If you’re on a blood thinner, you’re not just taking a pill. You’re managing a delicate balance between preventing deadly clots and avoiding life-threatening bleeding. For decades, warfarin was the only game in town. Today, direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban have taken over - and for good reason. But that doesn’t mean warfarin is obsolete. In fact, for some people, it’s still the safest choice.
The big shift happened because DOACs don’t need constant blood tests. No more weekly INR checks. No more worrying if your spinach salad will throw off your dose. But DOACs come with their own risks - especially if you have kidney problems or can’t afford them. Warfarin is cheap, but it’s a minefield of interactions and strict routines. So which one is right for you? Let’s break it down, real talk, no fluff.
Warfarin has been around since 1954. It works by blocking vitamin K, which your body needs to make clotting factors. Simple, right? Not quite. The problem is, warfarin’s effect is wildly unpredictable from person to person. One person might need 5 mg a day. Another might need 10 mg. And that dose can change based on what you eat, what other meds you take, or even how much you drink.
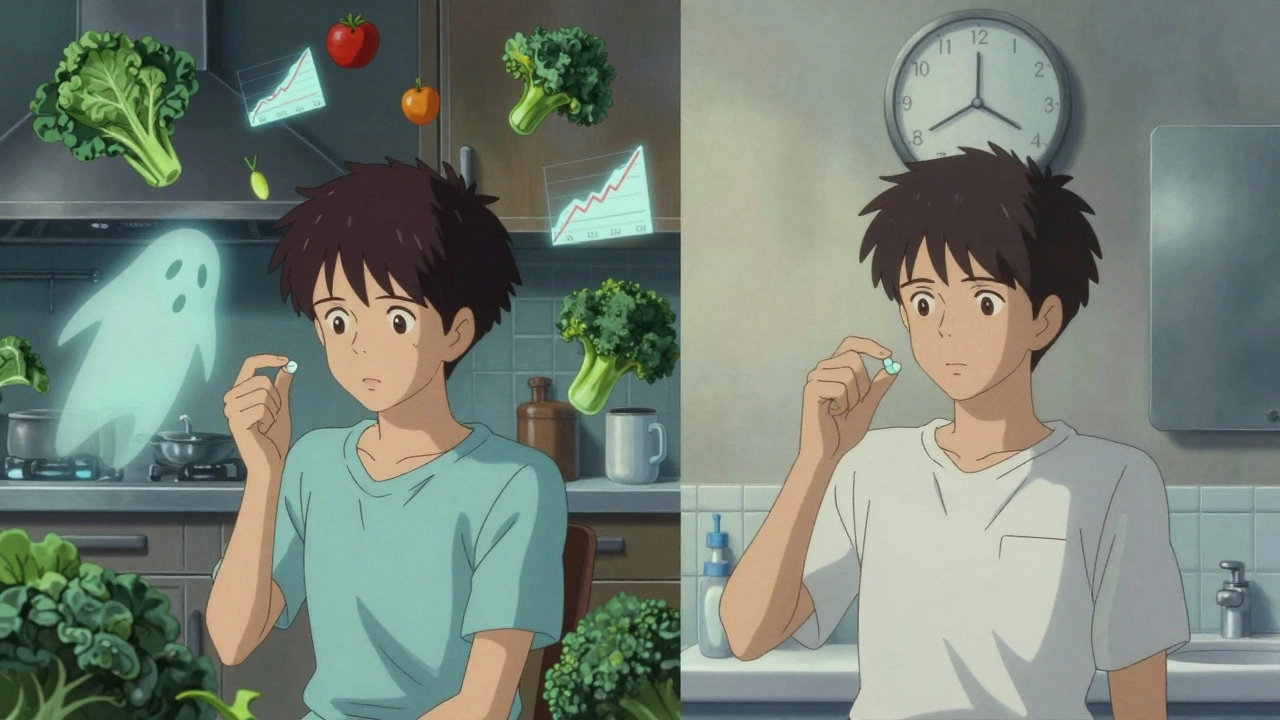
There are over 300 known drug interactions with warfarin. Antibiotics, painkillers, even some herbal supplements like St. John’s wort can send your INR skyrocketing or crashing. Vitamin K-rich foods - kale, broccoli, Brussels sprouts - can make warfarin less effective. So if you suddenly start eating more greens, you could be at risk for a clot. Eat less? You might bleed.
Monitoring is brutal. In the first month, you’ll likely get 6 to 12 blood tests. After that, it’s still 2 to 4 times a month. And even then, you need to stay in the therapeutic range - an INR between 2.0 and 3.0 - at least 70% of the time. Studies show nearly a third of warfarin users miss this target. That’s not just inconvenient. It’s dangerous.
DOACs changed everything. They don’t rely on vitamin K. They target specific clotting factors directly: dabigatran blocks thrombin (Factor IIa), while apixaban, rivaroxaban, and edoxaban block Factor Xa. That means they’re more predictable. Dosing is fixed. No routine blood tests. No dietary restrictions.
That’s why, as of 2023, DOACs made up 78% of all anticoagulant prescriptions in the U.S. Apixaban (Eliquis) alone accounts for nearly 40% of the market. And it’s not just popularity - it’s proof. Multiple studies, including one in JAMA Network Open (2023), show DOACs reduce the risk of stroke and major bleeding compared to warfarin. For people with atrial fibrillation, DOACs lower the risk of intracranial hemorrhage by about 50%. That’s huge.
Adherence is better too. People on DOACs are 32% more likely to take their medication consistently than those on warfarin. Why? Because it’s easier. No appointments. No dietary stress. Just pop the pill and forget it. For younger adults, especially those under 45, that difference in adherence is even bigger - up to 41%.
DOACs are safer for most people - but not everyone. If you have a mechanical heart valve, DOACs are dangerous. Period. Warfarin is the only option proven to work here. The same goes for severe mitral stenosis. In these cases, DOACs can lead to valve clots, strokes, or death.
Kidney function matters too. DOACs are cleared differently. Dabigatran is 80% removed by the kidneys. Apixaban? Only 27%. That means if your eGFR drops below 30 mL/min, some DOACs become risky. For patients with end-stage kidney disease on dialysis, warfarin is still preferred. The data on DOACs in this group is limited, and bleeding risk can spike.
And here’s something few patients realize: DOACs have no universal reversal agent. Yes, there’s idarucizumab for dabigatran and andexanet alfa for apixaban and rivaroxaban - but they’re expensive, not always available, and don’t work for all DOACs. Warfarin can be reversed quickly with vitamin K and fresh frozen plasma. In an emergency, that’s a big advantage.

Let’s be honest. DOACs are expensive. A 30-day supply of apixaban costs around $587. Rivaroxaban? $523. Dabigatran? Nearly $490. Warfarin? $4.27.
That’s not a typo. Warfarin is over 100 times cheaper. Insurance helps - but not always. Some plans still require step therapy: you have to try warfarin first, even if you’re a perfect candidate for a DOAC. And if you’re on Medicare or Medicaid, coverage gaps can leave you paying hundreds out of pocket.
For many, the cost isn’t just a hassle - it’s a dealbreaker. Some patients skip doses or stop entirely because they can’t afford it. That’s when the real danger kicks in. A missed dose of a DOAC? Risk of clot. A missed dose of warfarin? Maybe your INR drops. But if you’re not monitoring it, you won’t know.
Here’s the bottom line:
For cancer patients with AF, apixaban has the best bleeding profile. For those with recurrent clots, DOACs cut the risk of another one by 34% compared to warfarin. And if you’re over 75, DOACs reduce your risk of brain bleeding - the most deadly kind - by half.
DOACs have a short half-life. Apixaban lasts about 12 hours. Rivaroxaban, 7-11 hours. If you miss a dose, take it as soon as you remember - unless it’s almost time for the next one. Don’t double up. Missing doses increases clot risk fast.
Warfarin’s effects linger. If you miss a dose, your INR might drop slowly. But if you stop cold turkey, your risk of stroke spikes within days. That’s why the guidelines say a gap of 30 days or less is still considered “continuous” for warfarin. For DOACs? Only 14 days.
That’s why adherence matters more with DOACs. One missed day might not matter. Two? You’re flirting with danger.

If you bleed badly - say, from a fall or head injury - doctors need to reverse the anticoagulant fast. With warfarin, they give vitamin K and plasma. It works, but it takes hours.
For DOACs, there are specific antidotes: idarucizumab for dabigatran, andexanet alfa for apixaban and rivaroxaban. These work in minutes. But they’re not in every hospital. And they cost thousands. Edoxaban doesn’t even have an approved reversal agent in the U.S. That’s a real concern if you live in a rural area or travel often.
Research is moving fast. A new drug called Librexia™ - a combo of warfarin and vitamin K - is in phase 3 trials. The idea? Smoother INR control without daily testing. If it works, it could bring back warfarin for some.
The AUGUSTUS-CKD trial is watching how apixaban compares to warfarin in patients with advanced kidney disease. Results are due late 2024. That could change guidelines again.
For now, the trend is clear: DOACs are the future. But warfarin still has its place - especially when cost, kidney function, or mechanical valves are in play.
There’s no “best” anticoagulant. Only the best one for you.
If you’re young, active, and have AF - DOACs are likely your safest, easiest option. If you’re older, on dialysis, or have a mechanical valve - warfarin is still your best bet. If cost is a problem, talk to your doctor about patient assistance programs. Many manufacturers offer them.
Don’t let fear of blood tests or cost keep you from the right treatment. But don’t assume the newer drug is always better. Safety isn’t just about data. It’s about your life, your body, and your ability to stick with the plan.
Ask your doctor: “Based on my kidneys, my heart, my lifestyle, and my budget - which one is truly safest for me?” That’s the question that matters.
Yes, for most people. DOACs reduce the risk of stroke and major bleeding - especially brain bleeds - by 30-50% compared to warfarin. They also don’t require frequent blood tests or dietary changes. But they’re not safer for everyone. People with mechanical heart valves or severe kidney disease still need warfarin.
You can - if you don’t have a mechanical heart valve or severe kidney disease. Your doctor will check your kidney function (eGFR), review your medications, and make sure you’re not at high risk for bleeding. Switching usually happens after your INR is stable and within range. It’s a common move, especially for patients under 75.
If you miss a dose, take it as soon as you remember - unless it’s almost time for your next one. Don’t double up. Missing one dose is usually okay. Missing two or more increases your risk of clotting. DOACs wear off fast - within 12-24 hours - so consistency matters more than with warfarin.
Because DOACs aren’t safe for everyone. Warfarin is the only option for people with mechanical heart valves or severe mitral stenosis. It’s also the only choice for dialysis patients with limited DOAC data. Plus, warfarin can be reversed quickly with vitamin K, and it’s 100 times cheaper. For some, it’s still the most practical and proven option.
Your doctor checks your eGFR - a measure of kidney function - before prescribing any anticoagulant. DOACs like dabigatran and edoxaban are cleared mostly by the kidneys and may need dose adjustments if your eGFR is below 50. Apixaban is safest in mild-to-moderate kidney disease. If your eGFR is below 15, warfarin is usually preferred. Never start or switch without this test.
I've been on apixaban for 3 years now and honestly? Life changed. No more weekly blood draws, no more worrying if my kale smoothie killed my INR. I travel for work all the time and this thing just works. My doctor said I'm a textbook candidate for DOACs and I'm glad I switched.
Still, I get why some folks stick with warfarin - if you're on a tight budget or have a mechanical valve, it's the only real option. Just wish insurance didn't make us jump through hoops to get the better drug.
This is such a nuanced topic and I appreciate the breakdown because most people don't realize how much individual variation matters here. I'm from India and we have a lot of patients with CKD stage 3 or 4 who are on anticoagulants for AFib, and honestly, the cost differential between warfarin and DOACs is astronomical here - warfarin is like 20 rupees a month while apixaban runs you 4,000 rupees. Even with subsidies, many just stop taking it. But then again, I've seen patients with poor INR control on warfarin end up in the ER with intracranial bleeds, and it's heartbreaking. The real issue isn't the drugs themselves - it's access, education, and systemic gaps in monitoring. We need better infrastructure to support DOACs in low-resource settings, not just assume warfarin is the default because it's cheap. Also, kidney function testing is still not routine in many rural clinics, which is terrifying when you think about it. Maybe telehealth labs or point-of-care eGFR devices could help? I've been pushing for that in my hospital network.
Ugh why do people act like DOACs are magic? You think you're so smart taking them but you're just lazy and don't wanna test your blood. And then you miss a dose and boom stroke. Warfarin keeps you accountable. Also who even eats kale anymore? That's like 2015 nutrition advice. And don't even get me started on the price - if you can't afford 5 bucks a month you shouldn't be on blood thinners period. People are just too soft now.
I'm a nurse in a rural ER and I see the fallout from both sides. DOACs are amazing when patients take them - but when they miss doses? We get strokes in 40-year-olds. Warfarin? We see bleeds from INR spikes after antibiotics or dietary changes. The real hero here is patient education. If you're on DOACs, set phone alarms. If you're on warfarin, keep a food log. And please, for the love of god, tell your provider about every supplement you take - even that 'natural' turmeric pill. 🙏
The fact that we're even having this conversation shows how far we've drifted from real medicine. In my father's day, you took what your doctor prescribed and you didn't complain. Now everyone wants the 'best' drug based on some fancy study while ignoring cost, access, and discipline. DOACs are overpriced corporate toys. Warfarin has been saving lives since the Korean War. If you can't handle a weekly blood test, maybe you're not ready for the responsibility of anticoagulation. This country is falling apart because people think medicine is a menu.
I switched from warfarin to apixaban last year after my INR kept swinging wildly despite perfect adherence. My doctor said my genetics probably made me a poor warfarin responder. Honestly? I didn't even know that was a thing until I read this post. Now I take my pill every night at 8pm and never think about it. No more freezing up before a blood test. No more 'did I eat spinach today?' anxiety. I'm not saying DOACs are perfect but for someone like me? They're a godsend
Let's talk about the elephant in the room - the reversal agents. Andexanet alfa costs $10,000 a vial. Idarucizumab? $3,500. Most community hospitals don't stock them. So when a 78-year-old falls and hits their head on a DOAC? They get FFP and vitamin K anyway - the same old stuff. That means the 'safety advantage' of DOACs? It's mostly theoretical unless you're in a Level 1 trauma center. Meanwhile, warfarin reversal is cheap, reliable, and available everywhere. The marketing makes DOACs look like superheroes. Reality? They're just more expensive gamble.
I'm on rivaroxaban and I have to say - I used to hate the idea of blood thinners. But now I feel like I'm finally in control. I travel to Canada twice a year and I don't have to worry about finding a lab over there. I just pack my pills. My wife says I'm obsessed but I'd rather be obsessed than in the hospital. Also - anyone else notice that the DOAC commercials never mention the cost? They just show happy people hiking and laughing. Meanwhile, my insurance denied my first prescription and I had to call the manufacturer's patient assistance program. Took 3 weeks. But it was worth it.
You know... it's not about warfarin or DOACs... it's about the soul of modern medicine... we've lost our way... we chase convenience over commitment... we trade discipline for dopamine... and now we're surprised when people bleed out because they forgot their pill... the real tragedy isn't the drug... it's that we've forgotten how to be responsible... how to be patient... how to be human... I mean... if you can't remember to take a pill once a day... maybe you shouldn't be on a blood thinner at all... it's not the medication... it's the mindset... and the system that rewards laziness... and sells hope in a pill bottle... and calls it progress... sigh...
