This tool uses the Barnes Akathisia Rating Scale (BARS), a clinically validated assessment for akathisia. Answer 5 questions based on your symptoms to get an accurate score. If your score is 5 or higher, consider discussing with your doctor.
This tool is for self-assessment only. A score of 5 or higher suggests akathisia, but only a medical professional can diagnose this condition. If you scored 5 or above, consult your doctor immediately.
Akathisia is often misdiagnosed as anxiety. If you're experiencing these symptoms, bring this tool's results to your healthcare provider.
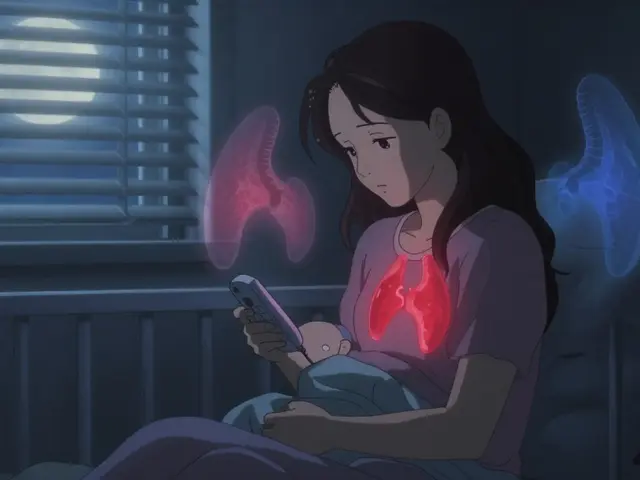
Imagine sitting in your chair, legs trembling, chest tight, mind racing. You can’t sit still. You stand up, pace, sit back down, cross and uncross your legs. Your doctor says, "It’s anxiety." You’re given more antidepressants. The restlessness gets worse. You feel like you’re losing your mind. But it’s not anxiety. It’s akathisia-a medication-induced movement disorder that’s been misdiagnosed for decades.
Thousands of people on antipsychotics, anti-nausea drugs, or even some antidepressants experience this. And most don’t know what’s happening. They’re told they’re "overreacting," "not coping," or "needing a higher dose." But the truth? Their body is reacting to the medicine itself.
People often confuse akathisia with restless legs syndrome (RLS). Both make you want to move your legs. But they’re not the same.
Akathisia feels like an inner storm. You don’t just want to move your legs-you feel like you have to move everything. Your arms twitch. Your feet tap. You rock back and forth. You can’t sit still, even if you’re trying. It’s not just discomfort-it’s unbearable. One patient described it as, "You ache with restlessness, so you feel you have to walk. And then as soon as you start pacing, you must sit. Back and forth. No relief."
Restless legs syndrome is different. It’s a physical urge, mostly at night or when you’re resting. It’s tied to low iron or genetics. Movement helps. You can sleep through it if you get up and walk. Akathisia? No amount of walking fixes it. It’s worse when you’re still. And it starts after you begin or increase a medication.
Here’s the kicker: drugs that help RLS-like levodopa-can make akathisia worse. Beta-blockers like propranolol? They help akathisia. Not RLS. If your doctor prescribes something that makes it worse, that’s a red flag.
Akathisia isn’t rare. About 20-40% of people on older antipsychotics like haloperidol develop it. Even newer ones like risperidone can cause it in up to 14% of users. But it’s not just antipsychotics.
It doesn’t take long. Symptoms usually show up within days to four weeks of starting or increasing the dose. Sometimes, they appear after you stop the drug-that’s withdrawal akathisia. And if it lasts more than six months? That’s chronic akathisia. It can stick around even after you stop the medicine.
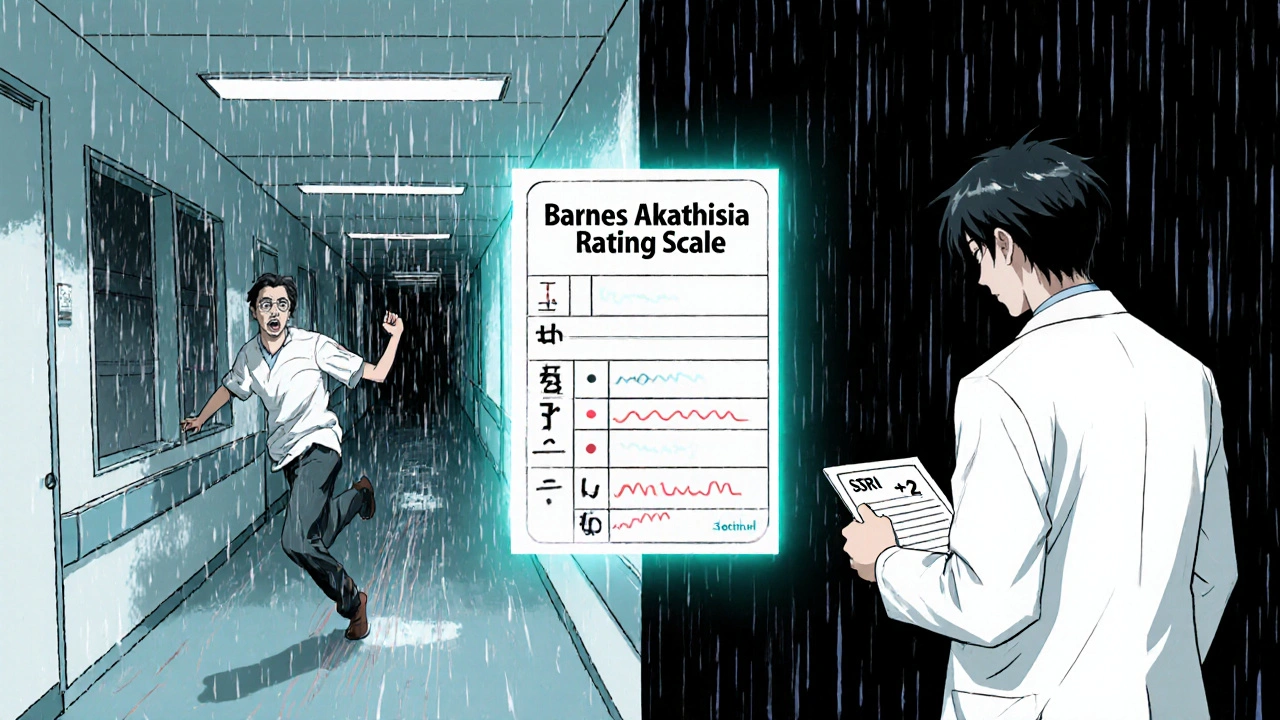
When a doctor mistakes akathisia for anxiety, they often do the worst thing possible: increase the dose of the drug causing it.
That’s what happened to a patient in a 2017 case study. Her doctor doubled her haloperidol because she "seemed more agitated." Within days, she had suicidal thoughts. Only after she found akathisia online and demanded a change did she get relief.
Studies show up to half of akathisia cases are misdiagnosed. The American Psychiatric Association warns this can lead to aggression, violence, or suicide. Why? Because the inner torment of akathisia is so intense, some patients say they’d rather have untreated psychosis than keep living with it.
And it’s not just psychiatric patients. Elderly people on metoclopramide for nausea, or even someone on an SSRI for depression, can develop it. Primary care doctors rarely screen for it. That’s why so many suffer in silence.
You don’t need a fancy test. Here’s what to look for:
If you answer yes to most of these, you’re likely dealing with akathisia. Use the Barnes Akathisia Rating Scale (BARS)-a simple 4-point tool doctors can use in under 10 minutes. Ask yourself: "Do I feel an inner restlessness that makes me need to move?" If the answer is yes, bring this up with your doctor.
Step one: Don’t panic. But don’t ignore it either.
1. Talk to your doctor about the medication. Ask: "Could this be akathisia?" Bring the checklist above. Many doctors haven’t been trained to recognize it.
2. Don’t stop cold turkey. Abruptly quitting antipsychotics or anti-nausea drugs can trigger withdrawal akathisia or worsen psychosis. Work with your doctor to taper slowly-sometimes over 3-7 days.
3. Ask about add-on treatments. If you need to stay on the medication, these can help:
These aren’t cures-they’re bridges. The goal is to reduce the dose of the drug causing it.
4. Rule out other causes. Make sure it’s not Parkinson’s (tremors, stiffness) or tardive dyskinesia (involuntary lip-smacking, tongue movements). These are different, but can happen together.

There’s real progress. In 2023, a new drug called pimavanserin (Nuplazid), originally for Parkinson’s hallucinations, showed 62% reduction in akathisia symptoms in a clinical trial. It’s not approved for this yet, but doctors are using it off-label.
Harvard is testing transcranial magnetic stimulation (TMS)-a non-invasive brain therapy-to calm the overactive circuits causing the restlessness. Early results are promising.
And tech is helping. The International Parkinson and Movement Disorder Society launched an app in 2023 that guides clinicians through diagnosis using video analysis. Stanford’s AI system can detect akathisia from a 1-minute video call with 89% accuracy. That’s huge for telehealth patients.
If you’re on any of these meds and feel restless:
Don’t wait. The sooner you act, the faster you’ll feel better. In the 2017 RACGP case study, one patient was back to normal in three days after stopping haloperidol and starting clonazepam.
Akathisia isn’t just a personal problem. It’s a system failure. Only 37% of U.S. psychiatric clinics screen for it. The FDA required warnings on antipsychotics in 2008-but many prescribers still don’t know the signs.
Every time someone is misdiagnosed, it’s not just a mistake-it’s a risk to their life. The distress of akathisia is worse than the psychosis it was meant to treat. And it’s preventable.
If you’ve been through this, your voice matters. Talk about it. Share your story. Push for better screening. Because no one should have to suffer in silence-especially when the fix might be as simple as lowering a dose or switching a pill.
Yes, but only if the triggering medication is reduced or stopped. Akathisia doesn’t resolve on its own while you’re still taking the drug. In many cases, symptoms improve within days of lowering the dose. If it’s acute (less than 6 months), stopping the medication usually leads to full recovery. Chronic akathisia can linger, but even then, switching to a lower-risk drug or adding a treatment like propranolol often helps.
No. While both can cause restlessness, anxiety is primarily a mental state-fear, worry, racing thoughts. Akathisia is a physical movement disorder caused by brain chemistry changes from medication. You can feel anxious without moving constantly. With akathisia, you can’t stop moving, even if you’re calm. The key difference? Anxiety meds won’t fix akathisia. In fact, they often make it worse.
Yes. SSRIs like fluoxetine, sertraline, and paroxetine are known to trigger akathisia, especially when started or increased quickly. It’s less common than with antipsychotics, but still happens in up to 10% of users. If you started an SSRI and suddenly feel an urgent need to move, pace, or rock back and forth, it could be akathisia-not a sign your depression is getting worse.
There’s no blood test or scan. Diagnosis is based on clinical signs and timing. The Barnes Akathisia Rating Scale (BARS) is the gold standard-it’s a short questionnaire doctors use to rate your inner restlessness and visible movements. If you can show your doctor a clear timeline linking symptoms to a medication change, and rule out other conditions, that’s usually enough. Bring a symptom log and describe your movements exactly.
Sometimes, yes. If your psychiatric condition is severe and you can’t stop the medication, your doctor may add a treatment like propranolol or clonazepam to manage the akathisia. This is called "add-on therapy." But the goal is still to reduce the antipsychotic dose over time if possible. Some newer antipsychotics like lumateperone have much lower akathisia rates and may be a better long-term option.
Acute akathisia usually improves within days to weeks after stopping the drug. For some, it’s gone in 3 days. Chronic akathisia can last months or longer, especially if it was untreated for a while. Tardive akathisia may persist even after stopping the medication for years. Early intervention is key-the sooner you act, the faster you recover.
I thought I was just anxious until I read this. My doctor kept upping my sertraline and I felt like I was going to crawl out of my skin. Turned out it was akathisia. Took me six months to find someone who knew what it was.
Propranolol saved me. 10mg twice a day. Not a cure, but a lifeline. I still get the urge to move, but now I can sit through a movie.
This is absolute nonsense. You're blaming medication for your own weakness. If you can't handle a little restlessness, maybe you shouldn't be on psychiatric drugs at all. My uncle was on haloperidol for 20 years and never had this "inner storm" nonsense.
I spent 18 months being told I was "just depressed" while my body screamed for movement. I'd pace the kitchen at 3am, hands shaking, heart pounding - and my psychiatrist said, "Try journaling."
It wasn't anxiety. It was my dopamine receptors screaming in protest. The moment I stopped the SSRI and started propranolol? I cried for an hour because I could finally sit still without wanting to rip my skin off.
This isn't just medical ignorance - it's a crisis. And if you're reading this and feel this way? You're not broken. The system is.
Man, I wish I'd known this back when I was on risperidone. I thought I was losing it. I'd bounce my knee so hard my leg hurt. My wife thought I was being rude. Turns out I was in hell and nobody had the map.
Propranolol? Yeah, it worked like magic. Didn't fix everything, but it gave me back my sanity. And now I tell every new patient I meet: "If you feel like your bones are buzzing, ask about akathisia."
I've seen this too many times. Doctor gives SSRI. Patient gets restless. Doctor increases dose. Patient gets suicidal. Doctor says "it's just adjustment period."
It's not. It's a known, documented, FDA-recognized side effect - and yet, 90% of GPs can't name it. The Barnes Scale? It's free. It takes 5 minutes. Why aren't we using it?
And yes - antidepressants absolutely cause this. Especially sertraline and fluoxetine. Don't let anyone tell you otherwise.
They're lying. Akathisia doesn't exist. It's a scam by Big Pharma to sell more drugs. They want you to think your meds are the problem so you'll switch to their new expensive pills. The real cause? Stress. Or maybe you're just lazy.
Also - why do you think your body "reacts" to medicine? Everything is medicine. Even water. You're just weak.
And that "app"? That's how they track you. Watch your phone. They're listening.
The clinical evidence is robust: akathisia is a well-documented extrapyramidal symptom, primarily associated with dopamine receptor antagonism. The temporal relationship between medication initiation or dose escalation and symptom onset is statistically significant (p<0.001) in multiple prospective cohort studies.
Furthermore, the efficacy of beta-blockers in mitigating akathisia has been demonstrated in randomized, double-blind, placebo-controlled trials, with propranolol achieving a mean reduction of 4.2 points on the Barnes Akathisia Rating Scale.
It is imperative that clinicians be educated on this phenomenon to prevent iatrogenic harm.
Oh wow. Another person who thinks their feelings are more important than medical science. You're not special. Everyone on these meds feels "restless" sometimes. You're just dramatic.
And you want to stop your antipsychotic? Good. Go off it. See how long you last without it. Then come back when you're not crying about your "inner storm."
Also - propranolol? That's for heart patients. You think your brain is a car engine? It's not.
I had this. For two years. Thought I was broken. My wife left me because she thought I was "unstable."
Then I found a movement disorder specialist. She looked at me, asked one question - "When did this start?" - and said, "That's akathisia."
Three days after lowering my dose and adding clonazepam? I slept for the first time in 700 days.
Don't give up. Find the right doctor. It's not your fault.
I didn't believe it either until I saw my own video. I recorded myself sitting still for 2 minutes. I didn't even realize I was rocking. My foot was tapping like a drum. My arms were twitching. I looked like a robot glitching.
My doctor said "it's anxiety." I cried. I went home. I googled. I found this article.
Propranolol 10mg. Two days later - I could sit on the couch without wanting to scream.
Thank you for writing this. I'm not alone.
This is an excellent, well-researched summary. The key takeaway: timing is everything. If symptoms emerge within 4 weeks of a medication change, akathisia must be ruled out.
And while the treatments mentioned are helpful, the real solution is prevention - better prescriber education, routine screening, and patient empowerment.
Thank you for bringing this to light. This needs to be in every medical school curriculum.
So let me get this straight - you're telling me the government and Big Pharma are poisoning people with antidepressants so they can sell more drugs?
And you're surprised Americans are restless? We're a nation of overworked, under-slept, sugar-chugging zombies. Maybe stop blaming pills and start blaming the system.
Also - propranolol? That's a beta-blocker. You think your brain is a baseball game? Chill out.
I had akathisia for 3 years. My husband left me. My mom said I was faking it. I lost my job. I tried everything.
Then I found a Reddit thread. I cried for 4 hours.
Now I have a support group of 200 people. We share our stories. We fight doctors together.
You think you're alone? You're not. I'm here. We're here. And we're not going silent anymore.
This is so important 💙
My sister had this after starting fluoxetine. They kept saying "it's just anxiety" - until she tried to jump out of a window.
Propranolol fixed it. She's back to painting, cooking, laughing.
Everyone needs to read this. Please share it with your doctor. Even if they roll their eyes. Just say: "I read this. Can we check?" 💪
I find it deeply concerning that this article, while ostensibly well-intentioned, perpetuates a dangerous narrative of pharmaceutical distrust. Akathisia, while real, is exceedingly rare in properly managed clinical settings. The majority of cases cited appear to stem from non-compliance, self-medication, or psychological suggestion.
Furthermore, the suggestion that beta-blockers are a "bridge" to discontinuation implies that antipsychotics are inherently toxic - a view that contradicts decades of clinical evidence.
One must be cautious not to conflate transient discomfort with pathological disorder.