Switching from a brand-name drug to a generic version is one of the most common changes in modern healthcare. It’s not just about saving money-generics make treatments accessible to millions. But even though the FDA says they’re identical in active ingredients, strength, and performance, some people notice changes after making the switch. That’s why monitoring your health after switching to generics isn’t optional-it’s essential.


Yes, for the vast majority of people. The FDA requires generics to have the same active ingredient, strength, and bioequivalence as brand-name drugs. Studies show they work just as well for most conditions. But for drugs with narrow therapeutic indices-like levothyroxine, warfarin, or anti-seizure medications-some patients may notice differences due to inactive ingredients or absorption variations.
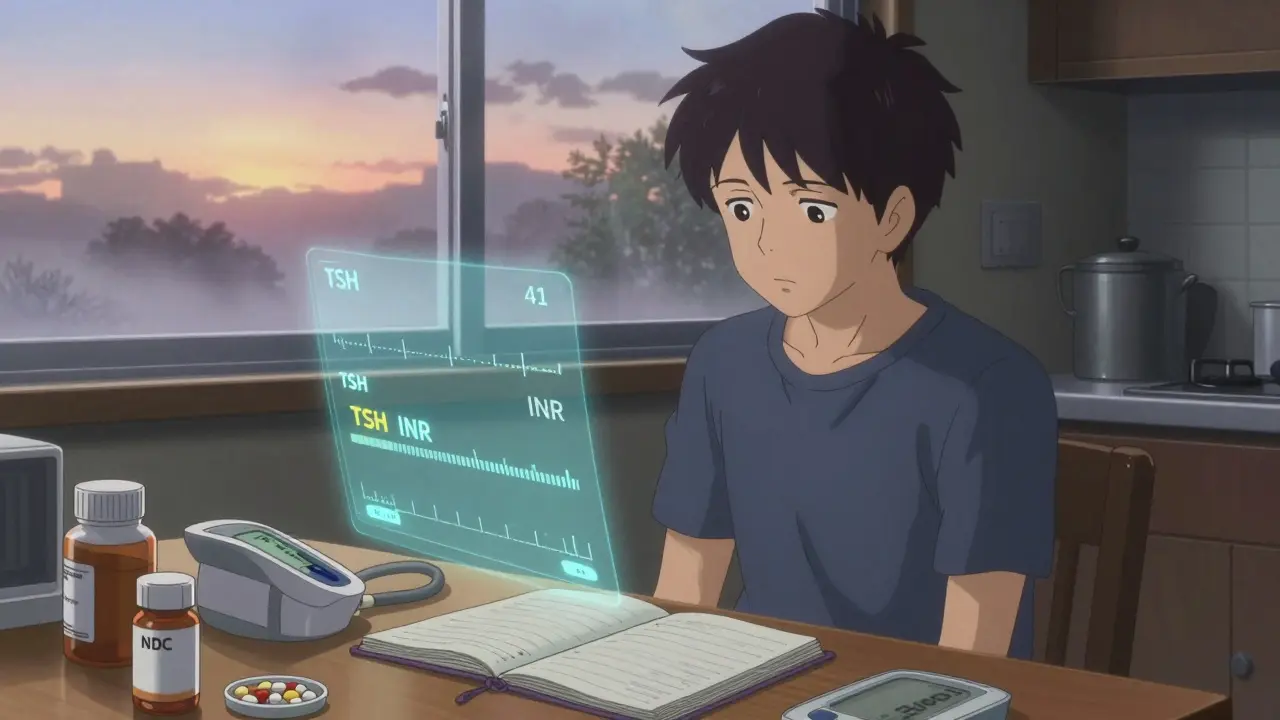
For most people, monitor for at least 30 days. For high-risk medications like thyroid, blood thinners, or epilepsy drugs, monitor for 60-90 days and get lab tests at 7-14 days and again at 30 days. Symptoms like mood changes, fatigue, or uncontrolled seizures should be reported immediately-don’t wait.
Yes. Two generics of the same drug can be made by different manufacturers with different fillers, coatings, or release mechanisms. Even though they’re both "generic," they may not perform identically in your body. Always check the NDC number on your prescription bottle. If it changes and you feel worse, talk to your doctor.
First, don’t stop taking it suddenly-this can be dangerous. Contact your doctor right away. Keep a log of your symptoms and any changes in how you feel. Ask your pharmacist for the NDC and lot number. Your doctor may request lab tests or suggest switching back to the brand-name version temporarily to confirm the issue.
Report issues to the FDA’s MedWatch program. You can file online at www.fda.gov/medwatch or call 1-800-FDA-1088. Include the drug name, manufacturer, NDC number, lot number, and a clear description of what happened. The FDA investigates all serious reports and uses them to improve safety.
Yes. You have the right to request that your prescription says "Dispense as Written" or "Do Not Substitute." Your doctor can write this on the prescription if they believe it’s medically necessary. Insurance may require prior authorization, but your health comes first.
I’ve been on generic levothyroxine for five years now, and I swear by it. But I get it-some folks feel different after a switch. I started keeping a little notebook like the post says: date, pill color, how I felt. One time, my new batch was a pale yellow instead of white, and I got this weird brain fog for a week. Turned out it was a different filler. I called my pharmacist, asked for the NDC, and they switched me back to the old manufacturer. No drama, just info. That’s all you need.
Generics saved me thousands a year. I’m not some rich guy who can afford brand names. But I’m also not dumb. If your body’s a finely tuned machine, treat it like one. Track it. Know your pills. Don’t just take what’s handed to you.
The FDA’s numbers are solid, but they don’t live in your skin. You do. So listen to yourself. Not the ads. Not the insurance reps. You.
OMG I can’t believe people are still debating this 😭
Generics are just Big Pharma’s way of poisoning the poor with chalk and glitter. I switched to a generic warfarin and my INR went from 2.3 to 4.8 in 3 days. I nearly bled out in my bathroom. The pill looked like a cartoon mushroom. I swear the manufacturer used crushed dreams as a binder.
They don’t want you to know-these pills are made in basements in Bangladesh by monkeys with lab coats. The FDA? A puppet. A joke. A corporate shill.
Bring back the brand. Or die trying. 💀
It is with profound respect for the integrity of patient autonomy and the sanctity of individual physiological response that I feel compelled to underscore the critical importance of the observations presented herein.
While the statistical data provided by the Food and Drug Administration may suggest a negligible rate of therapeutic failure, we must not conflate population-level metrics with the lived, embodied experience of the individual. Each person is a unique ecosystem-a symphony of biochemistry, psychological resilience, and environmental interaction. To dismiss a patient’s report of fatigue, mood dysregulation, or seizure recurrence as ‘anecdotal’ is not merely unscientific-it is ethically indefensible.
Moreover, the variation in inactive ingredients is not a trivial footnote. It is a profound biological variable. A dye that causes no reaction in one person may trigger an inflammatory cascade in another. A coating that alters dissolution kinetics may mean the difference between therapeutic efficacy and catastrophic relapse.
Let us not reduce healthcare to cost-efficiency metrics. Let us not normalize suffering as collateral. The call for monitoring, documentation, and advocacy is not alarmism. It is medicine at its most humane. Thank you for this vital reminder.
Been a nurse for 22 years. Seen it all.
Generic switch? Most folks are fine. But I’ve had three patients in the last year where switching their lamotrigine caused a full-on seizure storm. One guy went from zero seizures in 18 months to three in a week. He didn’t say anything till his wife dragged him in.
Don’t wait for a crisis. If you’re on one of those high-risk meds, check your labs at 7 days. Write down how you feel every day. Take a pic of the pill if you’re paranoid. It’s not crazy-it’s smart.
And yeah, if your new pill looks like a different candy, ask about the NDC. Pharmacies don’t always tell you when the manufacturer changes. You’ve got to be the detective.
Stay sharp. Your body’s not a spreadsheet.
In India, we have some of the best generic manufacturers in the world. Our pharmaceutical industry serves over 150 countries. How dare you suggest that Indian-made generics are unsafe? This is a Western paranoia, not science.
Our drugs are cheaper because we are efficient, not because we cut corners. The FDA approves them. WHO endorses them. Your fear is ignorance dressed as caution.
Do not shame the global supply chain that keeps your elderly parents alive. Be grateful, not suspicious.
lol i switched to generic bupropion last month and felt like a zombie for two weeks. didn’t say anything cause i thought i was just depressed again. then i saw this post and was like… ohhh. checked the bottle-different maker. switched back to the old generic and boom, i’m me again.
so yeah. pills can be sneaky. check the numbers. it’s free advice.
Wow. Someone actually wrote a novel about generic pills. Congrats, you win the Pulitzer for Overthinking Medications.
Look. I’ve taken 14 different generics in the last 5 years. One made me dizzy. One gave me a rash. One tasted like metal. I called my doc. They swapped it. Done.
You don’t need a spreadsheet. You need a doctor who listens. And if they don’t? Find a new one. Not a journal. Not an NDC tracker. A human.
Also, I’m from South Africa. We don’t even have brand names here. Just generics. And we’re still alive. So chill.
Everything is controlled. The FDA, the doctors, the pills. They want you to think you have choice. But you don’t. You take what they give you. And if you feel different, it’s because your soul is out of alignment. Not the pill.
Generics are a test. A test of faith. If you trust the system, you will be healed. If you doubt, you will suffer.
Stop tracking. Start praying.
Let’s be clear: this entire post is a masterclass in overengineering a non-issue. The FDA’s bioequivalence standards are among the most rigorous in the world. 80–125% AUC? That’s not a loophole-it’s a buffer zone designed for biological variance. Your body doesn’t absorb drugs like a syringe. It’s a wet, messy, hormonal, gut-flora-riddled mess. Of course your experience changes.
But that’s not the generic’s fault. That’s your physiology. You’re not a lab rat. You’re a human with circadian rhythms, stress hormones, and a liver that does whatever the hell it wants.
So yes, track your symptoms. But don’t blame the pill. Blame your sleep, your coffee, your anxiety, your diet, your menstrual cycle, your damn cat walking on your bed at 3 a.m.
And for the love of God, stop calling every side effect a ‘therapeutic failure.’ You’re not dying. You’re just… feeling things. That’s called being alive.
Also: emoji for mood tracking? 🤡
i switched to generic warfarin and my leg swelled up like a balloon. called my doc. they said it was probably the filler. switched back. done. no spreadsheets needed. just listen to your body.
They’re not just changing fillers. They’re changing the *frequency* of the pill. I read a leaked memo-generic manufacturers are embedding microchips to track compliance. That’s why I felt ‘off’ after switching. The chip was emitting low-level EMF waves that disrupted my pineal gland.
My TSH didn’t change. My cortisol did. That’s why I got migraines. The FDA knows. They’re covering it up. The same people who approved the opioid crisis are approving these pills.
Check your pill under a blacklight. If it glows? It’s not medicine. It’s a surveillance tool.
And if you think I’m crazy? Then why do all the generics have the same weird blue tint? Coincidence? I think not.
They’re watching. And they’re testing. On you.
