
When a dog develops a bacterial infection, the first question owners ask is "what will fix it fast?" The answer often lands on a trusted antibiotic: Cephalexin for Dogs. Below you’ll get a vet‑backed walkthrough of how this drug works, when it’s right, how to dose it safely, and what pitfalls to watch out for.
Cephalexin is a first‑generation cephalosporin antibiotic widely prescribed in veterinary medicine to combat a range of bacterial infections in dogs. It blocks the bacterial cell wall from forming, causing the microbes to burst and die. Because it targets a step that humans and dogs share, it’s considered safe when used at the correct dose.
Cephalexin belongs to the beta‑lactam class, which includes penicillins. In dogs, the drug binds to penicillin‑binding proteins, disrupting peptidoglycan cross‑linking. The result is a weakened wall that can’t hold up against osmotic pressure, leading to cell lysis. The action is bactericidal, meaning it kills bacteria rather than merely stopping their growth.
Veterinarians typically reach for Cephalexin when they suspect infections caused by gram‑positive organisms such as Staphylococcus aureus or mixed infections that also involve gram‑negative bacteria like Escherichia coli. Common scenarios include:
If the culture shows resistance to beta‑lactams, vets switch to alternatives like Amoxicillin or Clindamycin.
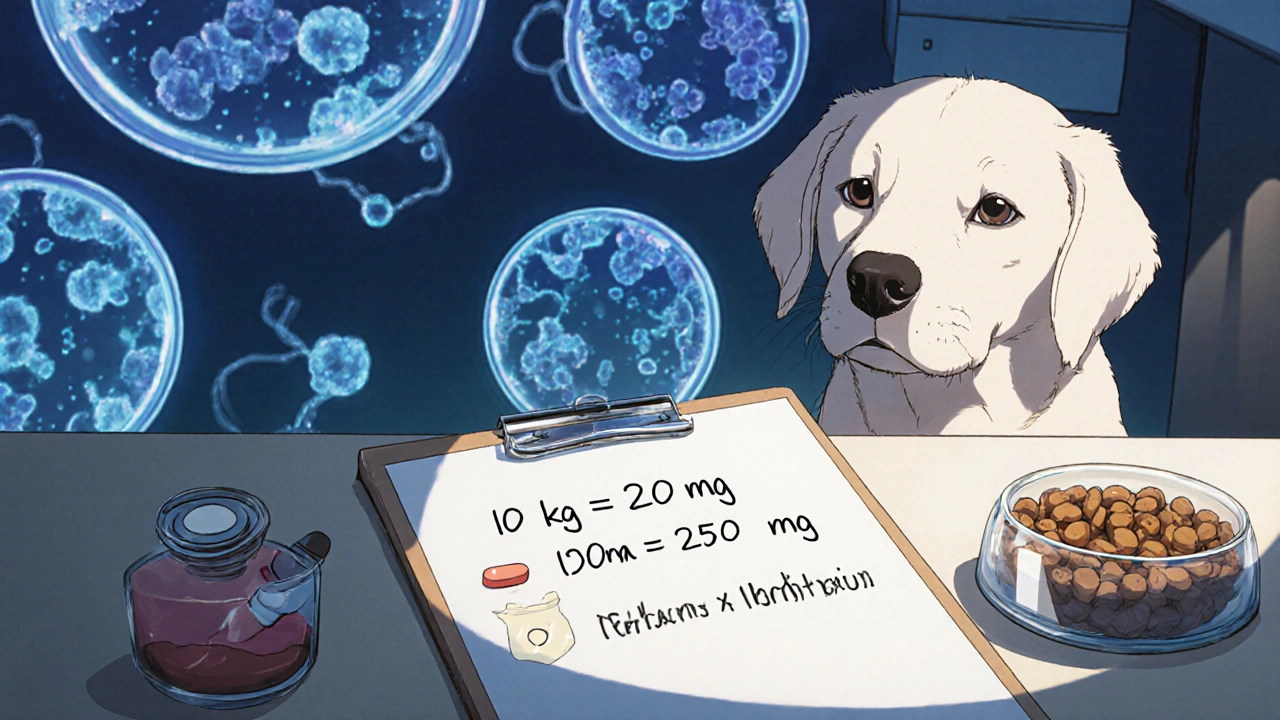
Accurate dosing is the single most important safety factor. The standard recommendation for healthy adult dogs is 15-30 mg per kilogram of body weight, given every 12 hours. Here’s a quick calculation example:
For puppies, senior dogs, or those with kidney dysfunction, the Veterinary Medicines Directorate recommends starting at the lower end (15 mg/kg) and monitoring bloodwork.
Most dogs tolerate Cephalexin well. When adverse reactions happen, they usually appear within the first few days:
If any of these occur, contact your vet. In rare cases, prolonged use can lead to antibiotic resistance, making future infections harder to treat.
Below is a side‑by‑side look at the three most frequently prescribed oral antibiotics for dogs.
| Attribute | Cephalexin | Amoxicillin | Clindamycin |
|---|---|---|---|
| Class | 1st‑gen cephalosporin | Penicillin derivative | Lincosamide |
| Spectrum | Gram‑positive + some gram‑negative | Broad gram‑positive, some gram‑negative | Strong gram‑positive, anaerobes |
| Typical Dose | 15‑30 mg/kg q12h | 10‑20 mg/kg q12h | 5‑10 mg/kg q12h |
| Common Uses | Skin, urinary, bone infections | Respiratory, dental, soft‑tissue | Abscesses, anaerobic infections |
| Side‑Effect Profile | Mild GI upset | GI upset, occasional rash | Higher risk of diarrhea, C. difficile |
Choosing the right drug hinges on culture results, infection location, and the dog’s health status. Cephalexin remains a first‑line choice for many skin and urinary cases because of its balance of efficacy and safety.

Resistance isn’t just a hospital problem - it’s a real concern in everyday pet care. Here are three vet‑approved habits to keep bacteria in check:
Following these steps helps preserve the effectiveness of Cephalexin and other antibiotics for future patients.
Only under veterinary guidance. Human formulations may contain inactive ingredients that irritate a dog’s stomach, and the strength could differ from the veterinary product.
Most dogs show improvement within 48-72 hours. Full resolution often requires 7‑14 days, depending on infection severity.
Studies suggest it’s low risk, but vets usually choose the minimal effective dose and monitor the dam closely.
Give a small amount of food and re‑dose after 30 minutes if the vomiting stops. If it recurs, call the vet - the dosage may need adjusting.
No. Cephalexin targets bacteria only. Fungal infections require antifungal agents like itraconazole or fluconazole.
Armed with this vet‑tested overview, you can discuss the plan confidently with your animal doctor and keep your canine companion on the fast track to recovery.
American vets love to push cephalosporins like Cephalexin while ignoring cheaper alternatives that work just as well. Many assume safety without questioning necessity.
It’s reassuring to see a thorough breakdown of dosing; many owners feel lost when the vet mentions milligrams per kilogram.
Understanding the mechanism helps owners appreciate why completing the full course is essential, especially when bacterial resistance is a global concern.
Cephalexin works well for skin infections and UTIs
I always double‑check the tablet strength before giving it to my pup.
Cephalexin is marketed as a harmless first‑line drug, but its overuse fuels resistance.
Vets prescribe it without culture results far too often, assuming safety.
This cavalier attitude ignores the evolutionary pressure it places on microbes.
Every unnecessary dose selects for beta‑lactamase producing strains.
When those strains spread, we lose a critical tool against gram‑positive infections.
Owners are routinely told “just finish the course,” yet the underlying problem is misprescription.
The dosage range of 15‑30 mg/kg is wide, leading some clinicians to err on the high side for convenience.
High doses increase gastrointestinal upset, prompting owners to stop early, which paradoxically promotes resistance.
In my experience, culture‑guided therapy reduces treatment failures by over 30 %.
Moreover, many formulations contain fillers that irritate a dog’s stomach, a fact rarely disclosed.
The cheap human tablets may have different excipients, making them unsuitable for canines.
Renal‑compromised dogs require dose reductions, yet this nuance is often omitted in busy practices.
Ethical prescribing demands a risk‑benefit analysis before reaching for any antibiotic.
Veterinarians should default to narrow‑spectrum agents unless broader coverage is justified.
Ultimately, responsible use of Cephalexin preserves its efficacy for the dogs that truly need it.
Glad you found the dosing guide useful; it’s also a good idea to ask the vet about weight‑based syringes for more precise dosing.
While your alarmist tone is noted, the reality is that American veterinary schools already emphasize antimicrobial stewardship, so painting the whole system as negligent is unfair.
The claim that stewardship curricula are uniformly robust overlooks the variability among institutions, many of which still lack mandatory culture‑first protocols.
Indeed, precise dosing is crucial, and, as you suggested, employing calibrated syringes not only improves accuracy, but also reduces the risk of under‑dosing, which, in turn, mitigates the development of resistant bacterial populations.
I appreciate the focus on resistance; it’s something I keep in mind when my own dog shows signs of infection.
Statistically, the absence of mandatory susceptibility testing correlates with a 12 % increase in treatment failures across surveyed clinics; this metric underscores the necessity for evidence‑based prescribing 😐.
Yo, that data is kinda whack, man-if u don’t run a culture u’re just guessin’ and wasting meds, lol.
Remember, a calm approach and consistent follow‑up labs can turn a scary infection into a manageable situation; you’ve got this.
It’s not a coincidence that the pharmaceutical push for Cephalexin aligns with hidden agendas to keep pet owners dependent on costly veterinary visits, a narrative conveniently ignored by mainstream discourse.