Many people believe that if a medication makes them feel weird, they should just stop taking it. That’s one of the most dangerous things you can do. Side effects are real-but so are the myths around them. And those myths are costing lives. Every year, over 125,000 people in the U.S. die from preventable causes linked to not taking their meds as prescribed. Most of those deaths aren’t because the drugs are unsafe. They’re because patients believed something that just isn’t true.
Feeling nauseous after taking your antibiotic? Dizzy after starting a new blood pressure pill? It’s natural to want to quit. But stopping abruptly can be worse than the side effect itself. The FDA says 10-20% of patients experience side effects from medications. That doesn’t mean the drug isn’t working-it means your body is adjusting.
Take antidepressants. About 56% of people who stop them suddenly develop withdrawal symptoms like dizziness, ‘brain zaps,’ or insomnia. These aren’t signs the drug isn’t right for you-they’re signs your nervous system is reacting to the sudden absence of the medication. A 2019 study in the Journal of Clinical Psychiatry found that most of these symptoms disappear if you taper off slowly under a doctor’s guidance.
Heart patients are especially at risk. A 2022 study in Circulation tracked over 14,000 heart attack survivors. Those who quit beta-blockers within 90 days because they felt tired or sluggish had a 3.2 times higher chance of having another heart attack. The fatigue? Often just your body recovering. The risk? Lifelong.
The fix? Talk to your doctor or pharmacist before stopping. Many side effects can be managed. Nausea from antibiotics drops by 68% when taken with food. Dizziness from blood pressure meds improves if you take them at night instead of in the morning. You don’t have to suffer-or risk your health.
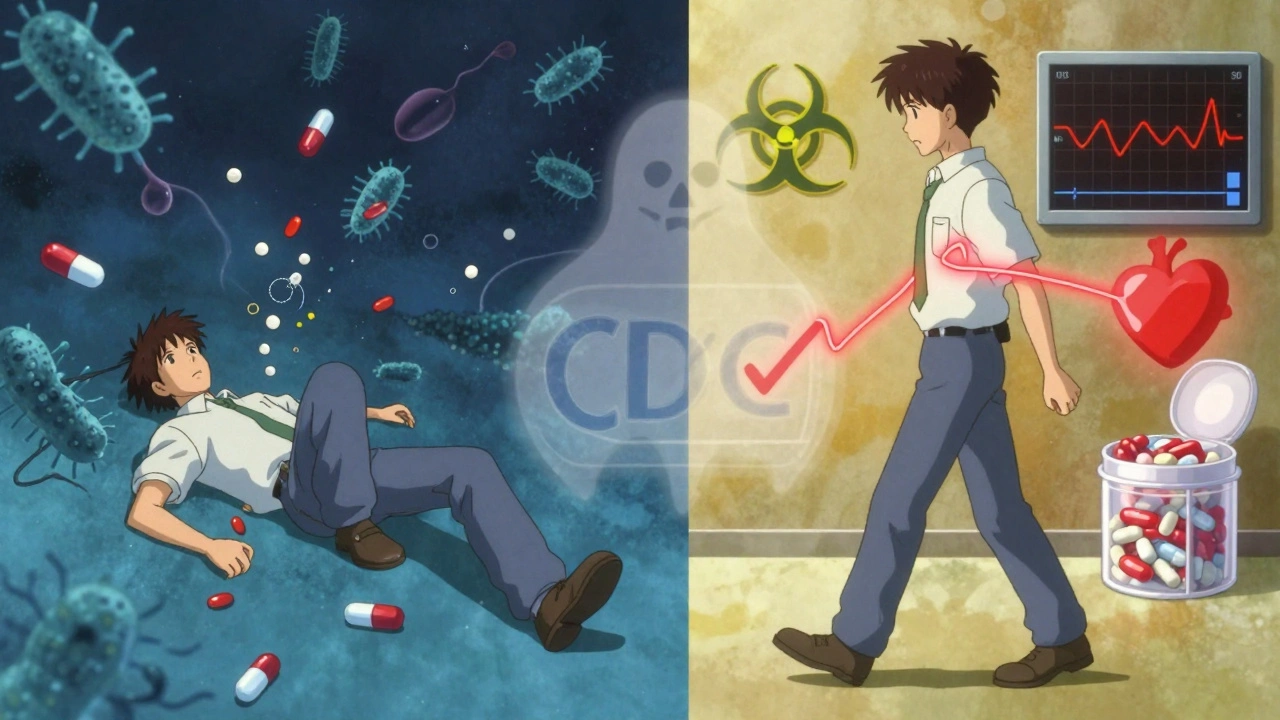
This one’s everywhere. You’ve got a bad cough. You take your pills for three days. You feel fine. So you toss the rest. Sounds smart, right? It’s not.
The CDC calls this the #1 driver of antibiotic resistance. When you stop early, you kill off the weakest bacteria-but the toughest ones survive. Those survivors multiply. And now they’re resistant to the drug. Every time you do this, you increase your chances of getting a future infection that won’t respond to treatment by 17%, according to a 2020 meta-analysis in The Lancet Infectious Diseases.
Here’s the science: Most bacterial infections need 7-14 days of antibiotics to kill 99.9% of the bugs. Feeling better doesn’t mean they’re gone. It just means your immune system is winning-temporarily. The remaining bacteria are still there, waiting to come back stronger.
A 2022 University of Utah survey found 63% of Americans think it’s okay to stop antibiotics early. Only 38% finish their full course. Meanwhile, 2.8 million Americans get antibiotic-resistant infections every year. 35,000 die. This isn’t theoretical. It’s happening in your community, your family, your own body.
The solution? Take every pill. Even if you feel fine. If you’re worried about side effects or cost, talk to your provider. They can switch you to a cheaper or gentler option. But don’t quit because you feel better.
Statins save lives. They lower cholesterol, prevent heart attacks, and reduce strokes. Yet 74% of people who start them quit within a year. Why? Because they think statins wreck their muscles.
Here’s what the data says: The Cholesterol Treatment Trialists’ Collaboration analyzed data from 174,000 patients across 27 studies. They found that only 0.9% more people on statins reported muscle pain than those on a placebo. That’s less than 1% difference. In real numbers: out of 100 people on statins, maybe one person has muscle discomfort that’s actually caused by the drug.
Here’s the twist: A 2018 study in the New England Journal of Medicine tested 90% of patients who claimed statins hurt their muscles. They were given statins again-blindly, without knowing if it was the real drug or a sugar pill. Most didn’t notice any difference. Their pain was likely due to the nocebo effect: expecting side effects made them feel them.
And not all statins are the same. Hydrophilic statins like pravastatin and rosuvastatin penetrate muscle tissue 70% less than lipophilic ones like simvastatin. If you’re having muscle issues, ask your doctor to switch you. You might not even notice the difference in effectiveness-but you’ll feel way better.
Don’t quit statins because you heard a story on Facebook. Talk to your doctor. Try a different type. Adjust the dose. But don’t walk away from a drug that’s proven to keep you alive.
You’ve got chronic back pain. You reach for ibuprofen. You take the max dose-1,200mg a day. Still hurting? You up the dose. You think, “It’s just a pill. How bad can it be?”
Here’s the truth: OTC painkillers are designed for short-term, mild pain. They’re not built for long-term, moderate-to-severe pain. A 2022 study in the Journal of Pain Research found that 68% of patients with chronic pain get little to no relief from OTC meds-even at the highest recommended doses.
And the risks? They’re real. Acetaminophen (Tylenol) causes 56,000 emergency room visits every year in the U.S. because people overdose-often by accident. Liver damage kicks in at just 4,000mg per day. That’s just eight 500mg pills. Easy to hit if you’re taking it for arthritis, migraines, or back pain over weeks or months.
Ibuprofen? Overuse leads to 10,000 hospitalizations a year for stomach bleeding. It’s not just “a little upset stomach.” It’s internal bleeding. The American Gastroenterological Association says it’s one of the top causes of GI emergencies in people over 50.
Yet 41% of chronic pain patients wait an average of 14.7 months before seeing a specialist. They think, “I’ll just tough it out with Advil.” By then, the pain has worsened. The damage has spread. The treatment is harder, more expensive, and less effective.
Don’t treat chronic pain like a cold. If OTC meds aren’t working after a week or two, see a doctor. There are safer, stronger options-like nerve-targeted meds, physical therapy, or low-dose antidepressants-that actually work for long-term pain.
It’s a comforting lie. “I didn’t do drugs-I just took my pills.” But prescription drugs aren’t safe just because a doctor wrote the script.
The National Institute on Drug Abuse says 53% of new opioid misuse cases in 2022 started with pills from a friend’s medicine cabinet. People think, “It’s legal, so it’s fine.” But prescription opioids carry a 23% risk of addiction after just 30 days of use, according to the American Society of Addiction Medicine.
And mixing them with alcohol? Deadly. A 2022 study in the Journal of Clinical Medicine found that combining prescription meds with alcohol increases the risk of death by 47%. Acetaminophen and alcohol together cause 450 liver failure deaths every year in the U.S. alone.
Prescription opioids killed 18,000 people in 2022. Thirty percent of those deaths involved people who weren’t even prescribed the drug. They got it from a relative, a neighbor, or a leftover bottle from an old surgery.
Illicit drugs like fentanyl are more dangerous per dose-but prescription drugs are easier to get. And that’s why they’re the gateway. The myth that “prescription = safe” is what lets people think it’s okay to share pills, take extra doses, or use them for fun.
Store your meds securely. Dispose of leftovers properly. Never take someone else’s prescription. And if you’re worried about dependency-talk to your doctor before it becomes a problem.

Side effects happen. That’s normal. But you don’t have to suffer-or quit.
Here’s what patients who stuck with their meds did:
The FDA recommends the “teach-back” method: after your doctor explains something, you repeat it back in your own words. If you can explain how to take your meds and what side effects to watch for, you’re more likely to stick with them. Studies show this improves adherence by 32%.
And here’s the best part: 63% of patients who stopped meds because of side effects were able to restart them successfully-once they got help. You’re not alone. And you don’t have to choose between feeling bad and staying healthy.
Technology is catching up. Smart pill bottles from AdhereTech send alerts to your doctor if you skip a dose. In a 2022 trial, this cut side effect-related quits by 47%.
Now there’s Proteus Discover-a pill with a tiny sensor that tells your phone when you took it. Combined with an app, it helps your care team adjust your plan in real time. A 2023 study in the New England Journal of Medicine found it improved side effect management by 63%.
The American College of Physicians just released 2024 guidelines pushing for “shared decision-making.” That means you and your doctor design your treatment plan together. Early results? A 52% drop in side effect-related discontinuations.
Medication isn’t one-size-fits-all. And side effects aren’t a reason to quit-they’re a signal to adjust. You’re not broken. Your treatment just needs tweaking.
ive stopped meds before and lived to tell about it so sue me
hey i get it-feeling like garbage on a new pill is terrifying. i was on an antidepressant that made me feel like a zombie with a headache for two weeks. i almost quit. but i talked to my pharmacist and switched the time i took it-from morning to bedtime. boom. no more dizziness. just a quiet night and a better morning. you don’t have to suffer. you just have to ask. and maybe try not taking it on an empty stomach. it’s not magic, it’s just science with a side of common sense
the entire premise is statistically naive. you cite studies like they’re gospel, but the FDA’s own data shows that 40% of reported side effects are psychosomatic. the nocebo effect is real, yes-but so is the confirmation bias of medical institutions clinging to profit-driven protocols. also, why is it always the patient’s fault for quitting? where’s the accountability for overprescribing? and why are we still using 1980s-era dosing algorithms in 2024? this isn’t medicine-it’s corporate choreography with a white coat
There’s a critical distinction here between anecdotal experience and population-level data. While individual side effects are valid and deserve attention, dismissing systemic adherence issues as mere ‘myths’ ignores the real psychological and socioeconomic barriers patients face-cost, access, misinformation, and provider communication gaps. The article rightly emphasizes patient agency, but true progress requires systemic reform, not just individual compliance. A well-informed patient is a powerful tool, but only if the system supports them.
my mom died because she stopped her blood thinner because she thought the dizziness was ‘just aging’… i’ve seen it. i’ve held her hand while she screamed because her body was shutting down from a clot that could’ve been prevented if someone had just told her to wait two weeks and call her doctor. please. just. talk. to. someone. before you quit. i beg you
As someone who has navigated the labyrinth of chronic illness across three continents, I must commend the nuanced approach of this piece. The emphasis on pharmacological individuality, the distinction between transient adaptation and true intolerance, and the call for collaborative decision-making are not merely clinical recommendations-they are ethical imperatives. The global burden of non-adherence is not a failure of patient willpower, but a failure of healthcare systems to personalize, communicate, and accompany. May this article be the catalyst for a more humane pharmacology.
ok so i’ve been on statins for 7 years and my muscles hurt so bad i could barely climb stairs. i went to my doc and they switched me to rosuvastatin and boom-no more pain. same cholesterol numbers. same heart protection. i didn’t quit, i upgraded. and guess what? my neighbor took her antibiotics for 3 days and got sick again with a superbug. she had to go to the hospital for IV drugs. i told her this story and now she finishes her pills. you don’t have to suffer. you just have to ask. and maybe don’t listen to random people on the internet. your pharmacist is your best friend. seriously. they know more than your google search. 🙌💊
you’re all just brainwashed by Big Pharma. the ‘side effects’ are the drug working exactly as designed-to keep you dependent. you think your doctor cares? they get paid per prescription. your ‘adjustment period’ is just the company buying time until you’re hooked. stop taking the poison. go natural. turmeric. ginger. sunlight. your body doesn’t need chemicals to heal. it needs freedom from corporate control. your death is their profit margin
There’s a grammatical inconsistency in the phrase: ‘a 2019 study in the Journal of Clinical Psychiatry found that most of these symptoms disappear if you taper off slowly under a doctor’s guidance.’ The modifier ‘under a doctor’s guidance’ is misplaced-it should be ‘if you taper off slowly, under a doctor’s guidance.’ Minor, but it undermines credibility when the rest of the piece is so meticulously sourced.
my buddy took his blood pressure med for 3 days, felt dizzy, tossed the rest. got a stroke a month later. he’s fine now, but walks with a cane. don’t be that guy. just call your doc. they’ve heard it all. it’s not a hassle. it’s what they’re there for. 🤝
in India we don’t have this problem. we take medicine when we feel like it. if it makes us feel worse, we stop. if it makes us feel better, we keep. no doctors, no apps, no expensive pills. our bodies know better than your western science. you think your studies matter? we’ve been healing for 5000 years without your lab rats and journals. this article is colonial medicine disguised as advice. go back to your pills and your data
listen-this isn’t about being ‘strong’ or ‘obedient.’ it’s about being smart. i was the guy who quit statins because my legs felt heavy. turned out i was dehydrated and sleeping wrong. changed my water intake, moved my pill to bedtime, and now i’m running 5Ks at 58. nobody told me to try that. i figured it out. but i didn’t quit. i tweaked. and that’s the whole damn point. your meds aren’t your enemy. your silence is. ask. adjust. don’t abandon.