
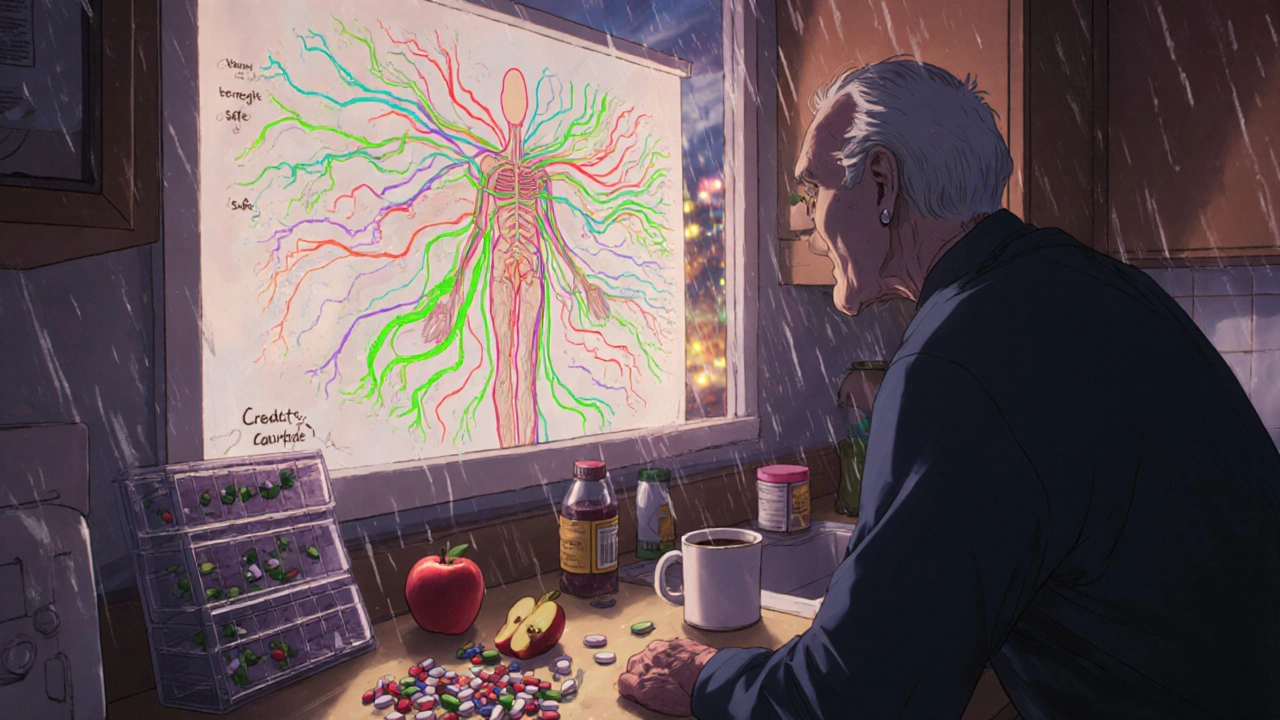
When you’re taking a medication, you expect some side effects - maybe a dry mouth, a bit of dizziness, or an upset stomach. But if you have other health conditions, those side effects can turn dangerous. It’s not just about the drug. It’s about your body’s overall state. People with multiple chronic illnesses are far more likely to suffer serious reactions, sometimes life-threatening ones. And it’s happening more often than most people realize.

Yes. Even a single medication can become risky if your body’s ability to process it is impaired. For example, someone with mild kidney disease might experience severe dizziness from a standard dose of a blood pressure pill that’s perfectly safe for someone with healthy kidneys. The problem isn’t the number of drugs - it’s how your conditions change how your body handles them.
Not always. Common OTC drugs like ibuprofen, naproxen, antacids with aluminum, or even cold medicines with pseudoephedrine can be dangerous. For example, NSAIDs can cause kidney failure in people with diabetes or high blood pressure. Antihistamines can cause confusion in those with dementia. Always check with your pharmacist before taking anything, even if it’s sold without a prescription.
Many doctors aren’t trained to handle complex polypharmacy. They’re under time pressure, and they often rely on guidelines that don’t account for multiple conditions. Also, some drugs are prescribed to treat side effects of other drugs - creating a cascade. For example, a statin causes muscle pain, so a muscle relaxant is added, which causes drowsiness, so a stimulant is prescribed. Each step adds risk. It’s not negligence - it’s a system that wasn’t built for today’s patients.
Look for new symptoms within days or weeks of starting a new drug - especially weakness, confusion, dizziness, nausea, or changes in heart rate or urination. If you’ve recently added a medication or changed a dose, and you feel worse, it could be an interaction. Don’t ignore it. Write down the timing and symptoms and bring them to your provider. Early detection can prevent hospitalization.
Never stop a prescribed medication without talking to your doctor. Some drugs - like blood pressure pills, antidepressants, or steroids - can cause serious withdrawal effects if stopped suddenly. But you can and should ask: “Is this still necessary?” and “Could it be interacting with my other conditions?” Your provider may be able to adjust the dose, switch to a safer alternative, or stop it safely under supervision.
So let me get this straight - we’re telling people with five chronic conditions to just ‘ask their doctor’ like that’s some magic wand? My grandma’s doctor barely remembers her name, let alone what 12 different pills are for. This whole system is a dumpster fire wrapped in a prescription pad.
The body isn’t a machine with separate parts. It’s a conversation - and we’ve been shouting over each other with pills.
Of course the FDA doesn’t test on real people. They test on the kind of people who can afford to be healthy - white, young, and legally compliant. Meanwhile, the rest of us are guinea pigs in a pharma-funded game of Russian roulette with our own organs. The system isn’t broken. It’s designed this way.
This is a critical issue, especially in countries where access to pharmacists is limited. Many patients don’t even know what their medications are for. Education and simple tools like printed med lists can save lives - but only if they’re made accessible.
Stop pretending this is about ‘patient safety.’ It’s about profit. If drugs were truly safe for comorbid patients, Big Pharma would’ve tested them on them. But then they’d have to admit half their products are dangerous for the people who need them most. So they just keep selling.
I’ve seen this firsthand with my uncle. He was on eight medications for diabetes, heart disease, and depression. Then he started falling, getting confused, and his doctor just added another pill for the dizziness. It wasn’t until his daughter insisted on a med review that they realized three of those drugs were canceling each other out - and two were making his kidneys shut down. It took six months and a near-death experience to fix it. No one was malicious. Everyone was just following protocol. That’s the tragedy.
We treat disease like it’s a list of checkboxes. Diabetes? Check. Hypertension? Check. Depression? Check. But we never ask - what happens when the body, this ancient, intricate, self-regulating organism, is forced to hold all these chemical imbalances at once? We don’t heal systems. We patch symptoms with more chemicals. And then we wonder why the house collapses.
It’s not just about the drugs - it’s about how we define ‘normal.’ If your body doesn’t match the clinical trial profile, you’re not ‘abnormal’ - you’re just invisible to the system. The NIH’s new database is a step forward, but we need to demand that every prescription comes with a disclaimer: ‘This was not tested on people like you.’ And then we need to force the system to change.
Patients must take responsibility. If you're on five medications, you're not a victim - you're a participant. You need to educate yourself. Read the inserts. Ask questions. Don't rely on a doctor who spends seven minutes with you. Your health is your responsibility.
My aunt took ibuprofen for her arthritis and ended up in the ER with kidney failure. She didn’t even know it was dangerous. 😔 So yeah - OTC doesn’t mean ‘safe.’ Always check. Always ask. Even if it’s just a cold pill.
the fda is a joke theyre owned by big pharma and they only test on healthy white people and then sell the drugs to everyone else like its a lottery and the rest of us are just the losers who get the bad numbers and then they wonder why people die in their sleep from a tylenol
Western medicine is a colonial scam. In Nigeria we have grandmothers who cure diabetes with herbs and fasting. But you people need a billion-dollar lab to tell you that your body can heal? You’re drowning in pills while the earth gives you the cure. Stop trusting white labs and start listening to your ancestors.
Let’s cut the fluff. The real problem isn’t polypharmacy - it’s the commodification of health. Hospitals are corporations. Doctors are KPI-driven. Patients are revenue streams. The system doesn’t care if you live or die - it cares if you refill your script. That’s the truth. Everything else is just noise.
People who can't manage their own health shouldn't be allowed to take meds. This isn't a medical issue - it's a moral failure. If you're too lazy to keep a med list, then you deserve the consequences. Stop blaming the system. Take responsibility.
My grandpa died from a drug interaction. He was on 7 meds. No one checked. 😔