When a pharmaceutical plant shuts down because a batch of pills has the wrong color coating, or a vial contains a foreign particle, it’s not a failure-it’s a safeguard. These moments, when production must stop due to quality problems, are the line between safe medicine and dangerous error. In 2023, the FDA issued over 300 warning letters to drugmakers citing inadequate quality control procedures, and nearly 40% of those specifically mentioned failed halt protocols. This isn’t about inefficiency. It’s about survival.
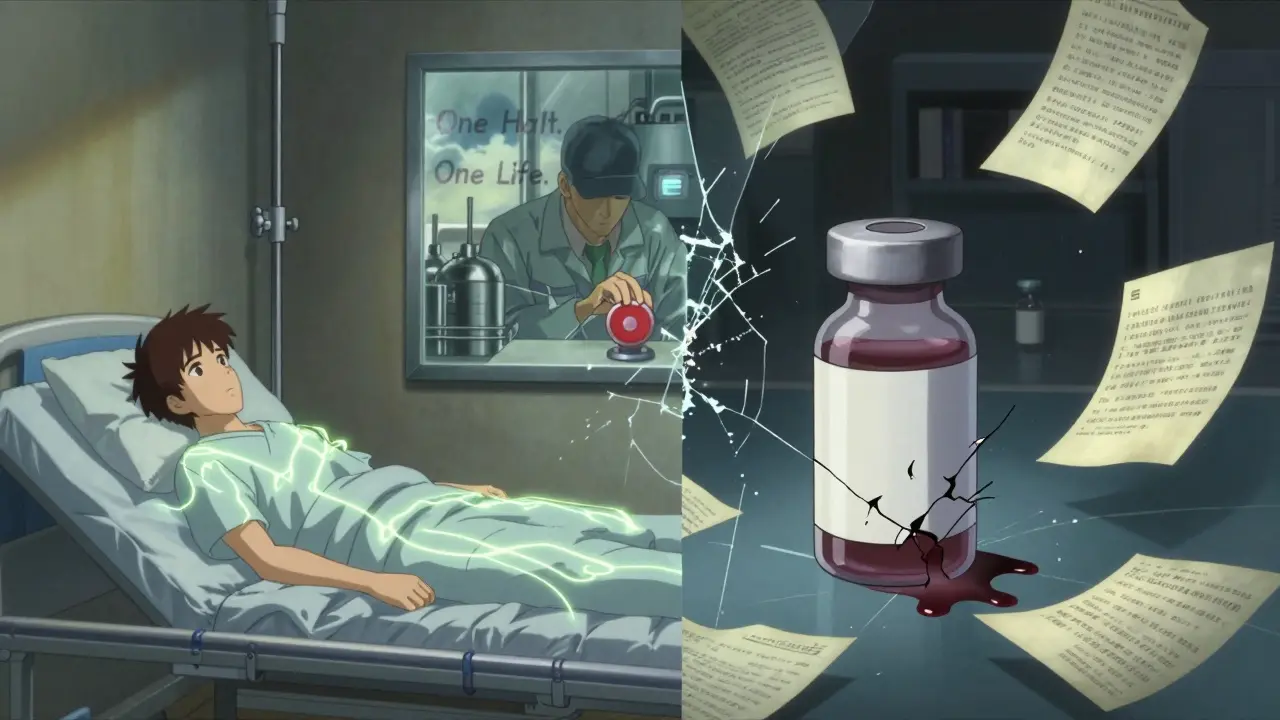
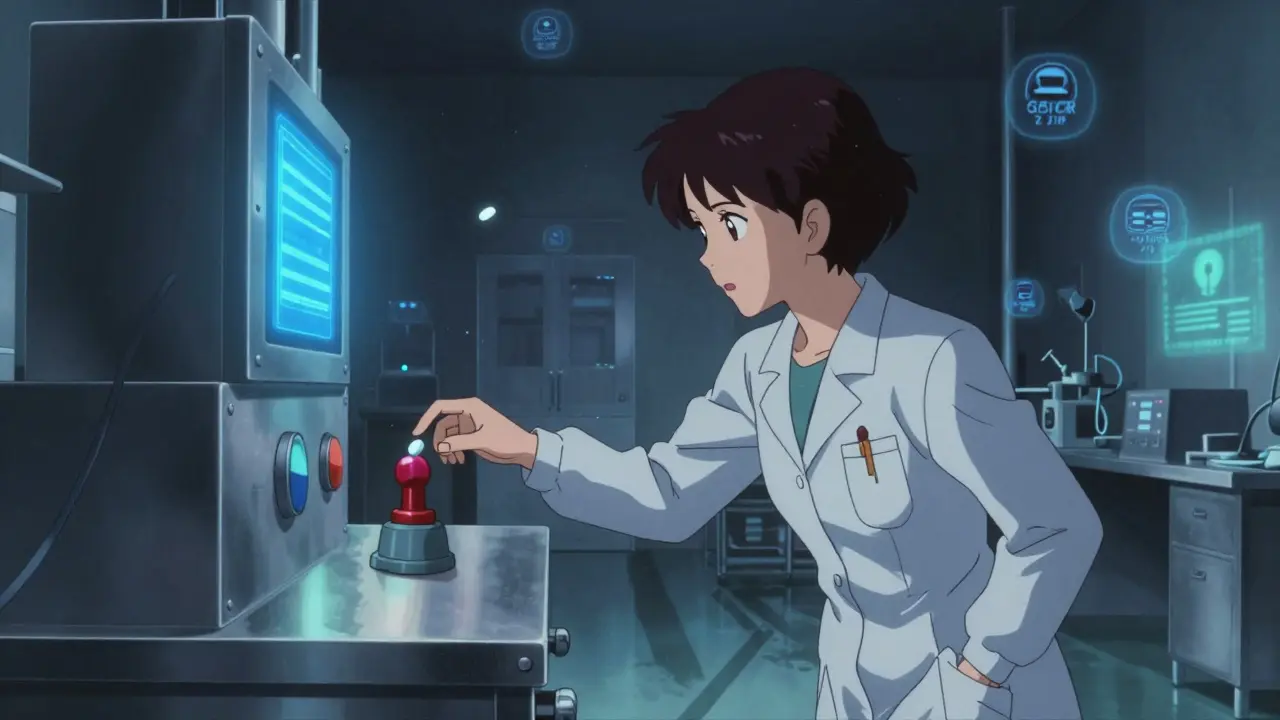
Pharmaceutical halts take longer because every step must comply with strict regulatory standards. After a halt, every affected batch must be quarantined, documented, tested, and reviewed by quality assurance teams. Regulatory bodies like the FDA require full traceability and root cause analysis before production can resume. Unlike electronics or automotive lines, where a machine can be restarted quickly, sterile environments, chemical processes, and patient safety protocols add hours to the process.
Yes-and they must. Even small manufacturers can start with low-cost solutions: digital checklists, basic sensors, and trained staff with stop-work authority. Many governments and industry groups offer free resources, like the Manufacturing Extension Partnership’s root cause analysis webinars. The real cost isn’t the system-it’s the recall. A single FDA warning letter can cost a small company its license. Investing in prevention is cheaper than surviving a crisis.
A maintenance shutdown is planned-for example, replacing a filter or servicing a pump. A quality halt is unplanned and triggered by a defect or deviation in the product or process. It’s not about equipment wear; it’s about safety. If a tablet’s active ingredient is 5% off-spec, it doesn’t matter if the machine is brand new. The line stops because the product is unsafe.
Regulators like the FDA and EMA see well-managed halts as a sign of a strong quality system. They don’t penalize companies for stopping-they penalize companies for not stopping. In 2023, 37% of FDA warning letters cited inadequate halt procedures. Companies that document halts properly, investigate root causes, and train staff are viewed as compliant and responsible. Ignoring problems is the real violation.
The number of halts is rising-not because quality is getting worse, but because detection is getting better. More sensors, better training, and stronger stop-work policies mean problems are caught earlier. In 2023, facilities using AI-driven quality systems reported 47% fewer *unnecessary* halts but 15% more *critical* ones. That’s progress. The goal isn’t fewer halts-it’s better halts.
Man, I’ve seen this firsthand in Philly-some small plant was cutting corners, and one batch of insulin had the wrong shade. Didn’t stop. Three people ended up in the ER. Now? They’ve got QR codes on every machine. No more paper logs. Just scan, read, do. Simple. Life-saving.
THE GOVERNMENT IS MAKING US STOP TO CONTROL US!! 🤯 They don’t care about patients-they care about lawsuits. Why can’t we just let people take the risk?? 😡 #FreedomToMedicate
Every halt is a heartbeat saved. In India, we used to bury mistakes under silence. Now I teach nurses to press that button like it’s their first breath. No shame in stopping. Only shame in pretending.
One must observe, with rigorous analytical precision, that the implicit assumption in this article-that quality halts are inherently virtuous-is not only unproven but dangerously reductive. The very notion of ‘zero tolerance’ is a statistical fallacy when applied to biological systems. Variance is inherent; the real failure lies in the institutionalization of fear over epistemic humility.
They're lying. Every single one of them. The FDA, the big pharma CEOs-they all know that these 'halts' are just cover for price hikes. They shut down production so they can jack up the price of insulin. They let people die on purpose. I read a leak once. The emails said 'delay until Q3'. That's not quality control. That's murder with a compliance badge. 😔
It’s profoundly troubling that this piece romanticizes bureaucratic inertia as moral superiority. The cult of the halt has become a shield for mediocrity. If your entire quality system depends on manual shutdowns, you’ve already failed. Real excellence is built into the process-predictive, elegant, invisible. This is not vigilance. It’s incompetence dressed in regulatory scrubs.
AI flags, humans decide-that’s the sweet spot. But let’s not kid ourselves: the human part is the bottleneck. We train technicians to recognize deviations, but we don’t train them to trust their gut. The machine sees a 0.1°C spike. The operator sees a memory of last week’s batch that smelled wrong. That’s tacit knowledge. And it’s being erased by KPIs and dashboards.
So wait-so if a vial’s got a speck of dust, you stop everything? Bro, that’s like shutting down a restaurant because someone sneezed near the salad bar. We’re talking about *microscopic* particles here. The air in my apartment has more junk than a cleanroom. Why’s this so sacred? 🤔
They say ‘stop-work authority’-but who’s really stopping? The guy on night shift? The one who’s scared to speak up because last time he did, his hours got cut? That’s not empowerment-that’s a trap. And don’t tell me about ‘digital logs.’ I’ve seen the tablets-they’re glitchy, the Wi-Fi drops, and the manager still yells at the tech for ‘causing delays.’ This whole thing is theater.
Can someone explain to me why the FDA doesn’t just mandate that every facility install real-time blockchain traceability from raw material to vial? It’s 2024. We track coffee beans from farm to cup. Why can’t we do this for life-saving drugs? Are we still using clipboards? Are we really?!
in Nigeria, we don’t have fancy sensors. But we have elders who’ve worked 40 years in a lab. They smell the batch. They touch the vial. They know. Sometimes, the best AI is a tired man who’s seen it all. Respect the hands, not just the machines. 🙏
Oh, so now we’re calling this ‘responsibility’? What a cute euphemism for ‘we’re too scared to admit we didn’t plan properly.’ Let’s call it what it is: a system that rewards panic over foresight. And hey, congrats on turning safety into a performance art.
Interesting perspective-but I must respectfully note that the data on false alarms is compelling. At our facility in Glasgow, we reduced unnecessary halts by 58% after implementing AI-driven trend analysis. The key? Not eliminating human input-but refining the signal-to-noise ratio. Machines don’t judge. Humans do. Together? Brilliant.
It’s not about halts-it’s about accountability. If you can’t produce a drug without contamination, you shouldn’t be making it. Period. The fact that we’re even having this conversation proves how far we’ve fallen from the days when quality was a creed, not a checkbox. Shame on the leaders who prioritize profit over purity.
Every time we stop, we’re not just protecting patients-we’re rebuilding trust. In a world where truth is optional, where corporations lie, where politicians spin, this is one of the last places where integrity still has teeth. This isn’t bureaucracy. This is the quiet, stubborn act of saying: ‘Some things are too sacred to rush.’
