This tool calculates the safe starting dose of azathioprine based on your TPMT and NUDT15 genetic testing results. Your doctor should always determine your final dosage.
Before you start azathioprine, your doctor should ask you one simple question: Have you been tested for TPMT? It’s not just a routine check-it could save your life.
Azathioprine has been used for over 60 years to treat Crohn’s disease, ulcerative colitis, lupus, and to prevent organ rejection after transplants. It works by calming down an overactive immune system. But for some people, this drug turns dangerous. Without proper screening, it can crash your bone marrow, leaving you with dangerously low white blood cells, red blood cells, and platelets. That’s called myelosuppression-and it can lead to sepsis, bleeding, or even death.
Your body breaks down azathioprine using an enzyme called thiopurine methyltransferase, or TPMT. If your TPMT enzyme doesn’t work well-because of your genes-azathioprine builds up to toxic levels. You don’t feel it coming. No warning signs. Just a routine blood test weeks later shows your white blood cell count has dropped to zero.
About 1 in 300 people have two broken copies of the TPMT gene. These people are at extreme risk. Even a normal dose of azathioprine can kill their bone marrow. Another 1 in 10 people have one broken copy. Their bodies process the drug slowly. They need lower doses to stay safe.
That’s why testing isn’t optional-it’s standard. The Clinical Pharmacogenetics Implementation Consortium (CPIC), which includes top experts from St. Jude and Harvard, says you must test before starting azathioprine. The FDA updated the drug label in 2019 to say the same. But many doctors still skip it. Why? Because they think it’s expensive, slow, or unnecessary. That’s outdated thinking.
There are two ways to test: genotyping and phenotyping.
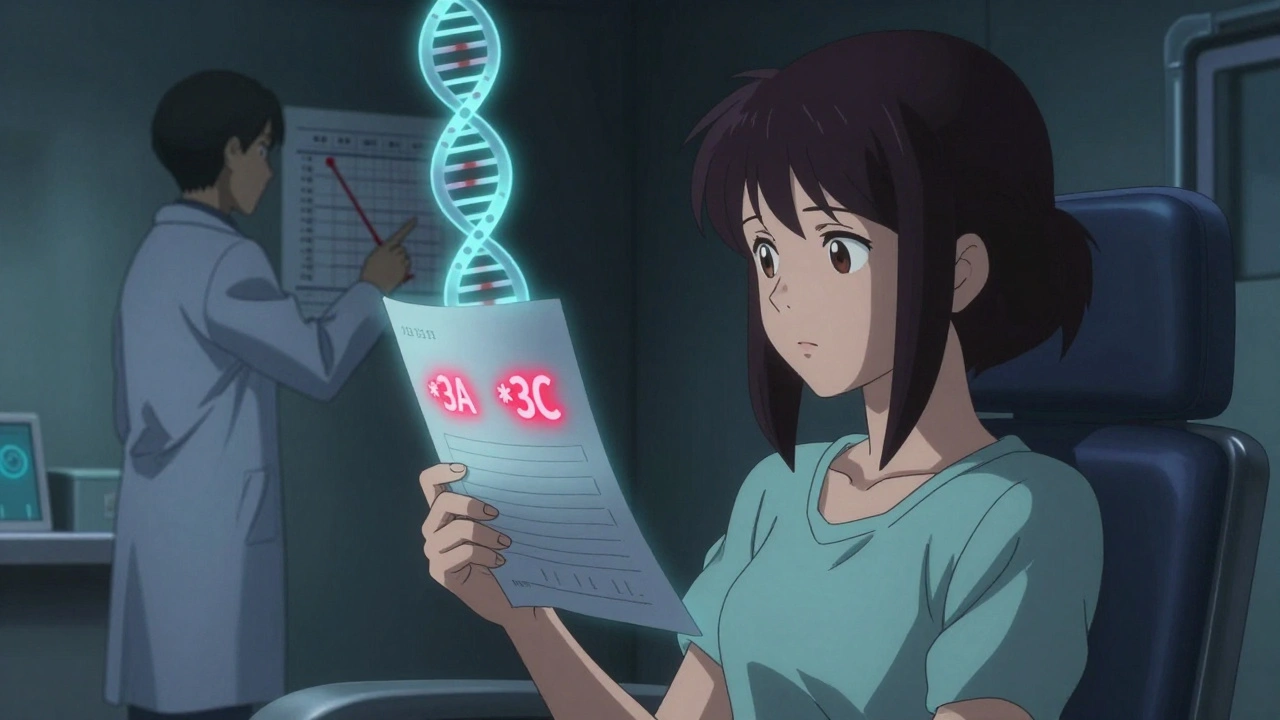
Genotyping looks at your DNA. It checks for specific gene variants like *2, *3A, *3B, and *3C. These are the common mutations that break TPMT. Results come back in 3 to 7 days. It’s accurate, even if you’ve had a blood transfusion recently.
Phenotyping measures enzyme activity in your red blood cells. It’s cheaper but unreliable if you’ve had a transfusion in the last 3 months. Your donor’s blood cells can mess up the results. That’s why genotyping is now the gold standard.
Cost? In the U.S., it runs $200-$400. Insurance usually covers it. In the UK, the NHS often provides it for free if you’re on the IBD pathway. The price is tiny compared to the cost of a hospital stay for sepsis or a blood transfusion.
Your result will fall into one of three categories:
One patient I spoke with-Sarah, 34, from Birmingham-had a routine TPMT test before starting azathioprine for ulcerative colitis. Her result showed intermediate activity. Her doctor cut her dose in half. Six months later, her white blood cell count was stable. Her friend, who skipped testing, had to stop the drug after three weeks because her ANC (absolute neutrophil count) dropped below 500. She ended up in the hospital with a fever and pneumonia.
For years, TPMT was the only gene we cared about. But in 2013, researchers found another player: NUDT15.
NUDT15 is another enzyme that breaks down azathioprine. People with NUDT15 variants are at high risk for severe myelosuppression-even if their TPMT is normal. This is especially true in people of Asian descent. Up to 20% of East Asian populations carry a risky NUDT15 variant. In white Europeans, it’s less than 5%.
That’s why CPIC updated its guidelines in 2022 to recommend testing for both TPMT and NUDT15 together. Many labs now offer a combined panel. If you’re of Asian, Hispanic, or Native American ancestry, this isn’t optional-it’s essential.
One study showed that in a group of Thai patients with IBD, 17% had NUDT15 deficiency. Without testing, they’d all have been given full doses. Nearly half developed severe neutropenia within 8 weeks.
Here’s the hard truth: TPMT testing doesn’t stop every side effect.
Some people get liver damage. Others get pancreatitis. Some develop nausea, rashes, or sun sensitivity. A 2000 JAMA Dermatology study found that only 1 out of 13 patients who had to stop azathioprine had low TPMT activity. The rest had normal genes but still got sick.
Drug interactions are a big culprit. Allopurinol-used for gout-blocks the same enzyme that breaks down azathioprine. Even if your TPMT is perfect, taking both drugs can cause life-threatening toxicity. The same goes for ACE inhibitors and some antibiotics.
That’s why your doctor still needs to check your blood every week for the first month, then monthly after that. CBC (complete blood count) and liver enzymes are non-negotiable. TPMT testing doesn’t replace monitoring. It just makes it smarter.
Azathioprine costs $20-$50 a month. Biologics like infliximab cost $1,500-$2,500 per infusion. So it’s tempting to skip testing and save money upfront.
But here’s the math: One hospitalization for sepsis from myelosuppression can cost over $50,000. Add in lost work, missed appointments, and long-term damage to your bone marrow, and the savings vanish.
A 2011 trial with 333 patients found that TPMT testing didn’t reduce overall side effects. But it did prevent every single case of life-threatening neutropenia in the homozygous-deficient group. That’s one life saved per 300 people tested. That’s worth it.
Insurance companies in the U.S. cover it. The NHS in the UK covers it. The European Crohn’s and Colitis Organisation (ECCO) says it’s recommended. Only in under-resourced clinics is it skipped.

If you’re about to start azathioprine:
If you’ve already been on azathioprine for months without testing, don’t panic. But get tested now. It’s not too late. Your doctor can still adjust your dose based on your results.
If your test shows you’re homozygous deficient, or you’ve had bad reactions before, here are safer options:
None of these are perfect. But they’re safer if your body can’t handle azathioprine.
Azathioprine is cheap. It’s effective. It’s been around for decades. But it’s not a one-size-fits-all drug. Your genes matter. Your ancestry matters. Your other medications matter.
TPMT and NUDT15 testing aren’t fancy science-they’re basic safety. Just like checking your blood pressure before giving you a drug that raises it. Or testing for allergies before giving you penicillin.
If your doctor hasn’t mentioned testing, ask. If they say it’s not needed, ask why. And if they still say no, get a second opinion. Your life isn’t worth the risk of skipping it.
Yes. You may have been lucky so far, but your risk hasn’t changed. Some people develop myelosuppression after months or even years of use. Testing now helps your doctor assess your current risk and decide whether to keep you on the drug, reduce your dose, or switch to something safer.
Don’t assume you inherited it. You could have normal TPMT even if a parent had a variant. Only a genetic test can tell you your status. Never rely on family history alone. Get tested before starting the drug.
That’s common. TPMT only explains part of the risk. Other genes, drug interactions, or liver problems can cause toxicity. Your doctor should still monitor your blood counts and liver enzymes regularly. Nausea, rash, or joint pain don’t always mean you need to stop-just adjust the dose or add supportive care.
Yes. In the UK, the NHS typically covers TPMT and NUDT15 testing for patients prescribed azathioprine for inflammatory bowel disease or autoimmune conditions. It’s part of standard care in most gastroenterology clinics. If your hospital doesn’t offer it, ask your specialist to refer you to an IBD center.
Yes. Some patients with autoimmune conditions or a family history of IBD choose to get tested preemptively. It’s not routine, but it’s allowed. If you’re considering azathioprine as a future option, ask your doctor about ordering the test now. Results are valid for life.
No. They test for different genes. Some people have normal NUDT15 but low TPMT. Others have the reverse. The safest approach is to test for both at the same time, especially if you’re of Asian descent. Many labs now offer a combined panel.
You could develop severe neutropenia, which increases your risk of life-threatening infections. You may need hospitalization, antibiotics, growth factors to boost your blood cells, or even a blood transfusion. In rare cases, it leads to permanent bone marrow damage. Testing prevents all of that.
This is why you don't skip labs. One blood test before starting azathioprine can prevent a trip to the ICU. Simple. No drama. Just do it.
In India, we still see doctors prescribe this like it's aspirin. My cousin got admitted with sepsis because his TPMT wasn't checked. He's fine now but lost three months of work. This isn't fancy science-it's basic.
The systemic neglect of pharmacogenomics in primary care is a moral failure. We have the tools to prevent iatrogenic death, yet inertia, cost-myopia, and institutional complacency persist. The TPMT/NUDT15 paradigm isn't an innovation-it's an ethical imperative. Failure to implement constitutes negligence under the principle of non-maleficence. We are not merely treating patients-we are stewards of biological integrity.
I got tested before starting azathioprine for my crohn’s. Turned out i was heterozygous. Doc cut my dose in half and i’ve been good for 2 years now. Seriously though, if your doc hasn’t mentioned this, just ask. It’s not weird. It’s smart.
I had a friend who skipped the test because she thought it was "overkill." She ended up in the hospital with a fever and zero neutrophils. Her mom cried in the ER. Please don’t be that person. Get tested. It’s not expensive. It’s not hard. It’s just... necessary.
So let me get this straight. We have a $20 drug that can kill you if you don’t pay $300 for a test first. And the system still lets doctors skip it? Welcome to American healthcare. Where saving lives is optional if it doesn’t involve a co-pay.
The CPIC guidelines are unequivocal. The FDA labeling is unequivocal. The pharmacokinetic data is unequivocal. Yet we persist in a pre-genomic paradigm of empiric dosing. This is not merely suboptimal-it is epistemologically regressive. The conflation of cost-efficiency with clinical safety represents a profound failure of translational medicine.
They say it's about safety. But what if this is just Big Pharma pushing tests to make more money? What if the real reason is that they want you on expensive biologics instead? I've seen this before. Always a test. Always a new drug. Always more bills.
NUDT15? What next? We gonna test for aliens in your DNA too? I’ve been on azathioprine for 8 years. No problems. Why you wanna test me? Maybe its just my body strong. Not all white people got this problem.
I just want to say how deeply moved I am by the thoughtful, compassionate, and scientifically rigorous approach to patient safety that this post embodies. It is not merely a clinical guideline-it is a moral compass in an increasingly fragmented healthcare landscape. The integration of pharmacogenomic principles into routine practice reflects not only medical advancement but a profound commitment to human dignity, equity, and the sanctity of life itself. I encourage every clinician, every patient, and every policymaker to internalize this message-not as a recommendation, but as a sacred obligation. Thank you for this luminous contribution to the collective conscience of medicine.