
Chronic back pain isn’t just a sore back that won’t go away. It’s pain that lasts longer than 12 weeks - long after an injury should’ve healed. About 8% of adults in the U.S. live with it, and for many, it’s not just physical discomfort. It’s sleepless nights, missed work, and the slow erosion of daily life. The good news? You don’t have to just live with it. A mix of physical therapy, smart medication use, and daily self-management can bring real, lasting relief - if you know how to use them together.
Yes. Even if your pain has lasted for years, your body can still learn to move differently. Physical therapy doesn’t just treat the spine - it retrains your nervous system. Studies show people with pain lasting over 5 years still get 40-60% improvement with consistent therapy and home exercises. The key isn’t how long you’ve had it - it’s whether you’re willing to show up every day.
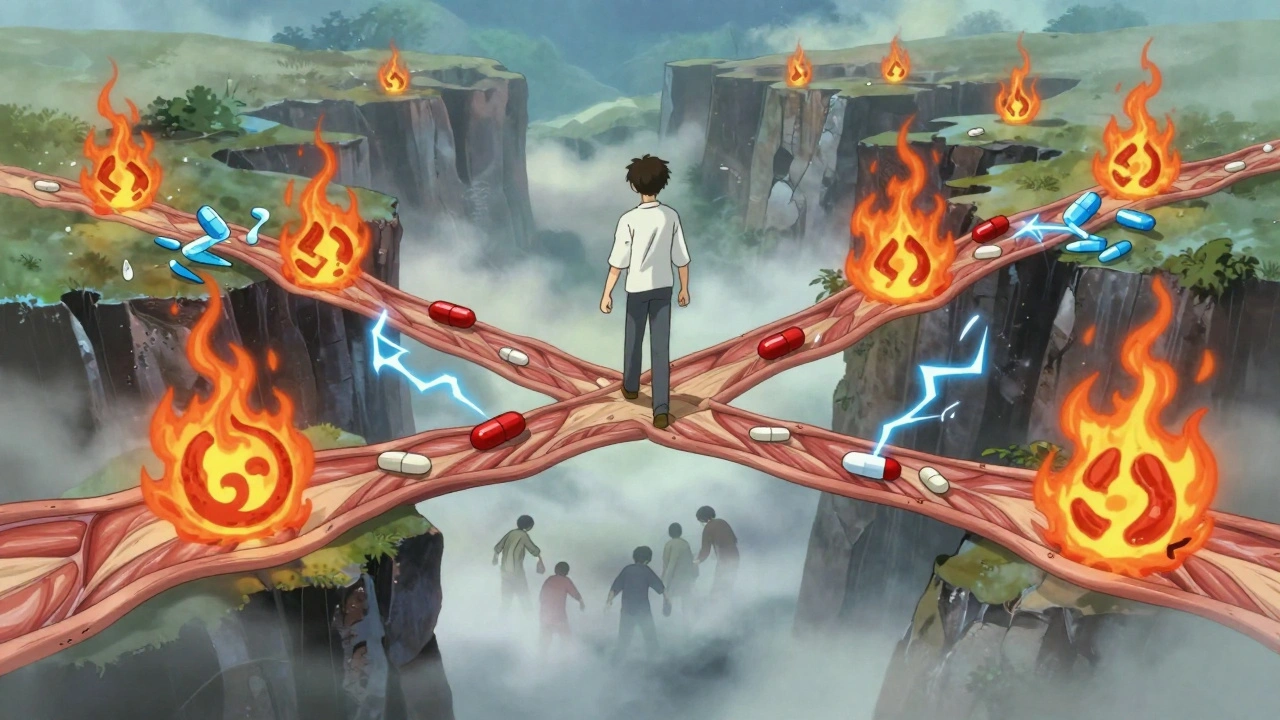
No medication is completely free of side effects. NSAIDs can harm your stomach or kidneys. Gabapentin causes drowsiness. Duloxetine can make you nauseous. But some options are safer than others. Topical NSAIDs (like diclofenac gel) have fewer systemic effects. Acetaminophen is gentler on the stomach than ibuprofen. And non-drug options - like heat, movement, and mindfulness - have zero side effects. The goal isn’t to find a perfect pill. It’s to find the least harmful option that gives you enough relief to move.
Long-term opioid use can cause opioid-induced hyperalgesia - where your body becomes more sensitive to pain. But even non-opioid meds can contribute. If you take NSAIDs daily for months, your body may stop responding as well. Also, relying on pills can make you avoid movement, which weakens muscles and makes pain worse. The body adapts. If you’re taking meds but not moving, you’re training your body to be more fragile. That’s why meds work best when paired with PT and self-management.
If your insurance limits sessions, yes - especially if you’re serious about long-term relief. A 2024 study found that people who paid for extra PT sessions had 30% better outcomes than those who stopped at their insurance limit. The average cost is $75-$120 per session. But think of it as an investment. One year of chronic pain costs the average person $10,000 in lost work and other expenses. A few extra PT visits could save you more than that.
Only consider advanced options after trying PT, medication, and self-management for at least 6 months - and only if your pain is severely limiting your life. Injections (like epidurals) can give temporary relief for nerve pain. Surgery is rarely needed for back pain alone. Most people who get surgery still need PT afterward. The real question isn’t whether you’re a candidate - it’s whether you’ve fully committed to conservative care first. Most surgeons won’t operate unless you’ve tried everything else.
Absolutely. Stress doesn’t cause back pain, but it amplifies it. When you’re stressed, your muscles tense up. Your nervous system becomes hypersensitive. That’s why people with chronic pain often say their pain spikes during work deadlines or family conflicts. Managing stress isn’t optional - it’s part of treatment. Breathing exercises, short walks, or even 10 minutes of quiet time each day can reduce pain signals by 20-30%. You don’t need to be zen. You just need to pause.
Next steps: Start tracking your pain for one week. Note what you did, what you took, and how you felt. Bring it to your next appointment. That small step can change everything.
I’ve been dealing with this for 7 years and honestly, the PT was the only thing that didn’t make me feel like a lab rat. The exercises felt silly at first-like doing planks while breathing weird-but after 3 months, I could carry groceries without wincing. No magic pill, just consistency.
Also, tracking my pain in a notebook helped me see patterns I never noticed. Turns out, bad sleep and coffee after 2pm were my real enemies.
One must question the epistemological foundation of this article’s implicit utilitarianism. The conflation of ‘relief’ with ‘functionality’ presumes a Cartesian dichotomy between mind and body-a framework increasingly discredited in phenomenological pain studies. Furthermore, the privileging of physical therapy as ‘first-line’ reflects a biomedical hegemony that pathologizes subjective experience under the guise of evidence-based practice. One wonders: who benefits from this paradigm?
Let me be perfectly clear: if you’re taking NSAIDs daily for more than 14 days straight, you’re not managing pain-you’re gambling with your kidneys and stomach lining. And don’t even get me started on people who think gabapentin is a ‘chill pill.’ It’s a neuro-modulator with a 30% dropout rate due to brain fog. If you’re too lazy to do 15 minutes of core work every day, stop complaining about your back.
Also, ‘SpineSurvivor22’ switched from gabapentin to duloxetine? Good. Because if you can’t function at work because you’re mentally underwater, you’re not ‘tolerating’ pain-you’re enabling it.
PT works for some but most of these studies are funded by clinics that sell PT. Real talk: if you’re paying $100 per session and only getting 20 visits, you’re being screwed. The real solution? Learn to sit properly. Stop slouching. That’s it. No fancy exercises. No pills. Just stop being a zombie at your desk.
Also, why does everyone act like self-management is a new idea? My grandma did this in the 70s with heat packs and walking. We just overcomplicate everything now.
Medications are crutches. PT is work. Self-management is discipline. Most people want a quick fix and then blame the system when it doesn’t work. You don’t need a study to tell you that sitting all day breaks your back. You just need to stand up. That’s it. No apps. No supplements. No magic.
Also opioids are evil. End of story.
Just started PT last week and already feel like a new person 😊
My therapist had me do this weird thing where I squeezed a towel between my knees while lying down… I thought it was dumb but now I can bend over to tie my shoes without groaning 🙌
Also bought a foam roller. Best $15 I’ve spent in years.
It’s fascinating how the modern medical-industrial complex has turned chronic pain into a productized experience: PT packages, medication regimens, app-based tracking, and now, even pain-themed Reddit communities. We’ve outsourced suffering to systems designed for efficiency, not healing. But the body doesn’t respond to spreadsheets. It responds to presence. To stillness. To the quiet, unquantifiable act of simply being with discomfort without trying to fix it.
Perhaps the real therapy isn’t in the exercises, but in the willingness to stop fighting-and start listening.
i did the 15 min thing every day for 3 months and now i can play with my kids without crying 😭 thank you for writing this
also i spelled everything wrong but you get the point lol
Discipline is the cornerstone of recovery. Physical therapy is not optional. It is a commitment to self. Medication may alleviate symptoms but only consistent movement rebuilds structural integrity. Self-management is not a suggestion-it is a responsibility. The body remembers what the mind neglects. Begin today. Not tomorrow. Not next week. Today.
I’m from California and I used to think back pain was just ‘adulting’ until I started doing the breathing thing before bed. Like, five minutes of slow inhale-hold-exhale? Changed everything.
Also I started walking around my block every night-no phone, just me and the stars. Turns out, nature doesn’t care if you’re in pain. It just keeps going. Kinda inspiring.
And yes, I cried during my first PT session. But I also laughed. And that’s more than I’ve done in years.