
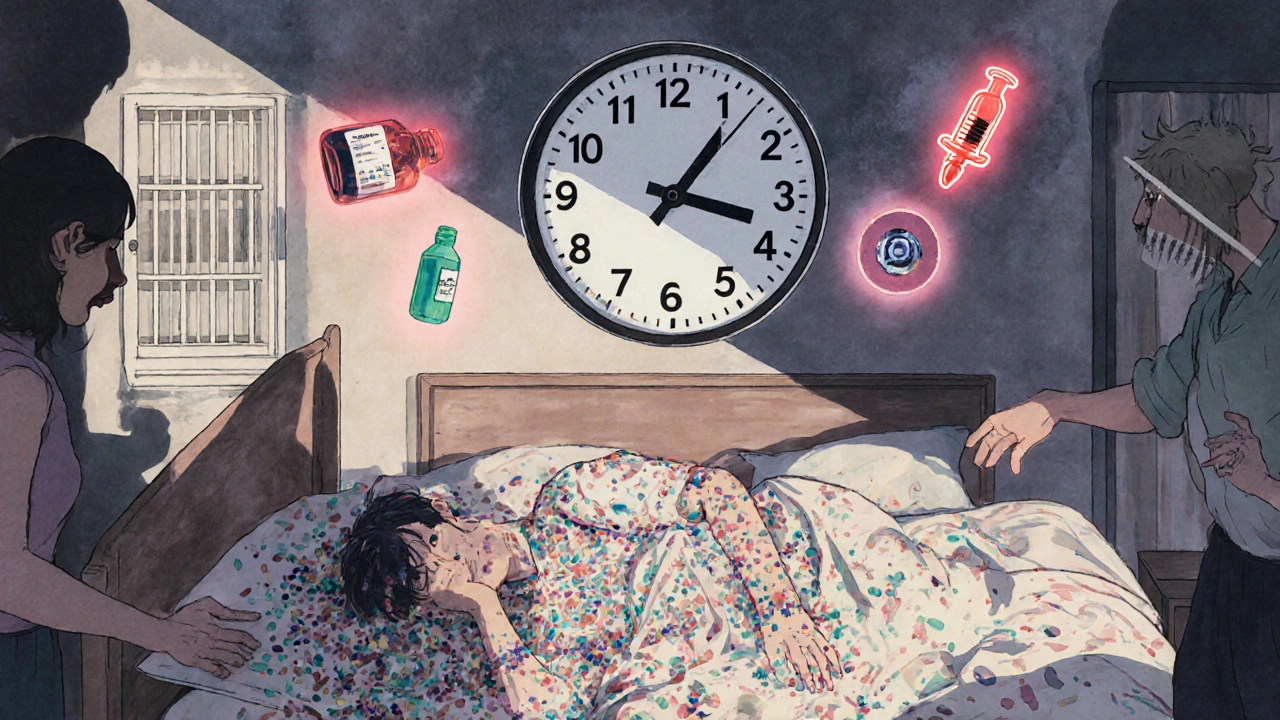
Restarting a medication after taking a break can be deadly-even if you’ve taken it safely before. This isn’t just a theoretical risk. People who stop opioids, benzodiazepines, or other central nervous system depressants for even a few days often return to their old dose and overdose because their body no longer tolerates it. The same dose that once felt normal can now shut down breathing. It’s not about being careless. It’s about biology changing without you realizing it.
This isn’t rare. The Washington State Department of Health found that 62% of fatal opioid overdoses happen within 72 hours after someone leaves jail, rehab, or the hospital-places where they were likely stopped from using. The same thing happens with benzodiazepines like Xanax or sleep meds like zolpidem. Even antidepressants like paroxetine or venlafaxine can cause dangerous reactions if restarted too soon after stopping, especially if you’ve taken other medications in between.
There’s no safe way to guess what your body can handle. You can’t rely on memory. You can’t trust how you felt last time. The only safe path is to start lower than you think you need.
For methadone, Washington State guidelines say you must wait 7 to 10 days after stopping before restarting-even then, start at 25% of your old dose. For short-acting opioids like heroin or oxycodone, 3 to 5 days of abstinence is enough to lose tolerance. Don’t assume you’re safe just because you feel fine. That’s when you’re most at risk.
Keep it with you. Give one to someone you trust-a family member, friend, or roommate. Teach them how to use it. In the U.S., Medicare and most private insurers now cover naloxone at no cost. If you’re in the UK, you can get it free from pharmacies or needle exchange programs.
Don’t wait until it’s too late. The CDC reports that 87% of people who survive an opioid overdose after restarting medication did so because someone nearby had naloxone and used it. That’s not luck. That’s preparation.
One case from the UK involved a man who stopped oxycodone for 10 days after a hospital stay. He returned to his old dose of 30mg and collapsed within an hour. He survived because his daughter had naloxone. He now takes 8mg daily-less than a third of his old dose-and feels better.
For example, if you were on a benzodiazepine for anxiety and stopped for a month, you might find that therapy or mindfulness practices work just as well. If you were on an opioid for chronic pain, your doctor might suggest physical therapy or non-opioid pain relievers instead.
The American Society of Addiction Medicine released new guidelines in February 2024 that include a 10-point scoring system to help doctors decide if restarting is safe based on how long you’ve been off the drug, your past dose, and other health conditions. Don’t skip this step. Your life depends on it.
There’s no shame in asking for help. People who restart safely don’t do it alone. They reach out. They follow protocols. They use naloxone. They listen to experts.
Medication restart after a break isn’t about willpower. It’s about science. It’s about respecting how your body changes. And it’s about having the tools to survive if something goes wrong.
If you’re thinking about restarting a medication after a break, talk to your doctor today. Don’t wait. Don’t guess. Don’t risk it. Your life is worth more than the old dose.
No. Feeling fine doesn’t mean your body can handle the old dose. Tolerance drops quickly, often without symptoms. Restarting without medical guidance puts you at high risk of overdose-even if you’ve taken the same dose for years.
Tolerance to short-acting opioids like heroin or oxycodone can drop in as little as 3 to 5 days. For long-acting opioids like methadone, it takes 7 to 10 days. But even after a single day off, your risk increases. Never assume you’re safe just because you’ve been off for a few days.
No. Naloxone is for anyone restarting prescription opioids, even if they were prescribed legally. Many overdoses happen to people on long-term pain medication after a hospital stay or break in treatment. It’s a medical safety tool-not a sign of drug use.
Yes, but not at your old dose. For most SSRIs and SNRIs, restart at 25% of your previous dose and increase slowly over weeks. If you stopped an MAOI, you must wait at least 14 days before starting any other antidepressant to avoid serotonin syndrome.
Contact a local pharmacy, harm reduction center, or community health clinic. Many offer free consultations and naloxone distribution. In the UK, you can get naloxone for free from needle exchange programs or pharmacies. In the U.S., most pharmacies dispense it without a prescription. Never restart without a plan-even if you’re on your own.
Yes. Extended-release naltrexone, given before restarting opioids, reduces overdose risk by 73% in the first 30 days. Wearable monitors that detect breathing changes and auto-administer naloxone are in clinical trials. Pharmacogenetic tests that analyze how your body metabolizes drugs are also becoming available to personalize restart doses.
If you’re restarting a medication after a break, your best protection isn’t willpower-it’s knowledge, preparation, and support. Start low. Go slow. Have naloxone. Talk to a professional. Your life depends on it.
lol u think i'm gonna start at 25%? i've been takin 40mg methadone for 5 yrs. i skip a week n come back? i got this. 😏
this is so important. i saw my brother almost die after he got outta rehab and went straight back to his old dose. he didn't even know his body changed. pls everyone read this. 🙏
i'm curious-how do we know the exact timeline for tolerance loss in different people? is it based on studies or just averages?
The data cited here is statistically significant and clinically validated. Misinformation about tolerance decay is responsible for countless preventable deaths. This post is not an opinion-it's a medical imperative.
It is of paramount importance to recognize that the physiological adaptations induced by chronic pharmacological exposure are not merely behavioral or psychological in nature; they are neurochemical, metabolic, and receptor-level phenomena that evolve dynamically over time. The notion that one can 'feel fine' and therefore assume safety is not only erroneous-it is potentially lethal. Medical supervision is not a suggestion; it is a non-negotiable safeguard.
so like... what if you're just some broke person who can't afford a doctor? you just gonna die? this whole thing feels like a rich person's checklist. 🤡
This is one of the most responsible, well-researched posts I've seen on this topic. The emphasis on naloxone access, low-dose restarts, and medical guidance is exactly what public health needs. Thank you for writing this.
i used to think restarting meds was about willpower... turns out it's about biology being smarter than my ego. i started at 10mg after 2 weeks off... felt like a ghost. but i'm alive. and that's better than being strong and dead. 🌱
fentanyl overdose after restart? yeah that’s real. lost my cousin last year. just 5mg. he thought he was fine.
if you're restarting opioids and don't have naloxone, you're playing russian roulette with your lungs. it's free at most pharmacies. go get it. now. 🙌
i did the 25% thing after 3 weeks off. turned out i only needed half of what i thought. felt better than ever. no more crushing doses. peace.
People who restart without medical supervision are selfish. They risk not just their lives, but the lives of everyone around them. This isn't a personal choice-it's a public health failure.
in SA we dont even have naloxone easy. people die on sidewalks. no one cares. this post is usa privileged. #realworld
i read this after my mom restarted her benzo and almost passed out. i had naloxone (she was on oxycodone too). called 911. she’s okay now. thanks for this.
as a veteran who's been on pain meds for 12 years, i can tell you-this isn't just advice. it's survival. my unit lost three guys after they got outta the VA. they didn't know their bodies forgot. now i carry naloxone in my truck. always.