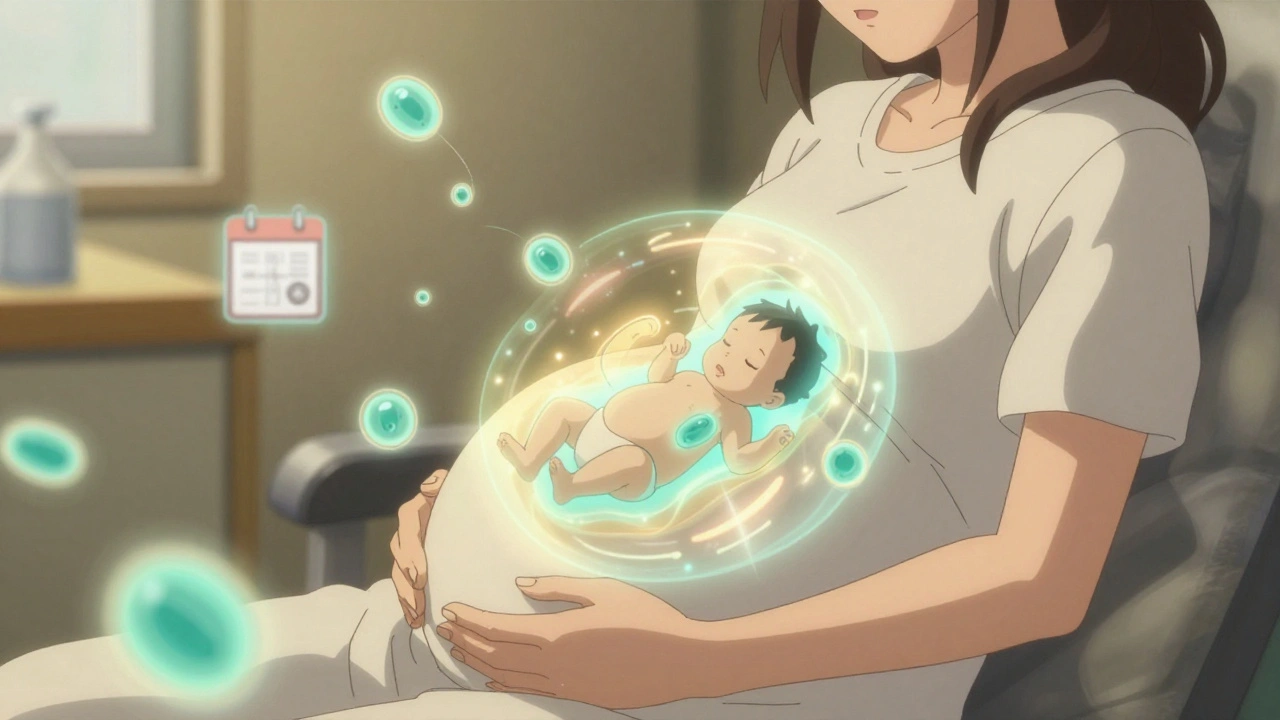
When you're pregnant, every decision feels bigger. Should you eat sushi? Is it safe to dye your hair? What about vaccines? The truth is, some vaccines aren't just safe during pregnancy-they're one of the best things you can do for your baby’s health. Yet, confusion still lingers. Many people worry about risks, timing, or whether the shots even work. The science is clear: getting the right vaccines while pregnant protects both you and your newborn in ways that post-birth shots simply can’t.
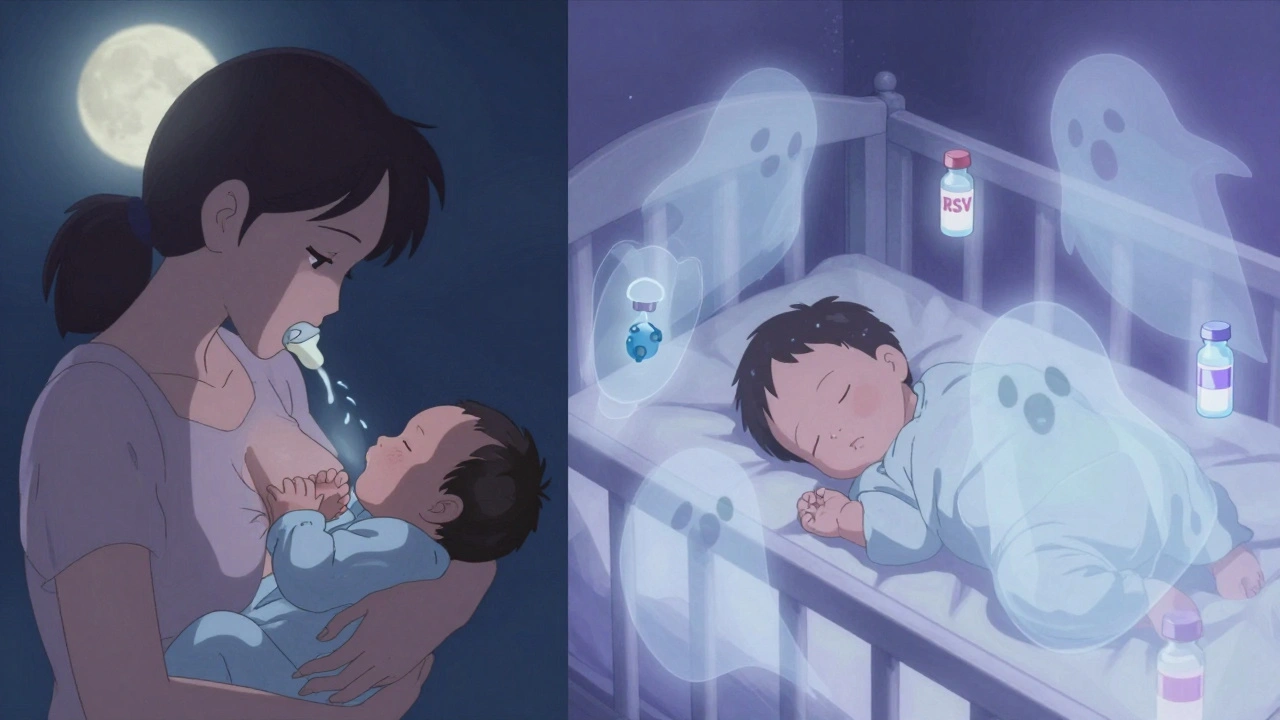

Yes. The inactivated flu vaccine is safe during any trimester, including the first. The CDC recommends getting it as soon as it’s available, ideally by October, to ensure protection through the peak flu season. There’s no increased risk of miscarriage or birth defects linked to flu shots in pregnancy.
You still need it during every pregnancy. Antibody levels drop over time, and the goal is to pass the highest possible amount to your baby right before birth. Even if you had Tdap five years ago, you’ll need another dose between 27 and 36 weeks of this pregnancy to protect your newborn.
No. There is no scientific link between vaccines given during pregnancy and autism in children. This myth stems from discredited studies from the late 1990s that have been thoroughly debunked. Multiple large-scale studies involving over 1.5 million pregnant women and their children found no increased risk of autism from flu, Tdap, or COVID-19 vaccines.
Yes, especially if your baby will be born in fall or winter. RSV causes over 58,000 hospitalizations each year in children under five in the U.S. For infants under six months, it’s the leading cause of hospitalization. The RSV vaccine reduces severe infection by nearly 70% in the first six months of life. If your provider offers it between 32 and 36 weeks, take it.
Yes. The flu, Tdap, and COVID-19 vaccines can be given on the same day, in different arms. The RSV vaccine can also be given at the same visit if you’re in the right window. There’s no evidence that combining them reduces effectiveness or increases side effects. Many clinics offer them together to make it easier.
Get it as soon as possible-even after 36 weeks. While antibody transfer is highest when given at 27-30 weeks, you still pass some protection even later. If you deliver before getting it, you can receive Tdap right after birth, but your baby won’t get the same level of passive immunity. It’s better to get it during pregnancy.
so like... vaccines n pregnancy? i mean i get the science but it still feels weird. like my body's not just mine anymore? idk. got the flu shot last year, arm hurt for a day. baby's fine. that's all i need.
The data is overwhelming. Over 2.3 million pregnancies reviewed across 147 studies. No credible safety signals for inactivated or mRNA vaccines. The placental transfer of antibodies is a biological imperative-not an experiment. If you're avoiding vaccines because of misinformation, you're not protecting your child-you're exposing them to preventable risks that have been quantified, measured, and debunked for decades.
I just... I can't stop thinking about thimerosal. I know it's been removed, but what if... what if they're lying? What if the 'studies' are funded by Big Pharma? I read a blog post once that said the CDC deletes negative data... and now I just... I don't know. I'm scared. I'm so scared.
I got the Tdap at 28 weeks and the RSV at 34 weeks. My baby is 3 months old and has never been sick. I cried when the nurse handed me the vaccine info sheet. I felt like I was giving him armor. You're not just protecting yourself-you're giving your baby a fighting chance before they even take their first breath. Do it. Please.
They say 'safe' but they never say WHO approved it. Who's really behind this? Are you sure the mRNA isn't altering your DNA? I saw a video where a scientist said the spike protein lingers for months. My cousin's friend's neighbor had a stillbirth after the booster. Coincidence? I think not.
In India, maternal vaccination uptake is still low due to misinformation and access barriers. But the data is universal. The WHO recommends Tdap and flu vaccines in pregnancy globally. The mechanism of passive immunity is conserved across populations. We must scale education, not skepticism. Your baby's first immune response begins in utero. Don't let cultural myths override biology.
If you're dumb enough to get a shot while pregnant you deserve what you get. My sister had a seizure after the flu jab and her kid had jaundice. Coincidence? Nah. You're playing Russian roulette with your baby's brain.
Got my shots at 29 weeks. No side effects. Baby is healthy. You're not a lab rat. You're a mom. And moms protect their babies. Even before they're born.
I got the COVID shot at 12 weeks. Had a headache for 12 hours. That’s it. My daughter is 1 now and she’s never had a cold. I’ve seen people panic over nothing. The science isn’t perfect-but it’s better than the alternative. 🤍
i got the rsv shot and then my arm was kinda sore but like... worth it? my lil one was in the icu last year with rsv. i didnt know then. now i do. dont wait. just do it.
Why are we pushing vaccines on American mothers? In my country, we don't do this. We trust nature. This is just another way for the government to control us. You think your baby is safe? They're just guinea pigs for corporate profit.