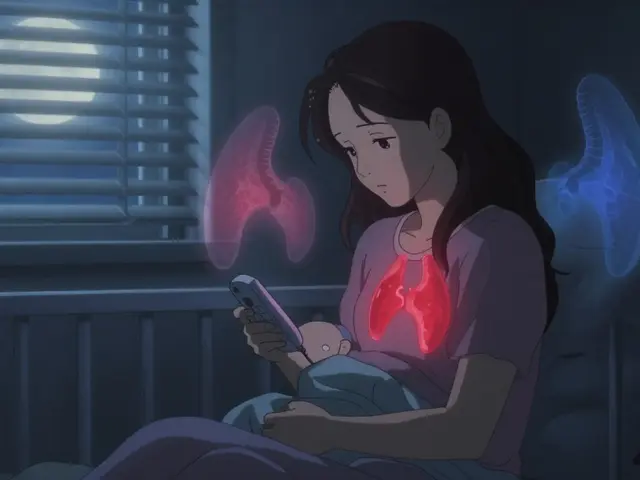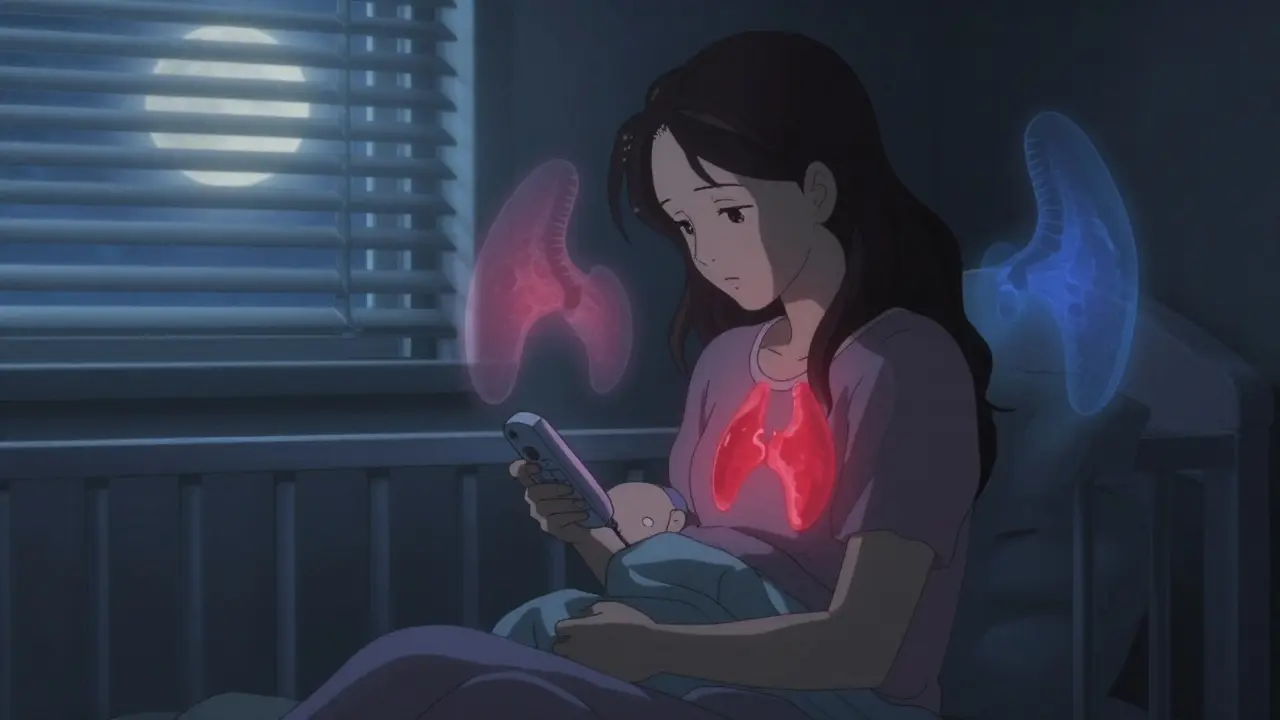
After having a baby, many women feel exhausted, emotional, and overwhelmed. It’s normal. But what if your fatigue isn’t just from sleepless nights? What if your hair is falling out, you’re gaining weight despite eating less, and you’re freezing cold when everyone else is sweating? These aren’t just signs of being a new mom-they could be symptoms of postpartum thyroiditis, a hidden thyroid problem that affects 5 to 10% of women after childbirth.
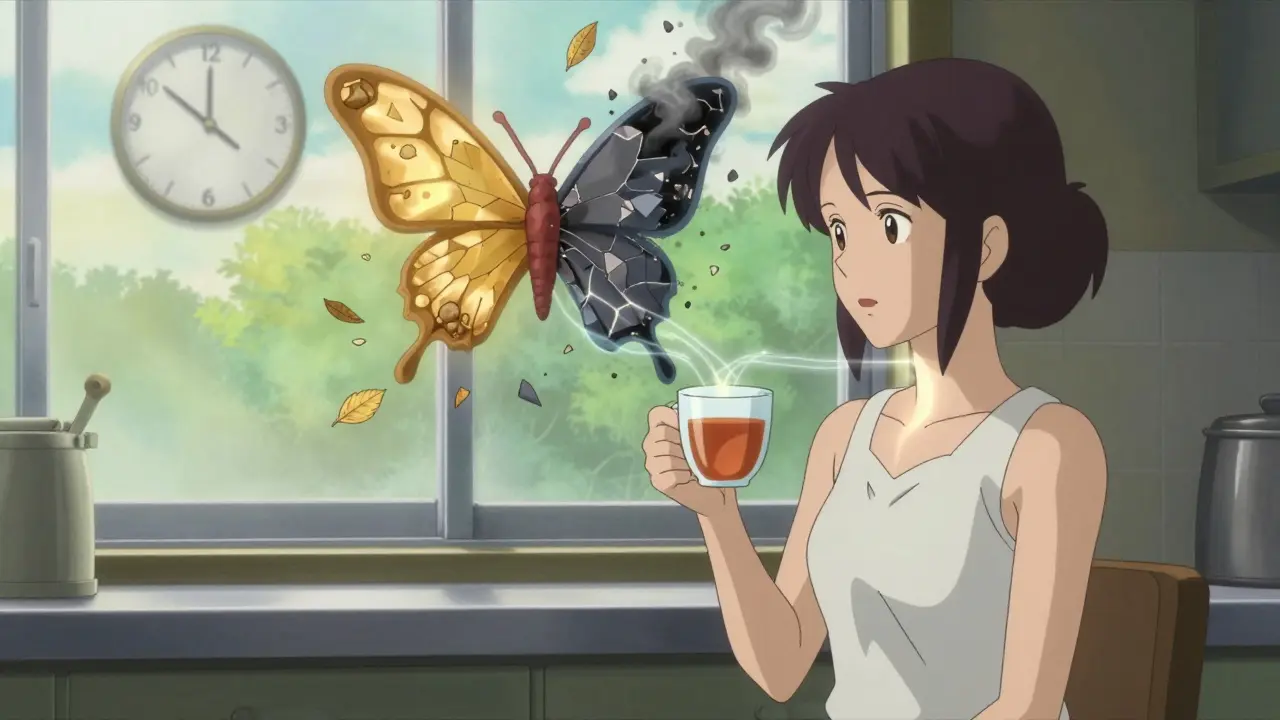
Postpartum thyroiditis is an autoimmune condition where the body’s immune system mistakenly attacks the thyroid gland after pregnancy. It’s not caused by infection or poor diet-it’s your immune system going into overdrive after being suppressed during pregnancy. The thyroid, a small butterfly-shaped gland in your neck, controls your metabolism, energy, mood, and body temperature. When it gets damaged, your hormone levels swing wildly.
This isn’t a permanent condition for most women. About 70 to 80% recover normal thyroid function within a year. But for 20 to 30%, it becomes lifelong hypothyroidism, requiring daily medication. The big problem? Most women don’t realize what’s happening. Doctors often mistake it for postpartum depression or just “being tired.”
Postpartum thyroiditis doesn’t hit you all at once. It comes in two phases-sometimes one, sometimes both-and they’re totally different.
Phase 1: Hyperthyroidism (1 to 4 months after birth)
Your thyroid gets inflamed and leaks stored hormones into your bloodstream. You don’t make more hormones-you just release what’s already there. This causes temporary hyperthyroidism. Symptoms include:
Here’s the catch: up to half of women feel almost nothing during this phase. If you do notice symptoms, you might think it’s just anxiety or caffeine overload. That’s why this phase often goes undiagnosed.
Phase 2: Hypothyroidism (4 to 8 months after birth)
After the thyroid runs out of stored hormones, it can’t make new ones fast enough. Now you’re hypothyroid. Symptoms are the opposite:
Eighty-nine percent of women with this condition report crushing fatigue. It’s not normal tiredness. It’s the kind that makes it hard to lift your baby, drive, or even shower. And it lasts months-not days.
Some women skip the hyperthyroid phase entirely and go straight to hypothyroidism. Others have only mild symptoms. But if you’re in the 20 to 30% who don’t recover, you’ll need lifelong thyroid hormone replacement.
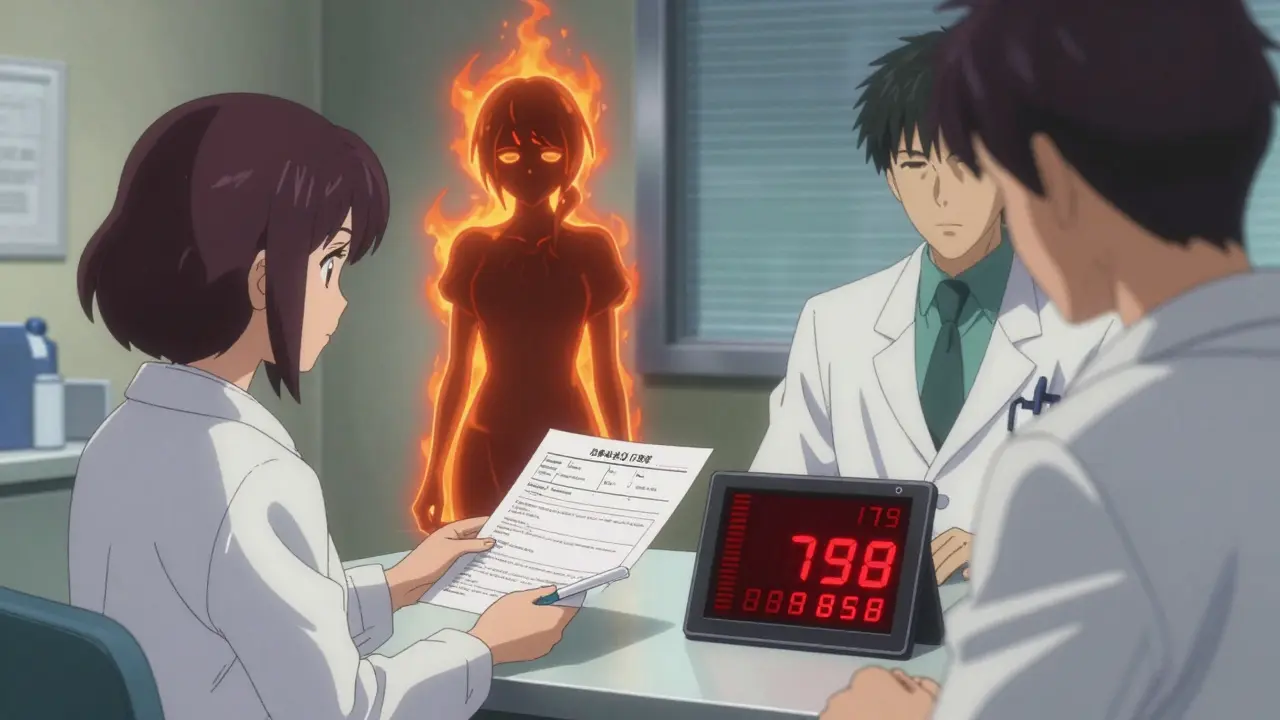
You can’t guess this. You need blood tests.
During the hyperthyroid phase, your TSH (thyroid-stimulating hormone) will be low-below 0.4 mIU/L-and your free T4 (thyroid hormone) will be high. In the hypothyroid phase, TSH spikes above 4.5 mIU/L and free T4 drops. But the real key? Testing for thyroid peroxidase antibodies (TPOAb). If they’re positive, you have autoimmune thyroiditis.
Over 80% of women with postpartum thyroiditis test positive for TPO antibodies. If you had them before pregnancy, your risk jumps to 70%. That’s why women with type 1 diabetes, a history of thyroid issues, or a family history of autoimmune disease should get tested at 10 weeks postpartum-even if they feel fine.
Here’s the problem: only 42% of OB/GYNs routinely check thyroid function in women with lingering postpartum symptoms. Most wait until the woman complains-often months later.
Postpartum thyroiditis looks a lot like other problems. Here’s how to tell them apart:
One study found that 30% of women diagnosed with postpartum depression actually had undiagnosed thyroiditis. Many were put on antidepressants for months before their thyroid levels were checked.
Not everyone gets this. But certain women are far more likely to:
If you fall into any of these groups, get tested at 6 to 12 weeks after delivery. Don’t wait for symptoms.
You don’t always need medication.
During the hyperthyroid phase: Most women don’t need treatment. If your heart is racing badly or you’re anxious, a beta-blocker like propranolol can help control symptoms. But you don’t need drugs to lower thyroid hormones-you’re not making extra. Your body will reset itself.
During the hypothyroid phase: If your TSH is above 10 mIU/L, or if you have symptoms, you’ll likely need levothyroxine (Synthroid or generic). This is safe during breastfeeding and usually temporary. Most women stop it after 12 months. But if your TSH stays high after a year, you probably have permanent hypothyroidism and will need it for life.
Don’t try to treat this with supplements, herbs, or diets. Thyroid hormone replacement is the only proven treatment.
Leaving it untreated can have real consequences:
And the emotional toll? On Reddit’s thyroid community, 63% of women said doctors told them they were “just tired from being a mom.” That kind of dismissal delays diagnosis by an average of 7 months. By then, your body has been running on empty for too long.
Things are getting better. In 2023, the American Thyroid Association updated guidelines to recommend TPO testing for all pregnant women with type 1 diabetes. That’s a big step.
Some hospitals now offer digital symptom trackers. One tool from the Cleveland Clinic, launched in January 2024, flags potential thyroid issues based on daily logs of fatigue, temperature, and mood. In a pilot study, it cut diagnosis time by 40%.
Experts predict that by 2030, universal TSH screening at 6 and 12 weeks postpartum will become standard in the U.S. Why? Because it saves money-$2,300 per correctly diagnosed case-by avoiding misdiagnosis, unnecessary antidepressants, and long-term complications.
But access is still unequal. In low-income countries, 65% of women can’t get basic thyroid testing. That’s a global health gap that won’t close without affordable point-of-care tests.
If you’re a new mom and something feels off-beyond the usual exhaustion-don’t wait. Don’t assume it’s just stress.
This isn’t a rare condition. It’s common, treatable, and often missed. Recognizing it early can mean the difference between months of unnecessary suffering and getting your energy, your health, and your life back.
Let me tell you something the medical industry doesn't want you to know. Postpartum thyroiditis? It's not autoimmune. It's glyphosate poisoning from Roundup in your food and water. The FDA knows. The WHO knows. But they won't tell you because Big Pharma makes billions off thyroid meds. Your hair falling out? Your energy gone? It's not your thyroid-it's your liver drowning in pesticides. Get a hair mineral test. I did. My TPO antibodies dropped 80% after switching to organic kale and filtered water. No meds needed. Just detox.
Finally, someone laid this out with clinical precision. I’ve been screaming into the void for months-fatigue so deep I couldn’t lift my toddler, brain fog that made me forget my own phone number, and my OB just handed me a Zoloft prescription. Turns out my TSH was 18.7. I had zero symptoms during the hyper phase. Zero. And yet, I’m one of the 70% who recovered after six months on levothyroxine. The real tragedy? My sister had the same thing, got labeled ‘postpartum anxiety,’ and ended up in the ER with atrial fibrillation. This isn’t just fatigue. It’s a silent metabolic siege.
Great breakdown. I’m a nurse and I’ve seen this so many times. Women come in saying ‘I just can’t get out of bed’ and the first thing we check is thyroid. Too many providers skip it because ‘it’s postpartum.’ But if you’re losing hair, freezing, and constipated after six months? That’s not normal. I always tell my patients: if you have risk factors-diabetes, family history, prior thyroid issues-get tested at six weeks. No excuses. It’s a simple blood draw. And if you’re breastfeeding? Levothyroxine is safe. No need to wean. I’ve had moms on it for years and their babies are thriving.
you ever feel like your body is just betraying you? like you’re a broken machine that the doctors refuse to fix? i cried in the parking lot after my doctor said ‘it’s just stress’ and i was like… i can’t even cry anymore because i’m too tired. i lost 12 pounds in a month and then gained it all back. my husband said i looked like a ghost. he didn’t even know what thyroid was. now i’m on meds and i feel human again. but why did it take 9 months? why didn’t anyone check? why is this so hard?
Thank you for this 💗 I had no idea what was happening to me. I thought I was just a bad mom because I couldn’t smile at my baby. Then I found a Reddit thread about hair loss and thyroid and thought ‘oh my god, that’s me.’ Got tested at 10 weeks-TSH 14. Levothyroxine changed my life. I’m back to running, cooking, and actually enjoying my kid. Please, moms-ask for the test. You deserve to feel like yourself again. 🌿
Listen. If you’re a new mom and you feel like you’re running on fumes while everyone else is zooming-don’t ignore it. Don’t let anyone tell you it’s ‘just hormones.’ You’re not lazy. You’re not broken. You’re not ‘overreacting.’ This is real. This is common. This is treatable. I was diagnosed at 8 months postpartum after my pediatrician noticed I was shaking and asked if I’d been tested. I hadn’t. I’m now 14 months off meds and feeling like me again. Advocate for yourself. Print this article. Bring it to your doctor. Your life is worth more than a 10-minute appointment.
so i read this whole thing and i’m still confused. like… if it’s temporary then why are we all acting like it’s the end of the world? my cousin had this and she just drank coffee and slept with the baby. now she’s fine. also why is everyone so obsessed with blood tests? i mean, i got a fever last week and i didn’t go to the doctor. i just took tylenol. why is thyroid different? also i think they’re just selling more meds. also my dog has thyroid issues and he just eats chicken. maybe we should all just eat chicken.
postpartum thyroiditis? nah. it’s all the vaccines. they put nanoparticles in the shots that latch onto your thyroid and make it go haywire. i know because my cousin’s neighbor’s cousin got it after the flu shot and then her daughter got autism. the CDC won’t admit it because they’re paid by Big Pharma. also the 5-10% stat? that’s a lie. it’s more like 40%. they only count the ones who survive the ‘medical neglect.’ i’m not even gonna get into the 5G towers. but trust me. your thyroid is being targeted. get a kelp supplement. and a Faraday cage for your bedroom.
why are you all so serious about this. i had baby and i was tired. that’s it. no tests no meds. i just drank tea and slept when baby slept. now i’m fine. you people need to chill. this is not a crisis. it’s just life. stop making everything a medical emergency. also i don’t believe in blood tests. they are expensive and useless. my uncle in india had thyroid and he just ate mangoes. it worked. so why not just eat mangoes?
bro i had this. i thought i was just bad at being a mom. turned out my tsh was through the roof. i didn’t even know what tsh was. i thought it was a brand of yogurt. got tested after my partner said ‘you’re not sleeping, you’re not eating, you’re just staring at the wall.’ i cried in the car after the results. then i got meds. now i can hold my kid without crying. it’s not magic. it’s science. ask for the test. it’s one needle. you’ve survived childbirth. this is nothing.
the data here is statistically significant but lacks longitudinal follow-up. 70-80% recovery is based on small cohort studies with selection bias. most women who recover are younger, healthier, and have better access to care. the 20-30% who don’t? they’re often low income, nonwhite, or undocumented. the article ignores systemic healthcare disparities. also, levothyroxine isn’t ‘safe’-it’s a synthetic hormone with potential long-term cardiovascular effects. why not explore functional medicine approaches? diet, stress reduction, gut microbiome? no one mentions that. this is a surface-level analysis with a pharmaceutical slant.
I found this so helpful. In the UK, we don’t routinely test unless symptoms are severe. I only got tested because I’d had thyroid issues before. My GP said, ‘It’s probably just exhaustion.’ I had to insist. I’m glad I did. I’m now 10 months postpartum and off medication. I think awareness needs to be better here too. Maybe we need a campaign-‘Check Your Thyroid After Baby’-like they do for gestational diabetes. Simple. Free. Life-changing.
Oh please. Another ‘mommy blog’ medical article. This is so reductive. You treat a complex endocrine disorder like it’s a glitch in a smartphone. ‘Just take Synthroid.’ No one talks about the adrenal fatigue, the cortisol dysregulation, the gut-thyroid axis. And you call it ‘temporary’? What about the women who develop Graves’ or Hashimoto’s later? You’re just giving them a Band-Aid and calling it a cure. Also, the ‘universal screening by 2030’ fantasy? That’s corporate wellness propaganda. They want you dependent on lifelong meds. Wake up. Your body isn’t broken. The system is.