
When you’re nauseous from chemotherapy, surgery, or even a bad case of food poisoning, antiemetics like ondansetron (Zofran) can be a lifesaver. But if you’re also taking an SSRI for depression or anxiety, that same medication might be quietly pushing your body toward a dangerous condition called serotonin syndrome. It’s not common-but when it happens, it can turn deadly in hours.
No, ondansetron alone is extremely unlikely to cause serotonin syndrome. It’s designed to block serotonin receptors, not activate them. Almost all documented cases involve a combination with another serotonergic drug-like an SSRI, SNRI, or MAOI. The risk comes from drug interactions, not single-agent use.
You can find out through a simple genetic test, often done with a cheek swab. Many hospitals and pharmacists now offer pharmacogenomic testing, especially if you’re on multiple medications. If you’re of European descent and have had unusual side effects from antidepressants or antiemetics, ask your doctor about testing. About 7-10% of people in this group are poor metabolizers.
Not immediately. SSRIs stay in your system for days or even weeks after you stop them. Fluoxetine, for example, can linger for up to 4 weeks. Wait at least 2 weeks after stopping an SSRI before taking ondansetron. If you’re switching from one antidepressant to another, consult your doctor-some require longer washout periods.
Stop all serotonergic medications immediately and go to the nearest emergency room. Do not wait for symptoms to worsen. Bring a list of all your medications, including supplements. Tell them you suspect serotonin syndrome. Early treatment with cyproheptadine and supportive care can prevent serious complications.
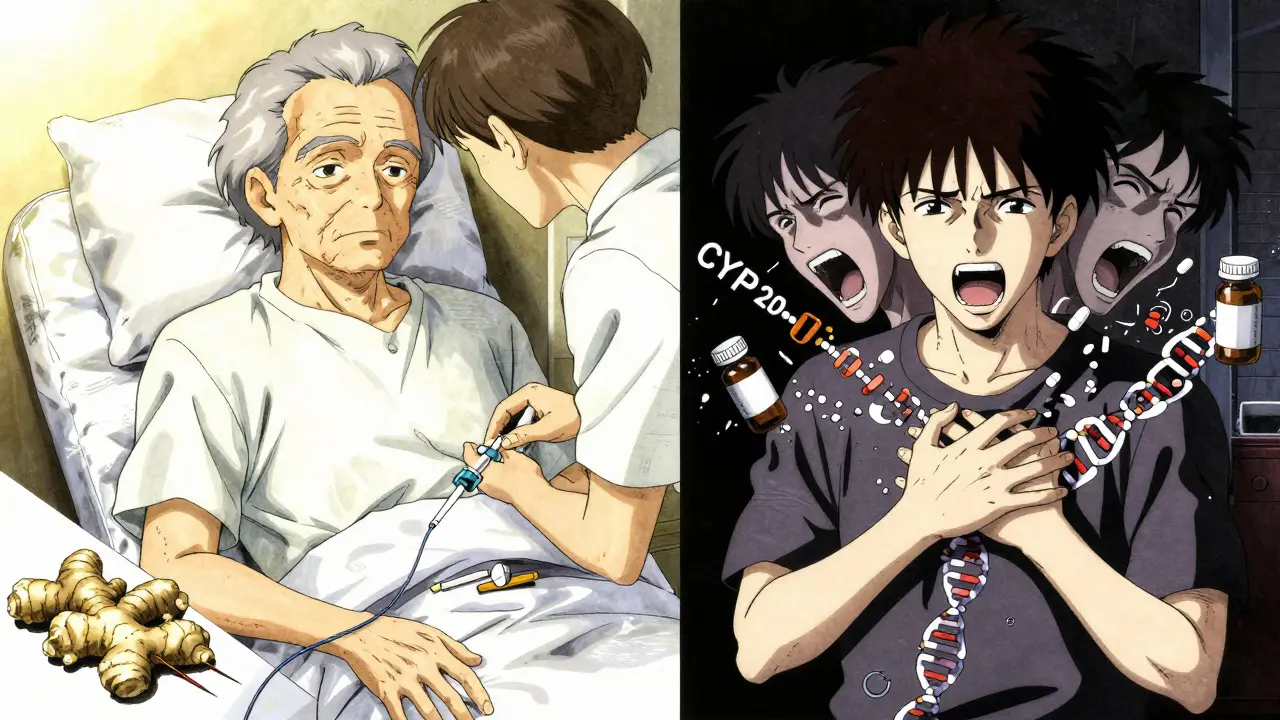
Yes. Ginger supplements (1,000-1,500 mg daily) are backed by clinical studies for nausea from pregnancy, chemo, and surgery. Acupuncture and acupressure (specifically the P6 point on the wrist) also show good results. For mild nausea, peppermint tea or deep breathing exercises can help. These don’t interact with serotonin and are safe with SSRIs.
So let me get this straight - we’re telling people to avoid a $5 anti-nausea pill because some lab rats in a 2020 Mayo study said it might kinda sorta glitch serotonin pathways if you’re already on antidepressants? Meanwhile, my grandma takes Zofran after chemo like it’s candy and still kicks ass at bingo. This feels like medical fearmongering dressed up as science. Also, why is everyone acting like serotonin is some sacred liquid god? It’s just a neurotransmitter. We’re not summoning Cthulhu here.
It is imperative to underscore the clinical significance of serotonin syndrome as a potentially life-threatening iatrogenic condition. The pharmacokinetic interactions between selective serotonin reuptake inhibitors (SSRIs) and 5-HT3 antagonists such as ondansetron are well-documented in peer-reviewed literature, including the FDA Sentinel Initiative data referenced. Furthermore, the CYP2D6 polymorphism, which affects up to 10% of individuals of European descent, significantly alters drug metabolism and necessitates personalized dosing strategies. The American Society of Health-System Pharmacists’ recommendations are evidence-based and should be strictly adhered to in clinical practice.
bro i took ondansetron after my surgery and im on zoloft and nothing happened like at all
maybe its just me but i think the fear is way overblown
also why is everyone so scared of drugs like its 1999
ginger tea works fine for me anyway
Oh please. This whole post is Big Pharma’s distraction tactic. They know Zofran is cheap and profitable so they bury the warning in a footnote. Meanwhile, the real danger? The CYP2D6 genetic test costs $300 and insurance won’t cover it unless you’re rich. And guess who gets tested? White people with good insurance. Black and Latino patients? They just get the pill and hope. This isn’t medicine - it’s genetic class warfare. And don’t even get me started on how palonosetron is just the same drug with a new label and a 10x price tag. They’re milking the fear, not protecting you.
Man I saw this same thing happen to my cousin in Lagos - they gave him Zofran after his chemo and he started shaking like he was possessed. Took him 3 days to come out of it. But here’s the twist - the hospital didn’t even ask if he was on antidepressants. They just assumed he was poor so he couldn’t afford them. That’s the real tragedy. We’re not talking about science here. We’re talking about who gets to live and who gets to be a statistic.
How is it that we live in a world where a drug designed to block serotonin receptors can somehow, under the right constellation of genetic and metabolic conditions, accidentally become a serotonin accelerator? It’s not just pharmacology - it’s cosmic irony. We’ve weaponized biology with the precision of a toddler with a matches. And yet, we still trust doctors who memorize drug names like they’re spellbooks. I don’t need a CYP2D6 test. I need a new species. One that doesn’t trust molecules with names longer than their soul.
my doc just gave me ondansetron last week and i’m on lexapro
no probs
but then again i’m a 23 y/o gym bro so maybe my liver is a tank
also why is everyone so into genetic testing like its the new horoscope
just dont take it with MAOIs and youll be fine
stop overthinking your meds
The entire discourse around serotonin syndrome reveals a deeper epistemological crisis in modern medicine: we treat pharmacology as a deterministic system when it is, in fact, a chaotic, nonlinear ecosystem of receptor dynamics, genetic variance, and metabolic entropy. The CYP2D6 polymorphism isn’t a footnote - it’s a mirror held up to the hubris of population-based prescribing. We reduce individuals to metabolic averages and then wonder why adverse events persist. The solution isn’t more drugs or more tests - it’s the radical humility to admit that biology refuses to be simplified into bullet points. Dexamethasone isn’t safer because it’s ‘non-serotonergic’ - it’s safer because it doesn’t pretend to control what it cannot understand.