Every time you pick up a prescription, there’s a small sticker on the bottle that could save your life-or hurt you if you ignore it. These aren’t just random pieces of paper. They’re legally required safety alerts, designed to stop dangerous mistakes before they happen. But here’s the problem: most people don’t understand them.
The most serious warning is the black box warning. It’s called that because it’s printed in a bold, black rectangle at the top of the prescribing info. About 40% of new drugs approved between 2013 and 2017 carried one. These aren’t warnings about mild side effects. They’re for risks that can kill you-like heart failure, suicidal thoughts, or severe allergic reactions. If your medication has this, it doesn’t mean don’t take it. It means: know the signs, call your doctor right away if something feels wrong.
But here’s the catch: not all pharmacies use the same colors. Some use red for everything. Others don’t use color at all. That’s why you can’t rely on color alone. Always read the words.
Same goes for “take on an empty stomach.” That means at least one hour before eating, or two hours after. If you take it with coffee, toast, or even a vitamin, it won’t work right. And yes, grapefruit juice counts as food here. It interferes with over 85 medications, including statins and blood pressure pills. One patient told a forum they ended up in the ER after ignoring that warning.
And don’t assume the pill shape means it’s safe to split. Some tablets are coated to protect your stomach or control release. Splitting them can ruin that. If you can’t swallow a pill, ask your pharmacist for a liquid version or a different form. Don’t guess.

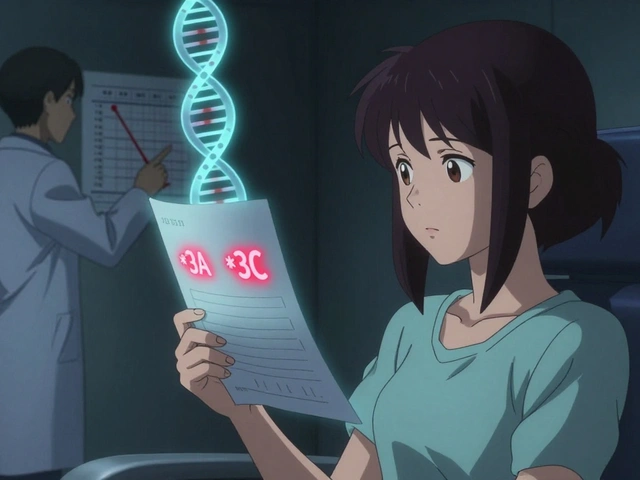
And here’s the kicker: the FDA admits most of these sheets are written at a college reading level. But 80 million American adults have trouble understanding basic health info. That’s why some pharmacies now use simplified labels. Kaiser Permanente tested a version with pictures, short sentences, and clear icons. Patient understanding jumped from 55% to 89%. The FDA is rolling out similar “Facts Labels” for 20 high-risk drugs by 2025.
One study found that using teach-back improved warning comprehension by 47%. That’s not magic. That’s just asking for clarity.
Meanwhile, patients keep getting hurt. A 2022 survey found 64% of people had ignored at least one warning. Most common? “Take with food” and “avoid sunlight.” One man took a skin cream that said “avoid sunlight” and ended up with second-degree burns. He thought it meant “don’t go to the beach.”
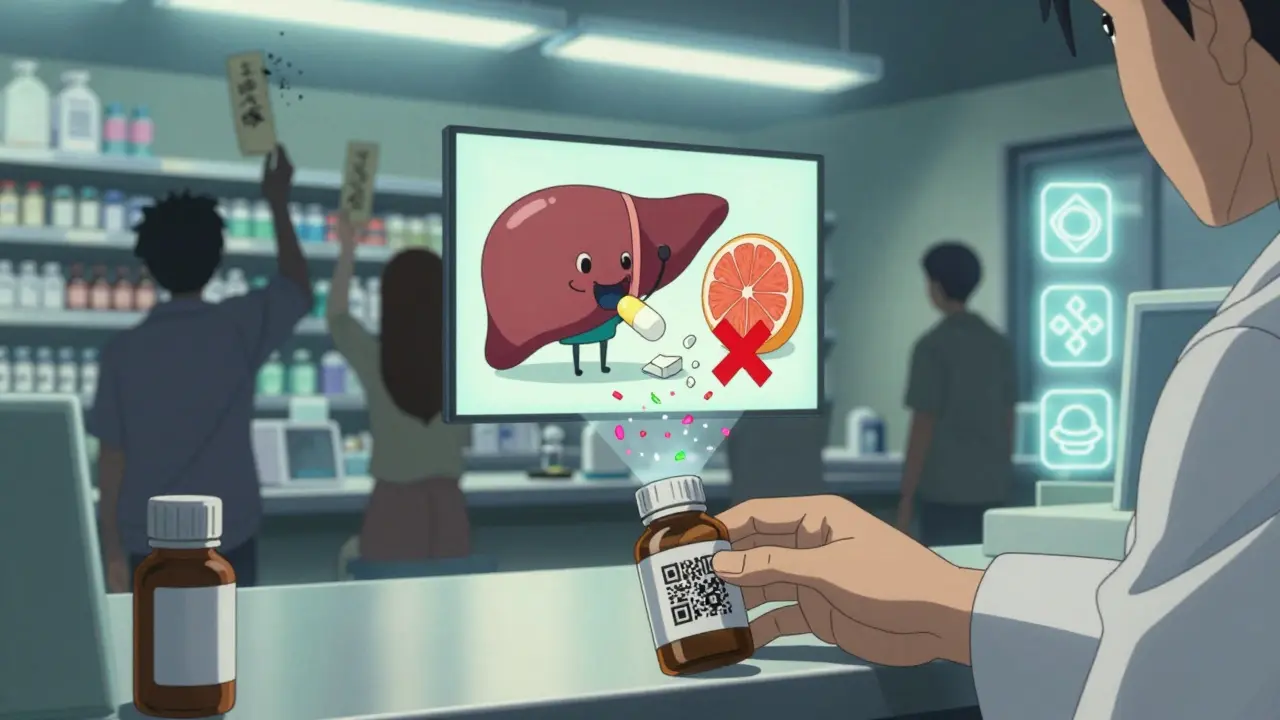
Some pharmacies are testing QR codes on labels. Scan it, and a 60-second video explains the warning in plain language. Mayo Clinic trials showed comprehension jumped 52%. By 2026, most major chains are expected to adopt these new standards.
It’s not perfect yet. But the direction is clear: labels are finally being rewritten for the people who actually take the medicine.
Medication errors cause 1.3 million injuries every year in the U.S. Most of them are preventable. The sticker on your bottle isn’t there to scare you. It’s there to help you stay safe. But only if you read it.
A black box warning is the strongest safety alert the FDA requires. It’s placed at the top of the prescribing information and signals that the medication carries a serious, potentially life-threatening risk-like heart failure, severe allergic reactions, or increased risk of suicide. It doesn’t mean you can’t take the drug, but it means you need to be closely monitored and know the warning signs.
It depends on how the drug is absorbed. Some medicines need food to help your body absorb them properly. Others can irritate your stomach or not work at all if taken with food. "Take with food" means eat a normal meal within 30 minutes before or after taking the pill. "Take on an empty stomach" means no food for at least one hour before and two hours after. Coffee, juice, or snacks count as food here.
No. Just because you didn’t have a reaction before doesn’t mean it’s safe. Your body changes. You might be taking a new drug that interacts with it. Or your liver or kidneys aren’t working the same. Warnings are based on the drug’s chemistry, not your past experience. Ignoring them is like driving without a seatbelt because you’ve never been in a crash.
Call your pharmacist or doctor right away. Don’t wait for symptoms. If it’s a time-release or extended-release pill, crushing it can release the full dose at once-this can be dangerous or even deadly. For example, crushing opioids can cause overdose. Your pharmacist can tell you if you need to skip a dose, adjust, or get a replacement.
No. While many pharmacies use red for danger and yellow for caution, there’s no nationwide standard. Some use only black text. Others don’t use color at all. Never rely on color alone. Always read the words. If you’re unsure, ask the pharmacist to explain what each sticker means.
That usually means your prescription was filled by a different pharmacy or a different batch of medication came from a different manufacturer. Even generic drugs can have different warning labels depending on the company that made them. Always compare the new label to the old one. If anything’s different, ask your pharmacist why.
So let me get this straight-the FDA says these labels are for our safety, but Big Pharma spent $200M lobbying to keep them unreadable? 🤔 I’ve been taking my blood pressure med for 5 years and never read the insert… until I started noticing my dreams were full of screaming pills. Now I’m convinced the stickers are mind-control nanobots disguised as warnings. They don’t want us to know the truth: the ‘black box’ is actually a portal to the pharmaceutical multiverse. I’ve seen the leaked documents. They’re not warnings-they’re *contracts*. You sign them by swallowing the pill. I’m not paranoid. I’m just… informed. 😈💊
Oh, PLEASE. Another feel-good article pretending the system cares about patients. The FDA? Ha! They’re just the PR arm of the pharmaceutical industry. You think they’d actually make labels easier to read? That’d be like asking a fox to redesign the chicken coop. And don’t even get me started on QR codes-next thing you know, they’ll be scanning your iris to confirm you’ve ‘consented’ to the side effects. And ‘take with food’? That’s code for ‘this drug is so toxic, even your stomach needs a bodyguard.’ I keep my inserts in a locked vault. One day, they’ll come for them. And when they do… I’ll be ready. 🚨📚
Interesting piece-though I’m surprised you didn’t mention that the FDA’s own internal memos admit that 72% of patients can’t parse even basic medical terminology. 🤦♂️ But let’s be honest: the real failure isn’t the labels-it’s the assumption that patients should be expected to decode legalese while dizzy from side effects. I’ve worked in pharmacy for 18 years. I’ve seen people cry because they didn’t know grapefruit juice could kill them. The ‘teach-back’ method? Brilliant. The fact that it’s not mandatory? Criminal. So yes, read the sticker. But also demand better. And if your pharmacist gives you a blank stare? Find a new one. 💉
Man, I’ve been there. Crushed a time-release Adderall once because I thought ‘swallow whole’ meant ‘don’t chew like a goat.’ Ended up vibrating for six hours. Didn’t die, but I did question my life choices. 🙃 Point is: we’re not dumb. We’re just tired. Tired of being treated like children who can’t read. The system’s broken, sure-but the fix isn’t more jargon. It’s empathy. Ask your pharmacist: ‘What’s the one thing I need to know that no one else told me?’ That’s the question that saves lives. And yeah, keep the insert. I keep mine in a shoebox labeled ‘Survival Manuals.’ It’s my little shrine to not dying. 💪
It is truly shameful that Western nations allow such chaotic and inconsistent labeling systems. In India, every medicine is labeled with clear, government-mandated Hindi and English instructions, accompanied by pictograms approved by the Ministry of Health. We do not rely on color-coded stickers that vary by pharmacy. We do not rely on QR codes that require smartphones. We rely on clarity, discipline, and respect for authority. This article reads like a cry for help from a society that has lost its way. The solution is not more technology-it is order. Structure. Responsibility. You cannot teach safety to those who refuse to obey. 🇮🇳
My grandma used to throw out her inserts like junk mail. Then she got hospitalized after mixing her blood thinner with a herbal tea she thought was ‘just a cleanse.’ She’s fine now, but she keeps every insert in a binder with tabs. Now she’s the one reminding me to read the labels. 😅 I used to think it was overkill… now I just copy her. I keep mine in a ziplock bag with my keys. Never forget: if it’s in your hand, it’s worth reading. Even if it’s boring. Especially if it’s boring. 💕
Look, I used to ignore all of this too. Until I took a steroid cream that said ‘avoid sunlight’ and ended up looking like a boiled lobster after a weekend at the beach. Turns out ‘avoid sunlight’ means ‘don’t go outside at all.’ Not ‘wear sunscreen.’ Not ‘stay under the umbrella.’ Just… don’t. 🤦♀️ I now read every label like it’s a Tinder bio-because if you skip the fine print, you’re gonna get ghosted by your own liver. And yeah, color codes are a mess. But if you’re not asking your pharmacist to explain it like you’re explaining it to your 12-year-old cousin? You’re doing it wrong. Chill. Read. Ask. Repeat.
Okay, real talk: I used to think the sticker was just a fancy decoration. Then I missed my own ‘take with food’ warning and threw up for 3 hours. 🤢 I didn’t know ‘with food’ meant ‘after a full meal’-I thought a granola bar counted. Spoiler: it doesn’t. Now I’ve got a sticky note on my fridge that says ‘READ THE STICKER.’ I even made a checklist: 1) Color? 2) Words? 3) Insert? 4) Ask? I’m not a genius. I just don’t wanna die. And if I can do it? So can you. You got this. 💪