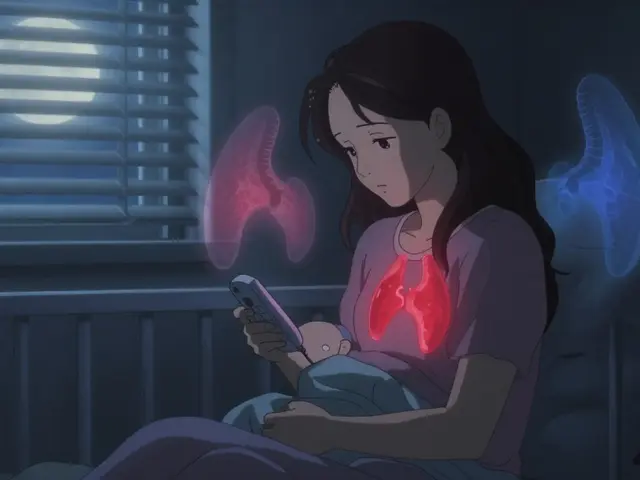
When you stop pills too soon, discontinuing a medication before your doctor says it’s safe. Also known as premature medication discontinuation, it’s one of the most common—and dangerous—mistakes people make with their health. It’s not just about forgetting a dose. It’s about deciding, often on your own, that you feel better so the drug isn’t needed anymore. But feeling better doesn’t mean the problem is gone. Antibiotics, antidepressants, blood pressure meds, and even birth control pills all need time to do their job. Stopping early can bring back symptoms, make them worse, or create new ones you didn’t have before.
Take antibiotics, drugs used to kill bacteria. When you stop them early, the toughest bacteria survive, multiply, and become resistant. That’s how superbugs form. The same thing happens with anticoagulants, blood thinners like warfarin or apixaban. Missing doses or quitting cold turkey raises your risk of clots, strokes, or heart attacks—even if you feel fine. And with antidepressants, medications that balance brain chemicals. Stopping suddenly can trigger dizziness, nausea, anxiety, or even suicidal thoughts. These aren’t side effects—they’re withdrawal symptoms, and they’re real.
It’s not just about the drug. It’s about your body’s adaptation. When you take a pill daily, your system adjusts. Remove it too fast, and your body doesn’t have time to readjust. That’s why restarting a drug after a break can be risky too—your tolerance drops, and you could overdose. This applies to opioids, benzodiazepines, even thyroid meds. Your doctor doesn’t give you a script just to check a box. They’re managing a biological process. Skipping it is like turning off a thermostat halfway through heating a house—you’ll never reach the right temperature.
And it’s not just you. People stop pills because of cost, side effects, confusion over pill changes, or because they don’t understand how long treatment takes. But the real danger isn’t the pill—it’s the assumption that you know better than the science. You might feel fine. But labs, scans, and blood tests don’t lie. That’s why tools like the medication adherence checklist and pharmacy refill records matter. They help you see the pattern, not just how you feel today.
If you’re thinking of stopping, talk to your doctor first. Don’t guess. Don’t Google. Don’t rely on peer attitudes or anecdotal stories. There are safe ways to adjust, switch, or taper—when done right. The posts below show you exactly what happens when people quit too early, how to spot the warning signs, and what to do instead. You’ll find real cases: people who stopped birth control and got pregnant unexpectedly, those who quit blood thinners and ended up in the ER, others who thought their depression was gone—until it came back harder. These aren’t hypotheticals. They’re lessons. And you don’t have to learn them the hard way.
Many people stop taking medications because of myths about side effects-like stopping antibiotics early or quitting statins over muscle pain. These myths are dangerous and preventable. Learn the facts, avoid risks, and stay healthy.