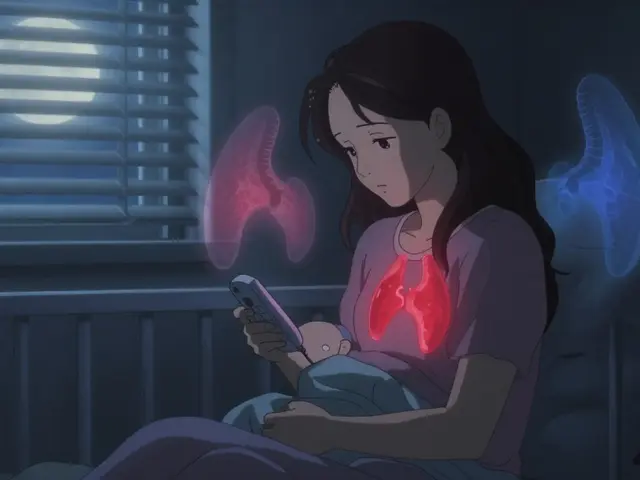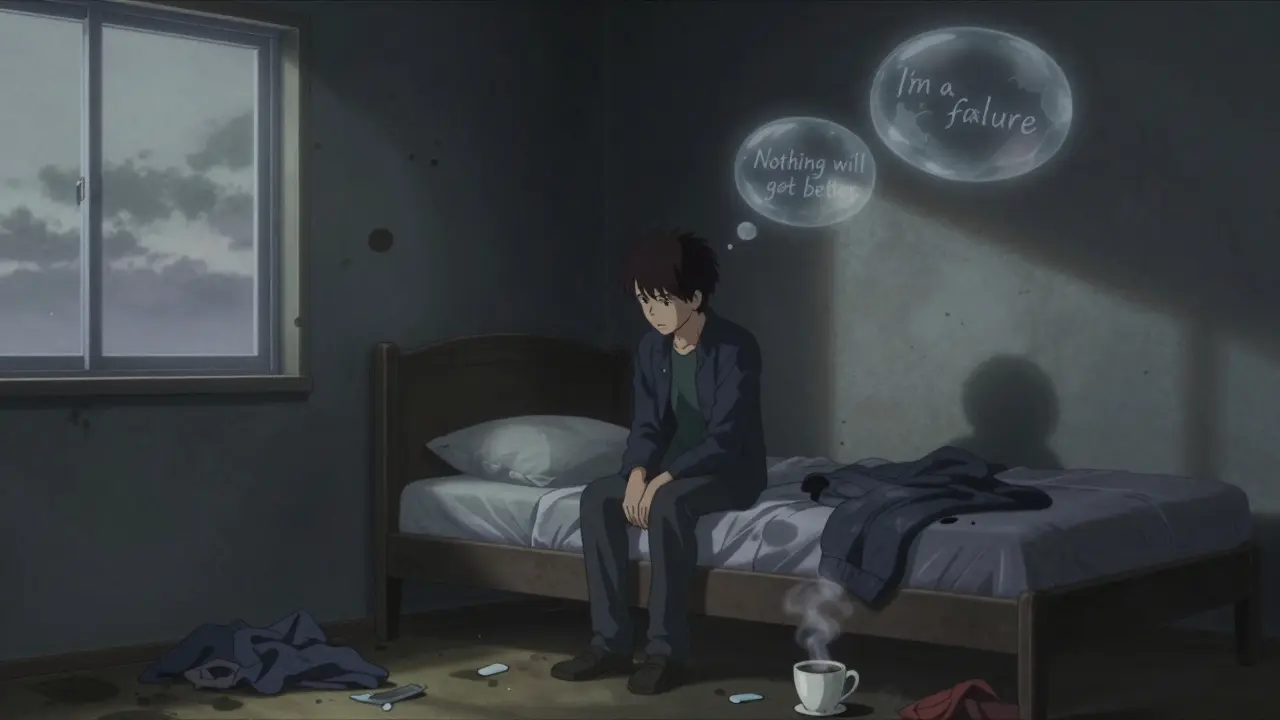
Depression isn’t just feeling sad. If you’ve lost interest in things you once loved, feel drained most days, or struggle to get out of bed even when you know you should, you might be dealing with major depressive disorder (MDD). It’s not a weakness. It’s a medical condition affecting about 1 in 6 adults in the U.S. every year, according to the National Alliance on Mental Illness. The good news? Treatment works. And you don’t have to choose between medication and therapy-you can use both.
Psychotherapy helps you understand why you feel the way you do. It gives you tools to change how you think, react, and cope. Medication helps balance the chemicals in your brain that affect mood. Neither is a quick fix. But both can lead to lasting improvement.
Most therapy sessions last 50 to 60 minutes and happen weekly. A full course usually takes 12 to 20 sessions. Some people feel better after just a few weeks. Others need longer. The key? Showing up consistently-even when you don’t feel like it.
The most commonly prescribed antidepressants today are second-generation drugs. They’re safer and have fewer side effects than older ones.
It takes time. Most people notice small improvements in energy or sleep after one or two weeks. But full relief usually takes 6 to 12 weeks. Many give up too soon. If you’re not feeling better after 8 weeks, talk to your doctor. It might mean adjusting the dose or switching meds.
Side effects are common at first-nausea, headaches, dry mouth, trouble sleeping, or reduced sex drive. These often fade after a few weeks. If they don’t, your doctor can help you switch to a different medication. Don’t stop taking antidepressants suddenly. That can cause withdrawal symptoms. Always taper off under medical supervision.

Why? Therapy teaches you skills that last. Medication helps you get to a point where you’re able to use those skills. If you’re too overwhelmed to even think clearly, medication can lift the fog enough for therapy to work. If you’re only on medication, you might feel better-but you haven’t learned how to handle future stressors. That’s why relapse rates are higher with medication alone.
The NHS and Cleveland Clinic both recommend combination therapy for moderate to severe depression. If your PHQ-9 score (a depression screening tool) is 16 or higher, this approach is strongly advised.
Online apps and chatbots might feel helpful, but they’re not a substitute for professional care. The Mayo Clinic warns that digital tools should be used as support-not replacement-for therapy or medication.
And while some believe antidepressants are overprescribed, the bigger issue is under-treatment. Many people suffer for years because they don’t know treatment exists-or they’re afraid of stigma. You’re not weak for needing help. You’re human.
Ask your GP for a referral. In the UK, you can often self-refer to NHS psychological therapies (IAPT) without seeing a specialist first. In the U.S., check with your insurance. Many employers now cover mental health services.

People on Reddit share real stories: one user said SSRIs made them feel emotionally numb-but functional. Another said CBT gave them tools they still use five years later. One person waited eight weeks for Prozac to work and felt worse before better. That’s common. Patience matters.
Therapy requires effort. You’ll get homework. You’ll be asked to track your thoughts. It can feel awkward at first. But the goal isn’t to “fix” you-it’s to help you understand yourself better.
Medication isn’t a magic pill. But for many, it’s the bridge back to life.
Electroconvulsive Therapy (ECT) is one of the most effective treatments for severe, treatment-resistant depression. It’s done under anesthesia. A small electric current triggers a brief seizure. It sounds intense, but it’s safe and often life-saving. Many patients report dramatic improvement after just a few sessions.
Other options include transcranial magnetic stimulation (TMS) and ketamine therapy. These are newer and usually offered through specialists.
Don’t give up. Keep talking to your doctor. There’s always another path.
Start with your GP. Ask about local therapy services. Research your medication options. Talk to someone you trust. And remember: asking for help isn’t surrender. It’s the first step back to living.
I've been on sertraline for 6 months and honestly? It didn't fix me, but it let me show up. Therapy did the rest.
The idea that antidepressants are 'just chemical crutches' is a dangerous myth pushed by anti-pharma ideologues. The brain is an organ. When it breaks, you fix it. End of story.
They want you on pills so they can control you. Big Pharma owns the FDA and your doctor. They don't want you cured. They want you addicted.
I must express my profound appreciation for the meticulous articulation of evidence-based therapeutic modalities, particularly the nuanced differentiation between CBT and ACT; such clarity is an absolute rarity in public discourse on mental health.
You say therapy helps you understand yourself. But what if you don't like what you find? What if you're just broken? And what if the therapist is just another overpaid person who's never had to work a real job?
If you're too tired to walk to the mailbox then you need to get up and move not sit there waiting for a pill to fix you
Did you know the WHO admits that antidepressants have no clinically significant advantage over placebo for mild depression? And yet they're prescribed to 1 in 5 Americans. Coincidence? Or a system designed to chemically sedate the population?
I tried CBT and honestly at first it felt like homework from a teacher who didn't get me but after like 8 weeks i started noticing i stopped yelling at my cat when she knocked over my coffee and that was kind of a win i guess
Funny how they list CCBT as a 'good option' but never mention that most of those apps are owned by the same pharma companies pushing the pills. You're not getting therapy-you're getting targeted ads with a side of cognitive restructuring.
The entire framework is a bourgeois construct-therapy as a commodified performance of self-awareness, medication as a neoliberal pacifier. We've reduced existential despair to a checklist of DSM-5 criteria and a subscription to BetterHelp. The real illness is the system that makes us believe we can heal alone in a world designed to break us.
I was prescribed Prozac after my dad died and the doctor didn't even ask about my childhood trauma. Just scribbled a script. Now I'm on five meds and I still cry in the shower. They don't care. They just want to keep the machine running
Ah yes, the classic 'just get out of bed' advice. Truly, nothing says 'I understand your suffering' like telling someone who can't lift their head to exercise. How very formal. How very cruel.