in a hot trunk, so why the hell would you do this with life-saving medication? If you're this careless, maybe you shouldn't be managing diabetes at all.
This is one of those posts that makes you pause. I've seen friends struggle with insulin storage because they didn't know any better. It's not about blame-it's about access. Not everyone has a reliable fridge, or knows what 'room temperature' actually means. Maybe we need community programs that hand out cheap thermometer strips and storage kits. A little education goes a long way.
I used to store my insulin in the fridge door because it was convenient until my BG went nuts for three days. Turned out the fridge was running at 50°F on the door and freezing the insulin. Now I keep a little thermometer next to it and mark every pen with a sharpie. Game changer. Also-yes, let it warm up before injecting. Cold shots feel like needles stabbing your thigh. Not fun.
I just want to say-thank you-for including the part about disposal. So many people don't know you can't just toss needles in the trash. I had a neighbor who did that, and then complained about the 'dirty needles' in the dumpster. I gave her a free sharps container from my pharmacy. It's not complicated. It's just... basic human decency.
The phrase 'room temperature' is misleading. Technically, room temperature is 20–22°C, yet the FDA permits up to 30°C. This is sloppy terminology. Furthermore, the claim that 'Toujeo lasts 56 days' is only true under controlled laboratory conditions. Real-world environments-especially in humid climates-degrade insulin faster. The FDA's guidelines are minimums, not recommendations. Precision matters.
I'm from India and we don't always have AC or reliable fridges. I use a Frio wallet when I travel and it's been a lifesaver. Also, I started putting my insulin in a small insulated lunchbox with a cold pack when I'm out all day. No fancy tech, just common sense. And yes, I use emojis sometimes because I'm emotional about this stuff 😔💉
So let me get this straight-you're telling me I can't just keep my insulin in my pocket while I'm at the gym? Like, I've been doing that for years. Are you saying I've been poisoning myself? 😅
You know what's worse than bad insulin? People who think they're experts because they read a blog. I've had diabetes for 22 years and I've seen insulin go bad in the fridge because someone left it next to the ice maker. And then they blame the manufacturer. No. It's not the brand. It's the person. You think you're saving money by reusing needles? You're just inviting MRSA into your bloodstream. And don't even get me started on people who think 'it still looks clear' means it's fine. Look at the date. Check the temp. Stop being lazy.
I used to forget to mark my pens until I ran out mid-week and had to borrow from my sister. Ended up giving her my expired one by accident. Now I write the date on the cap with a Sharpie and keep a sticky note on the fridge. Simple. Dumb. Works.
It's interesting how we treat insulin like a fragile object, yet we treat the people who need it like disposable. The real crisis isn't just storage-it's cost. If insulin weren't $300 a vial, people wouldn't risk using expired doses. We talk about temperature control like it's a personal failure, but what about systemic failure? Maybe the real question isn't 'how do we store it?' but 'why does it have to be so hard to get?'
