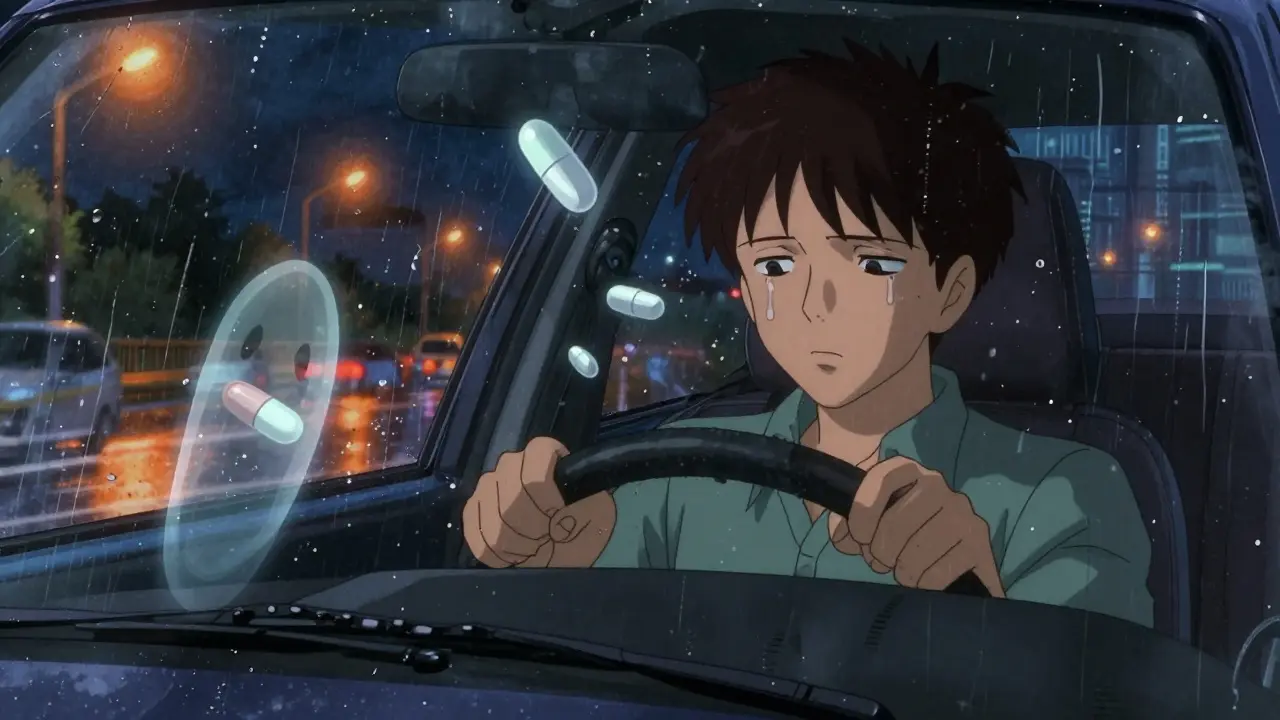
Driving while taking opioids isn’t just risky-it’s illegal in many places, even if the medication was prescribed by a doctor. You might think that if you’re taking your pills exactly as directed, you’re safe behind the wheel. But that’s not how the law or your body works. Opioids slow your reaction time, blur your vision, and make it harder to make quick decisions-exactly what you need when traffic suddenly changes. And the consequences? They can ruin your life in seconds.
Opioids don’t just make you sleepy. They dull your brain’s ability to process what’s happening around you. The National Institute on Drug Abuse says these drugs impair thinking, judgment, and coordination. Studies show that driving under opioid influence can double your risk of a crash. That’s not a small increase. That’s like driving with your eyes half-closed while texting.
Unlike alcohol, where we know a blood level of 0.08% means impairment, opioids don’t have a clear line. One person might feel fine on 10mg of oxycodone. Another might struggle to stay awake after 5mg. The same dose can affect people differently based on age, weight, tolerance, and whether they’re mixing it with other meds or alcohol. And that’s the problem-there’s no universal “safe” level.
Common side effects that matter while driving:
These aren’t side effects you can just “push through.” They’re biological changes your brain can’t override. Even if you’ve been on the same dose for months, your body’s response can change. A new prescription, a different pharmacy, or even a change in your sleep schedule can make you more impaired than before.
Many people assume DUI laws only apply to alcohol. They’re wrong. In the U.S., 16 states have zero-tolerance laws for opioids and other drugs. That means if there’s any trace of the drug in your system-even if you took it legally-you can be arrested. Five other states have per se laws, meaning any measurable amount above a certain threshold is automatically illegal.
Canada treats opioid impairment the same as alcohol impairment under its Criminal Code. In the UK, driving while impaired by any drug-prescribed or not-is illegal under the Road Traffic Act 1988. Police can pull you over if they suspect impairment, even without a breathalyzer test. They’ll use field sobriety tests, then send you for a blood or oral fluid sample.
Here’s the catch: some states let you defend yourself if you had a valid prescription. Utah says you’re not guilty if the drug was prescribed. Wisconsin requires you to prove you had a prescription and took it as directed. Georgia allows a defense for minors on therapeutic doses. But these exceptions are rare, hard to prove, and don’t guarantee you won’t be arrested. The officer doesn’t care if you’re following your doctor’s orders-they care if you’re impaired.
And it’s not just about being caught. In 2022, a survey of 1,247 chronic pain patients found that 63% didn’t know driving on opioids could lead to a DUI. One Reddit user shared how they failed a sobriety test after taking 5mg of oxycodone twice daily-exactly as prescribed. They lost their license for six months and paid $12,000 in legal fees.
Most doctors focus on pain relief, not driving safety. A 2022 study by the National Safety Council found that 72% of patients prescribed opioids received no counseling about driving risks. Pharmacists often give the same vague advice: “Don’t drive if you feel dizzy.” But what does that mean? When? How long?
The Mayo Clinic recommends waiting at least 3-4 hours after taking an immediate-release opioid like hydrocodone or oxycodone. For extended-release versions like OxyContin or fentanyl patches, wait 6-8 hours. But that’s just a guideline. Your body might metabolize the drug slower. You might be on other meds that interact. You might have slept poorly. All of that increases impairment.
And here’s the hidden risk: many people don’t realize their opioid prescription has changed. A refill might come from a different manufacturer. A generic version might have different fillers. Even small changes can affect how quickly the drug is absorbed. That’s why you can’t rely on past experience. Every new prescription needs a fresh assessment.

Police don’t have a breathalyzer for opioids. Instead, they use a three-step process:
Oral fluid testing devices like the Dräger DrugTest 5000, approved by the FDA in June 2023, are now used in 47 U.S. states. These can detect fentanyl, oxycodone, and other synthetic opioids in minutes. That means even if you think you’ve waited long enough, you could still test positive.
The big problem? There’s no scientific consensus on what blood level equals impairment for opioids. A level that’s safe for one person might be dangerous for another. That’s why zero-tolerance laws are so controversial. They punish people who are medically compliant but still legally impaired.
Here’s how to protect yourself:
California’s Office of Traffic Safety says: “If you plan to use an impairing drug, plan ahead for a sober driver.” That’s not advice. That’s a survival rule.

Lawmakers are catching up. In early 2024, seven more states were considering per se laws for opioids. The National Highway Traffic Safety Administration has invested $15.7 million in 2023 to train 5,000 more Drug Recognition Experts by 2025. The Transportation Research Board is pushing for scientifically validated blood limits for opioids within five years.
But the biggest threat isn’t the law-it’s the drugs themselves. Fentanyl, a synthetic opioid 50-100 times stronger than morphine, is now the most common drug found in impaired drivers. The DEA reports a 262% increase in fentanyl-related driving incidents between 2020 and 2023. These aren’t prescription pills anymore. They’re often counterfeit pills sold as oxycodone. You don’t even know what you’re taking.
Companies like UPS have already changed their policies. Since 2021, they require mandatory medical reviews for any employee prescribed opioids. Result? A 37% drop in medication-related incidents. That’s what happens when safety comes before convenience.
If you’re stopped and asked if you’ve taken any drugs, you have the right to remain silent. Don’t admit to anything. Don’t say “I’m on pain meds.” That’s evidence. Ask for a lawyer. Don’t consent to a blood draw unless ordered by a judge. But understand this: refusing a test can lead to automatic license suspension in most states.
If you’re charged, get a lawyer who understands drug-impaired driving cases. General DUI lawyers often don’t know the difference between alcohol and opioid impairment. You need someone who understands pharmacology, lab testing limits, and how prescription defenses work in your state.
And if you’re worried about your ability to drive safely-talk to your doctor about alternatives. Non-opioid pain management, physical therapy, or nerve blocks might be safer options. Your life is worth more than a prescription.
Legally, it depends on your state. Medically, it’s never safe. Even if your doctor says it’s okay, opioids slow your reaction time and impair judgment. Many people get arrested for DUI even when taking their medication exactly as directed. The safest choice is to avoid driving entirely while on opioids.
There’s no universal answer. For immediate-release opioids like hydrocodone or oxycodone, wait at least 3-4 hours. For extended-release versions like OxyContin or fentanyl patches, wait 6-8 hours. But individual metabolism varies. If you feel drowsy, dizzy, or foggy, don’t drive-even if it’s been hours. Your body’s response matters more than the clock.
Yes. In every U.S. state, Canada, and the UK, driving under the influence of any impairing drug is illegal-even if it’s legal to possess. Prescription opioids, benzodiazepines, sleep aids, and even some over-the-counter antihistamines can lead to a DUI if they affect your ability to drive safely.
Not always. A 2022 survey found that 63% of chronic pain patients didn’t know driving on opioids could lead to a DUI. Many patients say their pharmacists downplayed the risks. The FDA now requires “Do Not Drive” warnings on all opioid packaging since 2020, but the message still doesn’t reach everyone. Always ask your doctor, don’t just rely on the label.
Don’t drive. Plan ahead. Use public transit, rideshare apps, or ask a friend or family member to drive you. If you’re on long-term opioids, consider switching to non-opioid pain treatments. Your safety and legal standing are more important than the convenience of driving yourself. There are no exceptions that outweigh the risk.
Bro, I took oxycodone for a herniated disc and drove to Walmart. Got pulled over. Blood test showed 12ng/mL. Zero-tolerance state. Lost my license. Paid $14k. Now I take ibuprofen and cry in the shower. 🤡💊
Don't drive on opioids. Period.
They want us to be passive little sheep, don't they? 'Don't drive' they say. But what about personal responsibility? I'm a veteran, I've seen combat. I know my body. If I feel fine, I drive. The government's scared of real men who don't beg for permission. This isn't Sweden, folks. We used to have guts.
Now they want to drug-test every person who takes a pill? Next they'll scan your pupils at the DMV. Wake up. This is tyranny dressed in medical jargon.
Interesting how they say 'never safe' but then give exact time windows like 3-4 hours. That's a contradiction. If it's never safe, then why even pretend there's a safe window? The whole thing is a scam to make you feel guilty so you'll take less pain meds and they can save money on disability payouts.
Also, fentanyl in counterfeit pills? Yeah, but so what? People die from contaminated street food too. That doesn't mean we ban food. We just learn to be careful. This is just fearmongering dressed as public safety.
As someone from India where opioids are tightly controlled but pain is often untreated, I’ve seen both sides. In the U.S., there’s this strange mix of medical access and legal paranoia. You can get a 30-day supply of oxycodone like it’s coffee, but drive after taking it and suddenly you’re a criminal? Meanwhile, in rural India, people with chronic pain walk miles to a clinic that doesn’t even have morphine. So yes - the laws here are harsh, but the problem isn’t the laws. It’s the lack of education. Doctors don’t train on this. Pharmacists don’t explain. And patients? They’re left guessing. If we want real safety, we need mandatory pre-prescription driving-risk counseling - not just a footnote on a label. This isn’t about control. It’s about competence.
Hey - if you're on opioids and you're even slightly unsure about driving, don't. It's not worth it. I used to be a paramedic. I've seen the aftermath of crashes where someone thought 'I'm fine' after a pill. You're not fine. Your brain is fogged. Your reflexes are slow. You're not 'tough' - you're just lucky so far. Get a rideshare. Call a friend. Sleep in your car if you have to. Your life matters more than your pride.
And if your doctor won't talk to you about this? Find a new one. A good doctor doesn't just write prescriptions - they protect you.
Oh my god. Another one of these 'I'm on pain meds so I'm special' people. You're not special. You're a walking liability. If you can't manage your meds without endangering others, then maybe your pain isn't worth risking someone else's child's life. You think you're being brave? You're being selfish. And yes, I'm judging you. Because I'm not the one driving while drugged.
Zero tolerance for opioids? Good. America is soft. We need to stop coddling people who can't handle their own prescriptions. If you can't drive sober, don't drive. Period. No excuses. No 'but my doctor said-' Shut up and get a Uber.
Let’s be real - this whole thing is about control. They don’t care if you’re safe. They care if you’re obedient. If you take a pill and still move your body, you’re a threat to the system. The DREs? The lab tests? The ‘zero tolerance’ laws? They’re not about safety. They’re about power. They want you to feel guilty for existing in pain. And the worst part? You’re buying it. You’re reading this, nodding along, and still wondering if you’re a bad person. You’re not. The system is.
Thank you for writing this. 💙 I’ve been on long-term opioids for 8 years. I’ve never driven after taking them. Not once. I used to think I could 'tough it out' - until I nearly rear-ended someone while my vision blurred. I didn’t even realize it until the horn blared. That day changed everything. I started keeping a log. I talk to my pharmacist. I use Lyft. I don’t feel guilty - I feel responsible. And honestly? It’s peace of mind. You don’t have to be perfect. You just have to be honest with yourself.
Actually, the science is more nuanced. The NIDA study they cited? It’s a meta-analysis with high heterogeneity. And the 'doubling of crash risk' - that’s relative risk. Absolute risk is still low for low-dose, stable users. The real issue is polypharmacy and lack of pharmacokinetic education. Also, the Dräger device? It detects metabolites, not active drug. A positive test doesn't equal impairment. The legal system conflates presence with intoxication. That’s why so many people get wrongfully convicted. This isn’t about safety - it’s about bad science and bad policy.
Let’s deconstruct the cognitive dissonance here: The FDA mandates ‘Do Not Drive’ warnings, yet physicians still prescribe opioids without behavioral risk mitigation. This is a systemic failure of risk communication. The patient is not the agent of harm - the healthcare infrastructure is. The absence of standardized pharmacological competency training for prescribers creates a liability cascade. The state’s zero-tolerance statutes are merely reactionary band-aids on a wound caused by institutional negligence. Until we mandate DEA-certified opioid risk education for prescribers, we’re just criminalizing patients for a system’s incompetence.
My dad’s on fentanyl patches. He hasn’t driven in 3 years. He says it’s not worth the risk. I told him I’d drive him anywhere. Now we watch old movies and eat ice cream on Thursday nights. He says it’s better than driving anyway. 💕
