When you or your child gets sick with a fever, sore throat, or cough, the biggest question isn’t just "How do I feel?" It’s "Is this bacterial or viral?" Because the answer changes everything - especially whether you need antibiotics or not. And here’s the hard truth: bacterial infection and viral infection are not just different in name. They’re completely different in how they work, how they’re treated, and what happens if you mix up the two.
What’s Really Going On Inside Your Body?
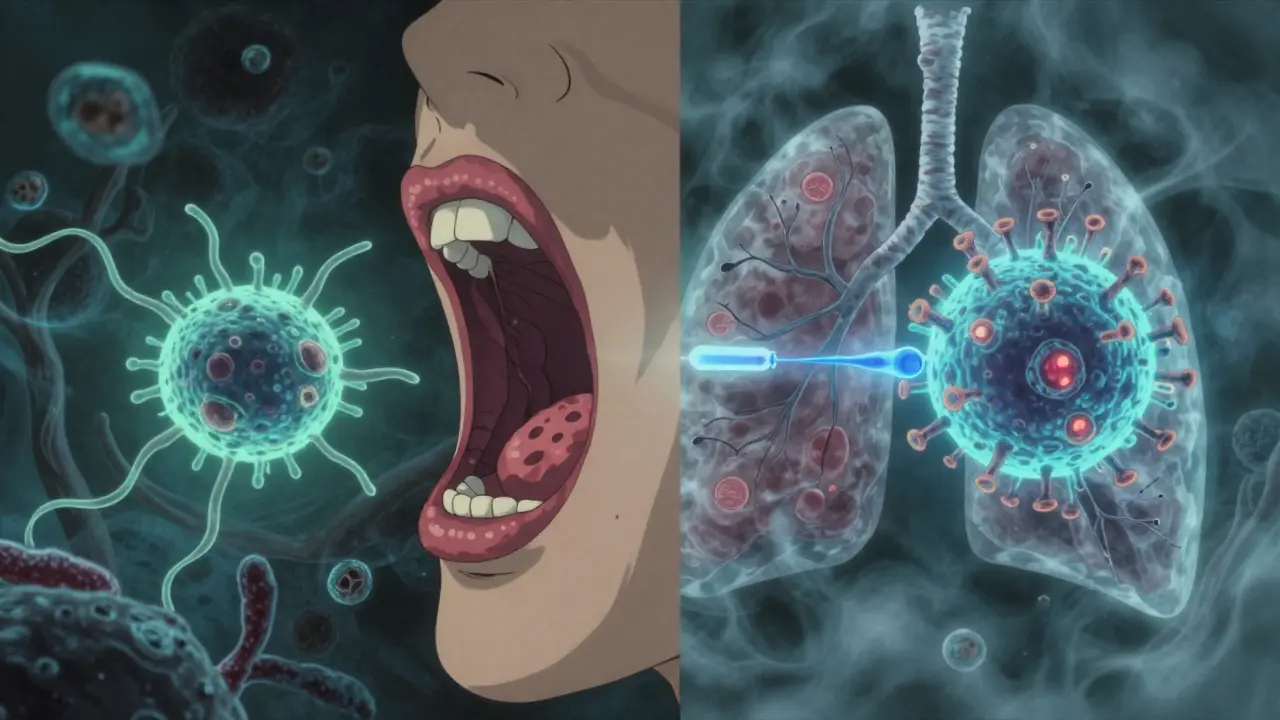
Bacteria are tiny, single-celled organisms. They’re alive, they eat, they reproduce, and they can survive on their own - on doorknobs, in water, even on your skin. Some are harmless. Some cause disease. When they do, they often trigger strong, localized infections like strep throat, urinary tract infections, or pneumonia caused by Streptococcus pneumoniae.
Viruses are not alive in the way bacteria are. They’re just genetic material wrapped in protein. They can’t survive or multiply on their own. They need to break into your cells and hijack their machinery to copy themselves. That’s why viruses cause things like the common cold, flu, chickenpox, or COVID-19. They don’t just infect you - they turn your own cells into virus factories.
This difference in structure is why antibiotics work on bacteria but do absolutely nothing to viruses. Antibiotics attack cell walls, protein production, or DNA replication - things viruses don’t have. Giving an antibiotic for a viral infection is like using a wrench to fix a broken lightbulb. It’s the wrong tool, and it can cause real harm.
Can You Tell Them Apart Just by Symptoms?
It’s tempting to think you can guess based on how you feel. But symptoms overlap way too much. Both can cause fever, fatigue, sore throat, cough, and body aches. Still, there are patterns that doctors use to guide their judgment.
Bacterial infections often come with:
- Fever higher than 101°F (38.3°C)
- Symptoms that get worse after a few days instead of better
- Localized pain - like one-sided ear pain, pus on tonsils, or thick yellow-green nasal discharge that lasts more than 10 days
Viral infections usually look like:
- Lower fever, often under 100.4°F (38°C)
- Runny nose, sneezing, hoarse voice
- Generalized aches and tiredness
- Symptoms peak around day 3-5 and start improving by day 7
But here’s the catch: a viral infection can open the door for a bacterial one. That’s why many people with the flu end up with bacterial pneumonia. About half of hospitalized COVID-19 patients develop a secondary bacterial infection. That’s not because the virus turned bacterial - it’s because the virus weakened the lungs, letting bacteria move in.
How Do Doctors Know for Sure?
Most people assume a doctor can tell just by listening to your throat or asking a few questions. But in reality, symptoms alone are wrong about 30% of the time - especially for sore throats. That’s why testing matters.
For strep throat, a rapid antigen test gives results in 10 minutes and catches 95% of cases. If it’s negative but the doctor still suspects strep, a throat culture (which takes 24-48 hours) is the gold standard, with 98% accuracy.
For viruses, PCR tests are the most reliable. For flu, they’re 90-95% accurate if done within the first 72 hours of symptoms. And now there’s something new: the FDA-approved FebriDx test, which checks two biomarkers - CRP (a sign of inflammation) and MxA (a protein your body makes only when fighting a virus). It can tell bacterial from viral in 10 minutes with 94% accuracy. That’s a game-changer for busy clinics.

What Happens When You Take Antibiotics for a Virus?
This is where things get dangerous. About 47 million unnecessary antibiotic prescriptions are written every year in the U.S. alone - most for colds, coughs, and sore throats that are viral. And each one carries a cost.
Antibiotics don’t just kill bad bacteria. They wipe out the good ones in your gut, skin, and mouth. That can lead to diarrhea, yeast infections, or worse - a deadly gut infection called Clostridioides difficile, which causes over 220,000 cases and 12,800 deaths in the U.S. every year.
Worse, every time you take an antibiotic when you don’t need it, you help create superbugs. Antibiotic-resistant bacteria are already killing 1.27 million people globally each year. By 2050, that number could hit 10 million - more than cancer.
The CDC says antibiotics should never be used for viral upper respiratory infections. Yet patients who get them anyway are 65% more likely to come back with the same symptoms next time - because they’ve learned that antibiotics = relief. That’s a dangerous expectation.
So What’s the Right Treatment?
If it’s bacterial:
- Antibiotics are the answer - but only the right one. Penicillin for strep throat, amoxicillin for ear infections, ciprofloxacin for UTIs.
- Finish the full course, even if you feel better in two days. Stopping early lets the toughest bacteria survive and multiply.
- Treatment usually lasts 5-14 days, depending on the infection.
If it’s viral:
- There’s no magic pill. Rest, fluids, and over-the-counter meds for fever and pain are your best friends.
- For flu, oseltamivir (Tamiflu) can shorten illness by 1-2 days - but only if taken within 48 hours of symptoms starting.
- For shingles (caused by chickenpox virus), acyclovir helps if started early.
- For severe COVID-19, remdesivir can reduce hospital stays, but it’s only used in hospitals.
Most viral infections - colds, bronchitis, sinus infections - get better on their own. The body’s immune system is the real hero here.
Why This Matters More Than You Think
The economic cost of viral respiratory infections in the U.S. is $45 billion a year - from missed work, school, and doctor visits. Bacterial infections cost billions more, especially when they become resistant.
Children average 6-8 viral upper respiratory infections a year. That’s 22 million missed school days and 20 million lost workdays for parents annually. Most of these don’t need antibiotics. But parents still ask for them - because they’re scared, tired, or just want their kid to feel better faster.
And here’s the reality: you can’t rush a virus. No amount of antibiotics will make a cold go away in 24 hours. But you can support your body with sleep, hydration, and time.
What’s Coming Next?
Science is catching up. Researchers are testing phage therapy - using viruses that only kill bacteria - to treat resistant infections. Early trials in Europe show 85% success rates. New narrow-spectrum antibiotics are being designed to target just one type of bacteria, sparing your good microbes.
The WHO’s 2023 report shows antibiotic resistance has jumped from 5.8% in 2017 to 17.3% in 2023. That’s not a slow creep - it’s a sprint. And without global action, we’re heading toward a future where simple infections become deadly again.
Meanwhile, universal coronavirus vaccines are in Phase III trials. If they work, they could prevent the next pandemic before it starts.
What Should You Do When You’re Sick?
Don’t panic. Don’t demand antibiotics. Do this instead:
- Monitor your symptoms. Are you getting better after 5-7 days? Likely viral.
- If you’re worse after day 5, or have a high fever, pus, or one-sided pain - see a doctor.
- Ask: "Could this be bacterial? Do we need a test?"
- If you’re given antibiotics, take them exactly as directed - no skipping doses.
- If you’re told it’s viral, trust that. Rest. Hydrate. Let your body heal.
Your body is smarter than you think. It’s been fighting off invaders for millions of years. You don’t always need a pill to help it win.
Can you have both a bacterial and viral infection at the same time?
Yes. A viral infection like the flu can weaken your immune system and make it easier for bacteria to invade. This is why many people with severe flu develop bacterial pneumonia. Doctors treat both - antivirals for the virus and antibiotics for the secondary bacterial infection. It’s not common, but it happens often enough in hospitals to be a major concern.
Why do some doctors still prescribe antibiotics for colds?
Sometimes it’s pressure. Patients ask for them. Sometimes it’s convenience - a quick script feels easier than explaining why it won’t help. Other times, doctors aren’t sure and prescribe "just in case." But guidelines are clear: antibiotics shouldn’t be used for viral upper respiratory infections. The rise of rapid tests like FebriDx is helping reduce this practice, but old habits die hard.
Is green mucus a sign of a bacterial infection?
Not necessarily. Green or yellow mucus can happen with both viral and bacterial infections. It’s your immune system sending white blood cells to fight the invader - whether it’s a virus or bacteria. The color alone doesn’t mean you need antibiotics. What matters more is how long symptoms last and whether they’re getting worse after day 5-7.
Can you prevent bacterial or viral infections?
You can reduce your risk. Wash your hands regularly. Get vaccinated - flu shots, pneumococcal vaccines, and soon, universal coronavirus vaccines. Avoid close contact with sick people. Don’t share utensils or towels. For bacterial infections like strep, early treatment stops spread. For viruses, vaccines are your best defense. Prevention beats treatment every time.
What if I took antibiotics for a virus - will I be okay?
One time? Probably. But each unnecessary use increases your risk of side effects and contributes to antibiotic resistance. If you’ve done it before, don’t panic. But next time, ask your doctor: "Is this definitely bacterial?" and "Is there a test we can do?" Your future self - and everyone around you - will thank you.