
Upper airway stimulation (UAS) is a surgical treatment for obstructive sleep apnea that works by gently stimulating the nerve that controls your tongue. Unlike CPAP, which uses a mask and air pressure to keep your airway open, UAS uses a small implant to move your tongue forward while you sleep-preventing it from blocking your throat. This device is called the Inspire system, and it’s been used in over 200,000 people worldwide since getting FDA approval in 2014.
The idea is simple: when you fall asleep, your tongue can relax and fall back, blocking your airway. That’s what causes snoring and breathing pauses. The Inspire device senses when you inhale and sends a tiny electrical pulse to the hypoglossal nerve, which moves your tongue out of the way. It turns off when you exhale, so you don’t feel it all night. No mask. No hose. No noise. Just better sleep.
Not everyone with sleep apnea qualifies. UAS is meant for people who’ve tried CPAP and couldn’t stick with it. About 3 out of 10 people give up on CPAP because it’s uncomfortable, too hot, or just feels claustrophobic. If that sounds familiar, UAS might be an option.
To qualify, you need to meet a few key criteria:
Before you even consider surgery, you’ll need a sleep study done in the last two years and a special endoscopy test while sedated. This lets doctors see exactly where your airway collapses and whether the device will work for your anatomy.
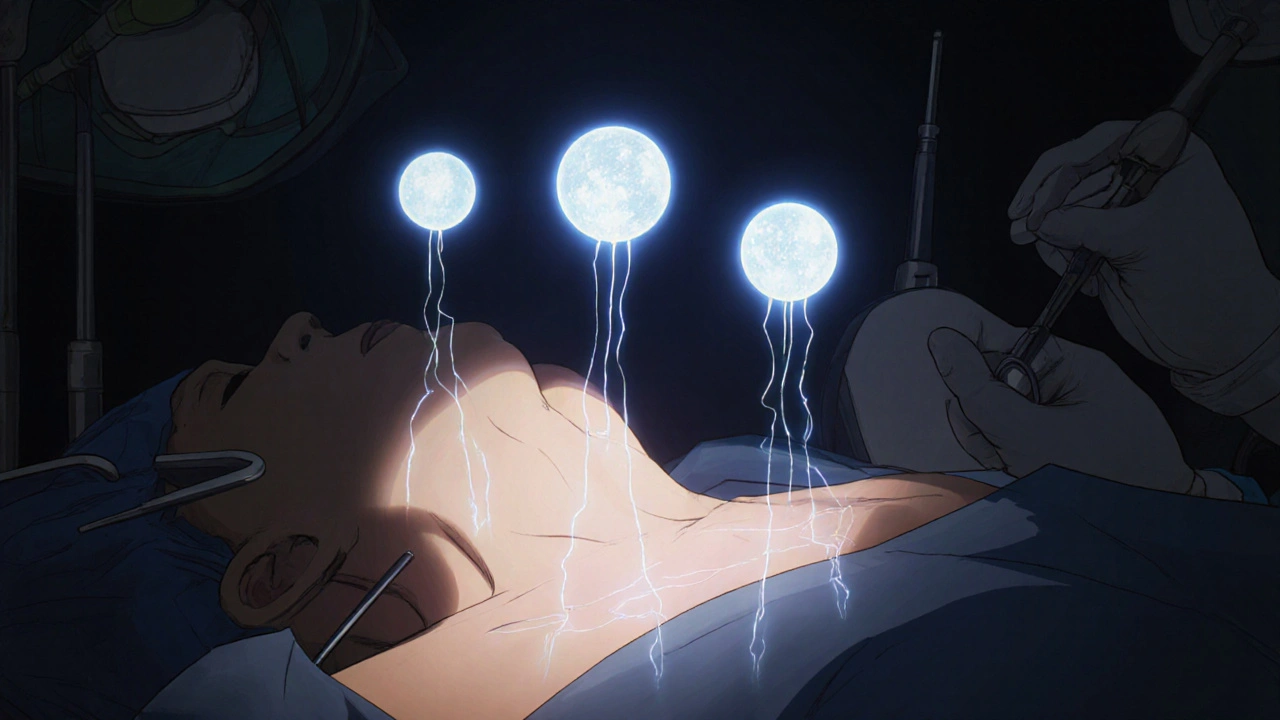
The Inspire system has three tiny parts implanted under your skin:
The surgery takes 2-3 hours and is done as an outpatient procedure. You’ll be under general anesthesia. There are three small incisions: one in your neck to reach the nerve, one lower down to place the breathing sensor, and one near your collarbone for the battery pack. Most people go home the same day.
After about a month of healing, your doctor turns the device on. You’ll get a small remote control-similar to a TV remote-that you use to turn the device on before bed and off when you wake up. It’s not automatic; you have to remember to use it every night. But most patients say it becomes part of their routine, like brushing their teeth.
The numbers speak for themselves. In the main clinical trial (called the STAR trial), patients saw their breathing pauses drop by 68%. On average, AHI went from 29 events per hour down to just 9. That’s a drop from severe to mild sleep apnea for most people.
Two out of three patients had at least a 50% improvement in their symptoms. After five years, those results held steady. In real-world use, 86% of patients say it’s better than CPAP. Bed partners report no snoring or only soft snoring in 85% of cases.
One patient from Birmingham, who asked to remain anonymous, shared: “I used to wake up 10 times a night gasping for air. My wife stopped sleeping in the same room. After Inspire, I haven’t woken up once in two years. We’re back in the same bed-and I actually feel awake during the day.”
Like any surgery, there are risks. But serious complications are rare. Over 99% of patients don’t have major problems. The most common issues are mild:
Some users report a tingling sensation at first. It’s not painful, but it can feel odd. Most get used to it within 2-3 weeks. A few forget to turn the device on-especially on vacation or after a late night. That’s the biggest behavioral hurdle, not the surgery.
Unlike tonsil removal or jaw surgery, this procedure is reversible. If you decide to stop using it, the device can be removed without lasting damage to your airway.
CPAP is still the gold standard-but only if you can use it. Studies show 29-46% of people abandon CPAP within the first year. UAS doesn’t fix all cases, but for those who can’t tolerate CPAP, it’s the next best thing.
Compared to older surgeries like uvulopalatopharyngoplasty (UPPP), UAS is less invasive and more effective. UPPP often requires months of recovery and still fails in up to 60% of cases. UAS improves multiple areas of the airway at once-tongue, soft palate-and has a success rate over 80%.
Oral appliances are another option, but they work best for mild to moderate cases. UAS is designed for moderate to severe sleep apnea. It’s also more reliable than tongue reduction surgery, which carries higher risks of nerve damage and swallowing issues.
The total cost of the Inspire system, including surgery and follow-up, ranges from $35,000 to $40,000. That sounds high-but think about it this way: CPAP machines cost $500-$1,000 upfront, but you’ll need to replace masks, tubing, and filters every few months. Over 5 years, that adds up to $10,000-$15,000. Plus, if CPAP fails, you’re back to square one.
Good news: insurance covers it. In the U.S., 95% of Medicare patients and 85% of private insurers now pay for UAS therapy. Most providers will help you get pre-approval. If you’re denied, you can appeal-many cases get approved on second review.

The FDA expanded eligibility in 2023 to include patients with BMI up to 40 and AHI up to 100. That opened the door for many more people who were previously turned away.
Researchers are working on smaller, longer-lasting batteries and AI tools that can predict who will respond best to the device. One study in 2024 used machine learning to analyze airway scans and correctly predicted treatment success in 92% of cases.
As more doctors get trained in implantation and patient awareness grows, UAS is becoming a standard option-not just a last resort.
On patient forums, stories are consistent:
There are also honest reviews: “It took me a month to get used to turning it on every night. I missed a few times and felt awful the next day. Now I put the remote next to my toothbrush.”
If you’ve struggled with CPAP and still feel tired, it’s time to ask your sleep doctor about UAS. Here’s your roadmap:
Most centers offer free consultations. You don’t have to decide right away. Take your time. Ask questions. Bring your partner. This isn’t just about sleep-it’s about your health, your relationships, and your quality of life.
I tried CPAP for 6 months. Felt like I was wearing a space helmet while trying to sleep. My wife started sleeping on the couch. Then I found out about Inspire. Two years later, we’re back in the same bed. No more midnight gasping. No more 3 p.m. naps. Just… peace. I didn’t think it’d work for me. But sometimes, the thing that sounds crazy is the thing that saves your life.
Let’s be precise: the 68% reduction in AHI is statistically significant, but the sample size in the STAR trial was n=344, with a 12% dropout rate. The long-term efficacy beyond five years remains underpowered. Furthermore, the exclusion criteria-particularly the BMI cap and central apnea threshold-introduce selection bias. This is not a panacea; it’s a niche intervention for a specific phenotype of OSA. Don’t let marketing masquerade as medicine.
Honestly? I was skeptical too. Thought it was sci-fi stuff. But my buddy got it done last year-same age, same BMI, same CPAP trauma. Now he’s hiking weekends, playing with his niece without falling asleep on the couch. I’m not saying it’s magic, but if you’ve been through the CPAP nightmare? It’s the closest thing to a reset button I’ve seen. Talk to your doc. No pressure. Just… maybe.
This gives me so much hope 😊 I’ve been struggling with sleep for years and CPAP felt like a prison. The idea of just turning on a little device before bed… it sounds so simple. I’m scheduling a consultation next week. Thank you for sharing this-it feels like a light at the end of a very long tunnel 🌟
My dad got the Inspire last year. He’s 61, BMI 32, used to snore like a chainsaw. Now he’s up at 6 a.m. making pancakes and actually remembers what he ate for lunch. The only thing he complains about? Forgetting to turn it on after a late night. But hey, better than forgetting to breathe. I’m telling all my friends about this.
bro i got this done last year and honestly?? it changed my life 😍 i used to wake up with my mouth dry and my head pounding. now? i sleep like a baby. the remote is kinda clunky but you get used to it. my wife says i don’t snore anymore and she actually cuddles now 🥲 i didn’t think i’d ever say this but… i’m kinda glad i have a robot in my chest
If you’re reading this and you’re still on CPAP because you’re scared of surgery-stop. This isn’t a gamble. It’s a solution. The data is solid. The success rate is higher than most surgeries people accept without a second thought. Your sleep isn’t optional. Your health isn’t negotiable. Talk to a specialist. Don’t wait until you’re 70 and on three meds just to stay awake.
Ah, the modern age of bio-technological transcendence. We implant devices to correct the consequences of our sedentary, sugar-laden, screen-saturated civilization-while never questioning the root causes. The Inspire system is not a cure. It is a Band-Aid on a hemorrhage. We have traded the tyranny of the mask for the quiet subjugation of the silicon pulse. And yet… we call it progress. But what is progress if we merely outsource our biology to machines? The tongue, that ancient instrument of speech and taste, now reduced to a relay for electromagnetic impulses. We are becoming less human. And we are proud of it.
The hypoglossal nerve stimulation paradigm leverages neuromodulatory pathways to dynamically counteract pharyngeal collapse during the inspiratory phase of the respiratory cycle. The device’s closed-loop feedback system, synchronized with respiratory airflow detection via the sensing lead, enables phase-specific activation-minimizing energy expenditure and enhancing patient compliance. The 86% patient-reported satisfaction metric is clinically meaningful, especially when contextualized against the 46% CPAP non-adherence rate. However, long-term data on lead migration and battery longevity (>10 years) remains limited.
In India, we don’t even have access to CPAP in most villages. But this? This sounds like something from a sci-fi movie. I wish this was available where I’m from. My uncle had sleep apnea and died because no one knew what was wrong. This isn’t just a device-it’s a lifeline. If someone can make this affordable here, they’ll save thousands. Please, someone bring this to the developing world.
So you’re telling me you’d rather cut yourself open and stick a battery in your chest than just lose 20 pounds? 🤦♂️ This is why America is broken. Instead of fixing the cause, you buy a $40k gadget. You want to sleep better? Eat less. Move more. Stop drinking. Stop scrolling before bed. This isn’t innovation. It’s capitalism selling you a fix for a problem you created.
