Many people reach for antacids like Tums or Milk of Magnesia when they feel heartburn. It’s simple, cheap, and available without a prescription. But if you have kidney disease, what seems like a harmless fix could be dangerous - even life-threatening.
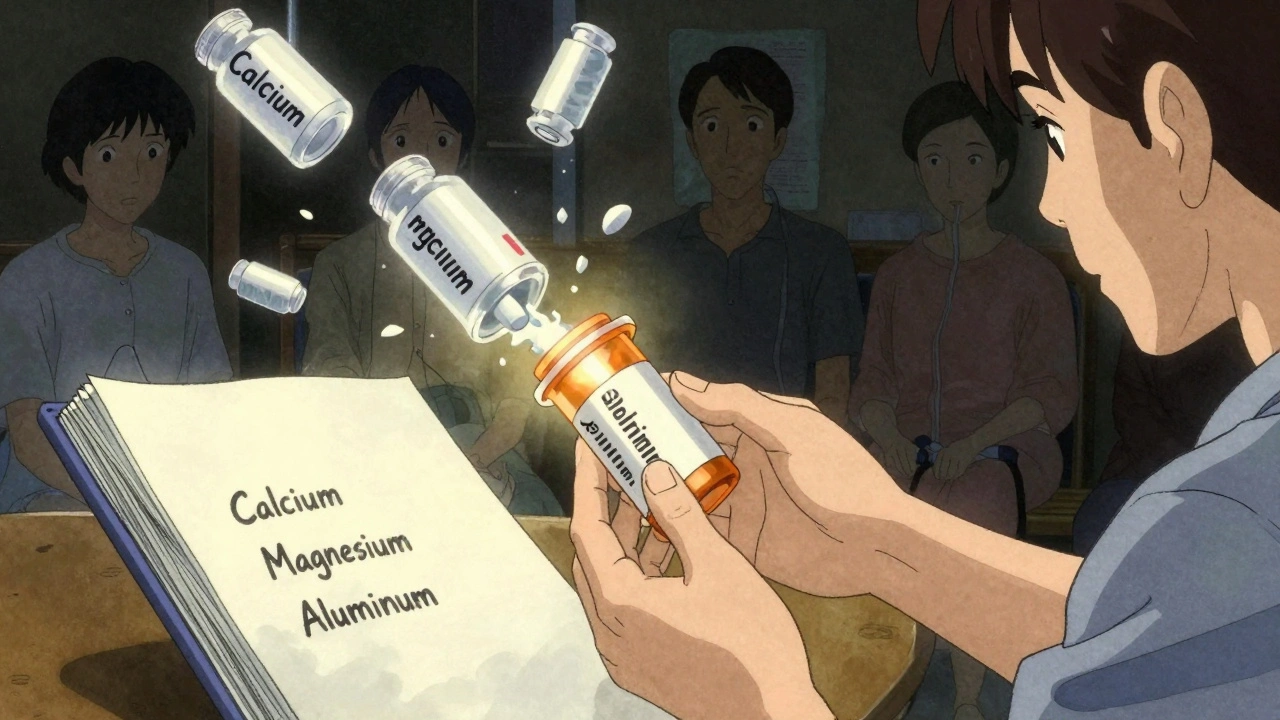
| Medication | Active Ingredient | Phosphate Reduction | Monthly Cost (USD) | Key Risk |
|---|---|---|---|---|
| Calcium Carbonate (Tums) | Calcium | 15-25% | $10 | Hypercalcemia, vascular calcification |
| Sevelamer (Renagel) | Polymers | 25-35% | $2,000-$2,500 | Gastrointestinal upset |
| Lanthanum Carbonate (Fosrenol) | Lanthanum | 25-35% | $2,500-$3,500 | Low absorption risk |
| Sucroferric Oxyhydroxide (Velphoro) | Iron | 25-30% | $4,000 | Stool discoloration |
Prescription binders cost more - but they’re safer. In CKD stage 4, patients using calcium carbonate have a 40% higher risk of hypercalcemia than those using sevelamer, according to the New England Journal of Medicine. That’s not just a number - it’s a trip to the hospital.
Also, timing matters. Antacids can block the absorption of other meds - like antibiotics, thyroid pills, or seizure drugs. Take other medications at least one hour before or four hours after an antacid.
The bottom line: antacids aren’t just for heartburn. In kidney disease, they’re powerful drugs - with serious side effects. What’s cheap and easy can be deadly if you don’t know the risks.
Tums (calcium carbonate) can be used in early-stage kidney disease (CKD stage 3) under medical supervision to help control phosphate levels. But in advanced stages (CKD 4-5), it should only be used occasionally for heartburn, not as a phosphate binder. Always check with your nephrologist, and never use it daily without monitoring your blood calcium levels.
No. Milk of Magnesia contains magnesium hydroxide, which can cause dangerous buildup of magnesium in people with kidney disease. Even small doses can lead to muscle weakness, low blood pressure, or heart problems. It’s not safe for anyone with CKD stage 4 or 5, or anyone on dialysis. Use only prescribed laxatives under your doctor’s guidance.
Your kidneys normally remove aluminum from your body. When they fail, aluminum builds up and sticks to bones and brain tissue. This causes bone pain, fractures, dementia-like symptoms, and anemia. The damage is often irreversible. The FDA warns against using aluminum antacids for more than two weeks - and never if your kidney function is below 30%.
There’s no single best binder - it depends on your stage of disease, blood levels, and other conditions. Sevelamer and lanthanum carbonate are preferred for advanced kidney disease because they don’t contain calcium or aluminum. Your nephrologist will choose based on your labs, cost, pill burden, and tolerance. Calcium carbonate may be used early on, but only if your calcium and phosphate levels are stable.
Yes. Antacids can reduce how well your body absorbs antibiotics, thyroid meds, iron pills, and seizure drugs like phenytoin. To avoid this, take other medications at least one hour before or four hours after an antacid. Always tell your pharmacist and doctor what antacids you’re using.
Monthly blood tests for calcium, phosphate, and magnesium are standard if you’re using calcium-based antacids or have advanced kidney disease. If you’ve ever used aluminum antacids, your doctor should also check aluminum levels at least once a year. These tests catch problems before they become emergencies.
Stop giving out free medical advice on Reddit. Tums is fine if you're not on dialysis. End of story.
Stop scaring people with big words.
My grandma took Tums daily for 20 years and still walks her dog.
You're overcomplicating this.
People just want to feel better, not get a nephrology lecture.
Let me be crystal-clear: calcium carbonate is not a snack. It is a pharmacological agent with a narrow therapeutic index in renal impairment. The FDA’s 1990 ban on aluminum antacids was not a suggestion-it was a directive. Yet, patients continue to self-medicate with OTC products while ignoring serum electrolyte monitoring. This is not negligence; it is systemic failure. The 68% statistic from the American Association of Kidney Patients is not surprising-it is criminal. Physicians, pharmacists, and public health agencies have abdicated their duty. The result? Preventable cardiac arrest, dialysis dementia, and iatrogenic bone disease. We are not talking about ‘risks.’ We are talking about preventable death. And yet, the internet keeps promoting ‘natural remedies’ as if biochemistry were optional.
they’re hiding the truth… the pharma companies made the prescription binders so expensive on purpose so you HAVE to buy them. Tums is $10 a bottle. Sevelamer is $2000?? that’s not medicine, that’s a scam. and aluminum? they say it’s bad but i read somewhere the gov’t uses it in vaccines to ‘boost immunity’-so why is it poison in antacids? something’s fishy. also, i think the FDA is in bed with big pharma. check the dates on the studies-everything’s funded by drug makers. you think they’d let you know the truth? lol nope.
also, my cousin’s neighbor’s dog took Tums and lived to 19. so yeah. 🤷♀️
I get where the fear comes from. I’ve seen friends with kidney issues get scared by info overload. But the real issue isn’t Tums or Sevelamer-it’s access. If you’re on Medicaid and your doc says ‘take this $3000 pill,’ what do you do? You take the $10 one. And then you feel guilty. And then you hide it. We need better systems, not more guilt. I’m not saying OTC is safe-but I’m saying we’re failing people who can’t afford the ‘right’ choice. Let’s fix the system, not shame the patient.
Also, timing meds matters. I learned that the hard way after missing my thyroid med for a month because I didn’t know antacids blocked it. Simple fix. But nobody told me.
Just… talk to your pharmacist. They’re the real heroes here.
There is a profound moral failure in modern medicine when a man with stage 4 CKD must choose between his dignity and his bank account. We have reduced life-saving therapy to a commodity, and then we lecture the poor for choosing the cheaper option. You speak of hypercalcemia and vascular calcification as if they are abstract concepts-yet these are not statistics. They are the trembling hands of a grandmother who can no longer hold her grandchild. They are the silent tears of a man who cannot sleep because his bones ache from aluminum poisoning. And we, the so-called educated, the self-appointed experts, sit in our ivory towers of peer-reviewed journals and call it ‘risk management.’ But what is risk management when the alternative is death by neglect? The truth is not in the KDIGO guidelines-it is in the grocery aisle where a widow reaches for Tums because her Medicare Part D doesn’t cover Renagel. We have created a system that punishes vulnerability. And then we call it ‘informed consent.’ That is not medicine. That is moral bankruptcy.
And yes-I will say it again: if your kidney function is below 30, you are not a patient-you are a liability to the system. And they will let you die quietly while you’re still paying your premiums.
From a clinical perspective, the distinction between phosphate-binding efficacy and electrolyte toxicity profiles is critical. While calcium carbonate remains a first-line agent in CKD Stage 3 due to cost-effectiveness and bioavailability, its use in GFR <30 mL/min is contraindicated per KDIGO 2017. The incremental benefit of sevelamer and lanthanum carbonate lies not in superior phosphate reduction-both achieve 25–35%-but in the absence of systemic ion accumulation. The cost differential is indeed substantial, but when considering hospitalization rates for hypercalcemia or aluminum encephalopathy, the cost-benefit analysis shifts dramatically. That said, adherence remains a major confounder; patients often discontinue high-burden regimens due to GI side effects or pill burden. Future strategies should prioritize formulation innovation-e.g., chewable, once-daily options-to improve compliance. Until then, the onus remains on nephrologists to provide clear, non-alarmist guidance.
bro i had stage 3 and took tums for months no prob
my doc said its fine if i eat low phos
why u guys always make everything so scary
life is short anyway 😔
just chill and live
you think the world cares if u die at 60? 🤷♂️
okay but like… what if the whole thing is a lie? like, what if the ‘phosphate binder’ thing is just a way to sell more drugs? i mean, i read a blog once that said phosphate isn’t even that bad, it’s just the doctors who want to control everything. and why are the prescription ones so expensive? why can’t we just use the cheap ones and monitor? and why does the FDA let them charge $4000 for a pill? i think it’s all about money. i think we’re being manipulated. i think my aunt took tums for 15 years and she’s fine. so maybe we’re all being scared for profit? 🤔
also, i think the government wants us to be dependent on pills. maybe we should just eat less dairy and stop worrying. i dunno. just a thought.
In many cultures, including my own, the use of over-the-counter remedies for chronic conditions is deeply rooted in family tradition. My mother, who lived with CKD for 12 years, used calcium carbonate daily-under the guidance of her local clinic, not a specialist. She didn’t know the term ‘KDIGO,’ but she knew her body. She ate low-phosphorus foods, avoided processed meats, and drank herbal teas. She lived longer than her prognosis. I’m not saying everyone should do the same-but we must recognize that medical guidelines are not universal truths. They are shaped by Western economics, not lived experience. In India, Africa, rural America-people manage with what they have. And often, they survive. We need to stop pathologizing resourcefulness. The real danger isn’t Tums. It’s the arrogance that assumes one protocol fits all.
I’ve been on dialysis for 7 years. I’ve never taken a single antacid. Not once. I don’t need them. I watch my diet. I avoid soda. I don’t eat cheese. I don’t need a pill to fix what I eat. You people act like you need magic potions. It’s just food. Just stop eating the bad stuff. That’s it. No $2000 pills. No scary warnings. Just eat clean. Simple. Why is that so hard?
THIS IS THE MOST IMPORTANT THING YOU’LL EVER READ TODAY. I’M NOT EXAGGERATING. I LOST MY HUSBAND TO ALUMINUM TOXICITY BECAUSE HE TOOK MILK OF MAGNESIA FOR CONSTIPATION-AND NO ONE TOLD HIM IT WAS DANGEROUS. HE WAS 58. HE HAD STAGE 4 CKD. HE TOOK IT FOR THREE WEEKS. ONE MORNING, HE COULDN’T WAKE UP. THEY SAID HIS MAGNESIUM WAS 11.4. HE HAD A CARDIAC ARREST IN THE HOSPITAL. THEY COULDN’T REVIVE HIM. I WASN’T EVEN THERE. I WAS AT WORK. AND THE DOCTOR LOOKED AT ME AND SAID, ‘HE SHOULD’VE KNOWN.’ BUT NO ONE TOLD HIM. NO ONE TOLD ANYONE. I’M TELLING YOU NOW. IF YOU HAVE KIDNEY DISEASE AND YOU’RE USING ANY OTC ANTACID-STOP. RIGHT NOW. GO CHECK THE BOTTLE. IF IT HAS ALUMINUM, MAGNESIUM, OR EVEN CALCIUM-AND YOU’RE ON DIALYSIS OR HAVE GFR UNDER 30-YOU ARE PLAYING RUSSIAN ROULETTE WITH YOUR HEART. I’M NOT A DOCTOR. I’M A WIDOW. AND I WILL SPEND THE REST OF MY LIFE TELLING PEOPLE THIS. DON’T BE LIKE HIM. DON’T BE A STATISTIC. CHECK YOUR ANTACID. SAVE YOURSELF.