When your heart arteries are clogged, two main options exist to restore blood flow: PCI and CABG. Both save lives, but they’re not interchangeable. Choosing between them isn’t about which is "better"-it’s about which fits you.
PCI (Percutaneous Coronary Intervention) is a minimally invasive procedure where a thin tube is threaded through an artery in your wrist or groin to reach the blocked heart vessel. A tiny balloon is inflated to open the blockage, then a metal mesh stent-usually coated with medicine-is left behind to keep the artery open. It’s done under local anesthesia. Most people go home the next day.
CABG (Coronary Artery Bypass Grafting) is open-heart surgery. Surgeons take a healthy blood vessel from your leg, arm, or chest and sew it around the blocked coronary artery, creating a detour for blood. This requires general anesthesia, a cut down the center of your chest, and stopping your heart temporarily while a machine keeps you alive. Recovery takes weeks, not days.
Think of PCI like fixing a pothole with asphalt. CABG is building a new highway around it. One is quick and patchy. The other is permanent but invasive.
PCI works best for simple blockages. If you have one or two narrowed arteries, especially in the front of your heart, and you’re not diabetic, PCI often makes sense. It’s the go-to for heart attack patients-time is muscle, and PCI can open a blocked artery in under an hour.
Studies show PCI reduces chest pain and improves quality of life just as well as CABG in low-risk cases. The recovery is faster: most people are back to light work in 3-5 days. If you’re older, have lung disease, or can’t tolerate major surgery, PCI avoids the risks of open-heart procedures.
Modern drug-eluting stents have cut the chance of needing another procedure by more than half compared to older bare-metal stents. Today’s stents keep arteries open in about 90% of cases after five years.
CABG is the gold standard for complex disease. If you have three or more blocked arteries, especially if the main left artery (LAD) is involved, CABG gives you a better shot at living longer.
The FREEDOM trial in 2012 showed diabetic patients with multivessel disease had a 60% higher risk of dying within five years after PCI compared to CABG. That’s not a small difference-it’s life-changing. CABG’s arterial grafts (especially from the chest wall) stay open over 85% of the time after 10 years. Vein grafts from the leg? Only 60-70%. But arterial grafts? They last.
Patients with a high SYNTAX score (a measure of how tangled your blockages are) also do better with CABG. Scores above 32 mean your arteries are severely diseased. In those cases, CABG cuts the risk of another heart attack or repeat procedure by more than half.
And while CABG has a higher stroke risk right after surgery (1.7% vs. 1.0% for PCI), that risk drops fast. Five years out, your chances of being free of chest pain and repeat surgeries are significantly higher with CABG.

PCI feels like a minor procedure. You might feel sore at the wrist or groin, but you can walk within hours. Most people return to normal activities in under a week. You can drive again after 48 hours if you’re not on strong pain meds.
CABG recovery is harder. Your sternum is cut open and wired back together. It takes six to eight weeks to heal. You’ll feel fatigued. Your chest will ache. Some people report memory issues or brain fog for weeks-this affects about 18% of patients, but most recover fully by a year.
Still, long-term quality of life favors CABG. In one study, 92% of CABG patients said their chest pain was gone after a year. Only 85% of PCI patients could say the same. And while 87% of PCI patients were back at work in two weeks, 32% of CABG patients were. But by six months? Nearly everyone in both groups was working again.
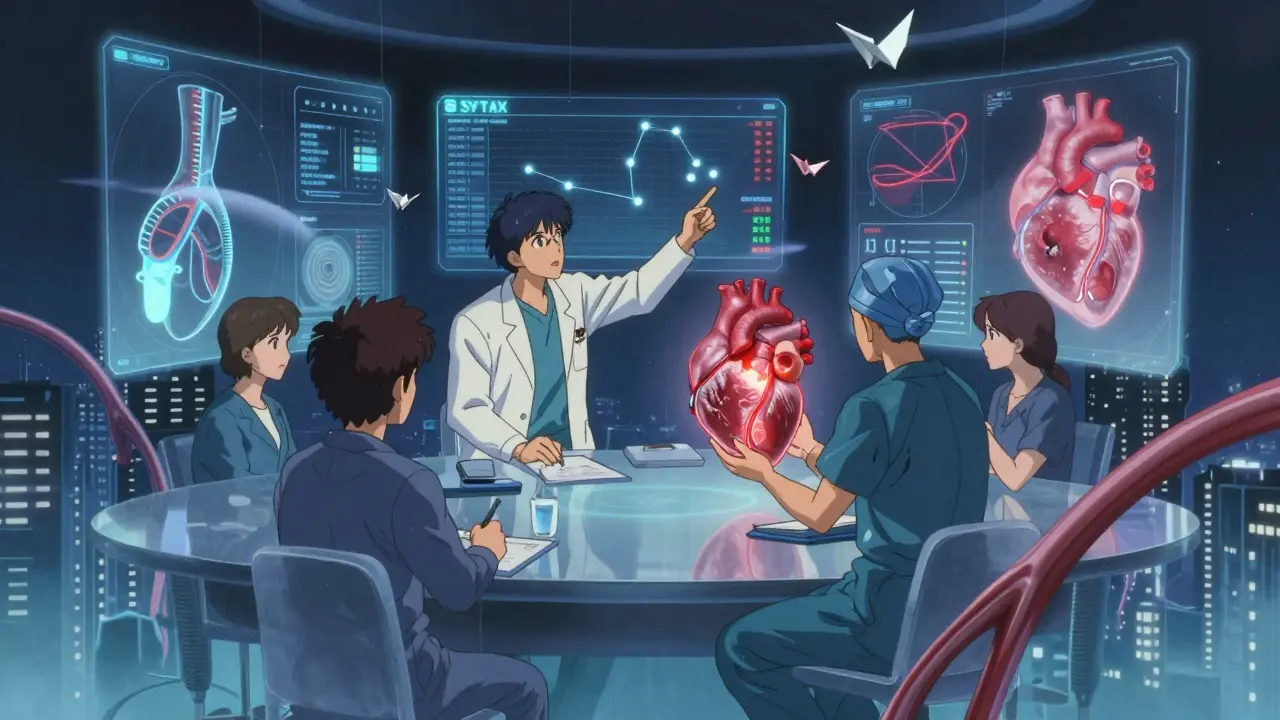
Guidelines now demand a "heart team"-a cardiologist and a cardiac surgeon review your case together. That’s not bureaucracy. It’s science.
One doctor might see a stent as the fastest fix. The other sees a bypass as the lasting solution. Alone, each might push their own tool. Together, they look at your age, diabetes status, kidney function, artery structure, and even your job. A truck driver might need CABG for long-term reliability. A 78-year-old with emphysema might be better off with PCI.
High-volume centers-those doing over 400 PCIs or 200 CABGs a year-have 40% lower death rates. If you’re considering CABG, ask where your surgeon performs most of their cases. Don’t settle for a hospital that does fewer than 50 a year.
Trials compare groups. But your life isn’t a group. You’re one person with one set of arteries, one job, one family.
Some people choose PCI because they can’t take time off work. Others choose CABG because they’ve seen a sibling go through repeat stents and don’t want to live with that uncertainty. One Reddit user wrote: "Six weeks of recovery was tough-but two years later, I’m hiking again with no chest pain." Another said: "Back to work in three days. Needed another stent after 18 months."
There’s no shame in either choice. But if you’re diabetic, have multiple blockages, or your LAD is involved, CABG isn’t just an option-it’s the best chance you have to live longer.
Technology keeps evolving. New stents are thinner, more flexible, and coated with better drugs. Some are even designed to dissolve over time. But so far, none match the durability of an arterial graft.
On the surgical side, robotic-assisted CABG is becoming more common. It uses smaller incisions, reduces blood loss, and can shorten hospital stays. Complete arterial revascularization-using only arteries, never veins-is now being shown to improve 10-year survival by 8%.
And hybrid procedures are on the horizon: a small bypass for the LAD, plus a stent for other blockages. Early results are promising, especially for patients who want the durability of surgery with less trauma.
If you’ve been told you need revascularization, ask for a heart team evaluation. Don’t accept a quick decision. Request a copy of your angiogram and ask: "What’s my SYNTAX score?" If it’s above 22, CABG should be seriously considered. If you’re diabetic, it’s even more critical.
Ask your surgeon: "How many CABGs do you do a year?" Ask your cardiologist: "How many stents do you place?" Their answers tell you their experience level.
And remember: this isn’t about which procedure is "better." It’s about which one gives you the best chance to live well for the longest time-with the fewest repeat interventions.
PCI has lower immediate risks-it doesn’t require open-heart surgery, so stroke and infection rates are lower in the first 30 days. But over time, CABG reduces the risk of heart attacks and repeat procedures. For most patients, the long-term safety profile favors CABG, especially if you have diabetes or complex blockages.
Yes. Some patients get a stent first for an urgent blockage, then later undergo CABG if more arteries become blocked. Others get a hybrid approach: a small bypass for the most critical artery, and stents for others. This is becoming more common, especially in centers with advanced heart teams.
CABG requires a longer hospital stay, general anesthesia, surgical staff, and intensive care. Medicare pays about $35,000 for CABG versus $12,500 for PCI. But the cost difference isn’t just about the procedure-it’s about long-term outcomes. Fewer repeat surgeries and fewer heart attacks mean lower total costs over five years with CABG.
After PCI, you’ll typically take two blood thinners-like aspirin and clopidogrel-for at least one year to prevent stent clots. After CABG, you’ll usually take aspirin for life to keep grafts open. Some patients need additional meds depending on their risk factors. Never stop these without talking to your doctor.
Success depends on how you define it. For immediate symptom relief, both are about 90% effective. For long-term survival and avoiding repeat procedures, CABG wins in complex cases. Five-year survival is 10-12% higher with CABG for diabetic patients with multivessel disease. Repeat revascularization rates are nearly double with PCI in these groups.
Just had my second stent last year after a heart attack. First one was 5 years ago. The recovery was nothing compared to my cousin’s CABG-he was out of work for 3 months and still gets chest tightness when it’s cold. I’m back to hiking weekends. Stents aren’t perfect, but for a single blockage? Worth it.
Let’s be real-CABG is just Big Pharma’s way of keeping surgeons employed. You think they want you to get better? They want you to come back. Stents are cheaper, faster, and you don’t need to be cut open like a Thanksgiving turkey. Why do you think the hospitals push CABG? Profit.
I’m a nurse in cardiac ICU. Saw both procedures a hundred times. PCI is great for the right patient-quick, low risk. But when someone’s got three blocked arteries and diabetes? CABG isn’t just better, it’s life-saving. The stents keep failing, and then you’re back in the cath lab again. It’s exhausting for the patient. CABG gives you a real shot at 10+ years without another surgery.
If you’re reading this because you or someone you love is facing this decision-breathe. This isn’t a race. Talk to your heart team. Ask for your SYNTAX score. Don’t let a cardiologist push stents because they’re trained to do them. Don’t let a surgeon push CABG because it’s their specialty. You deserve both perspectives. And if you’re diabetic? Don’t wait. CABG is the move. You’ve got one heart. Treat it like it matters.
PCI success rates are inflated. Most studies exclude patients over 75 or with CKD. Real-world data shows 40% of stent patients need another procedure in 5 years. CABG grafts last longer. The data’s clear. Stop pretending they’re equal.
My uncle had CABG in India. Surgeon used his internal mammary artery. No vein grafts. 12 years later, he’s still walking 10 km every morning. No meds except aspirin. This isn’t just medicine-it’s a second life. Don’t underestimate the power of the right surgery.
Stents are a government conspiracy 😱 They put tracking chips in them so they can monitor your heart rate and sell your data to insurance companies. I read it on a blog. CABG is the only real way out. Also, the hospital food is poison. 🤫
my dr told me to get a stent but i asked for the sytax score and it was 38 so i went with cabg. 8 weeks later i can lift my grandkids again. no chest pain. no meds except aspirin. if you got multivessel disease dont play games. go cabg. your future self will thank you
Just a heads-up-CABG isn’t always better. I had a 72-year-old patient with emphysema and a single LAD blockage. CABG would’ve killed him. He got a stent, walked out the next day, and is still gardening. One size doesn’t fit all. Context matters.
Choice is an illusion. We’re all just data points in a system designed to keep us consuming.
Anyone who thinks PCI is a good long term solution hasn’t read the 2023 JAMA meta-analysis. The 10-year occlusion rate for drug eluting stents is 28% in diabetics. Arterial grafts are 15%. That’s not even close. Also if you’re getting a vein graft you’re already losing. Use the internal mammary. Always. And stop using the word "safe" for PCI. It’s not safe. It’s convenient.