When your doctor orders liver function tests, it’s not because they think you have a serious problem-most of the time, it’s just a routine check. But if your results come back with numbers that look odd, it can feel confusing. What do ALT, AST, and bilirubin even mean? And why does one number being high matter more than another? The truth is, liver tests don’t measure how well your liver is working like a machine. They measure damage. And understanding that difference changes everything.
The term "liver function tests" is misleading. These aren’t tests of liver performance-they’re tests of liver injury. Think of them like smoke alarms. When your liver cells get damaged, they leak enzymes into your blood. Those enzymes show up on the test. The higher the number, the more damage has likely happened. But here’s the catch: a slightly elevated ALT or AST doesn’t always mean disease. About 10-15% of healthy people have numbers just above the normal range without any liver problems.
The main markers are ALT (alanine aminotransferase), AST (aspartate aminotransferase), ALP (alkaline phosphatase), GGT (gamma-glutamyl transferase), bilirubin, albumin, and prothrombin time. But not all of them are created equal. ALT and AST are the most talked about because they’re the first to spike when liver cells are hurt. ALT is mostly found in the liver, so when it’s high, it’s a strong signal that something’s wrong there. AST, on the other hand, is also in your heart and muscles. That means if you’ve had a bad workout or a heart attack, AST can rise too-even if your liver is fine.
Normal values aren’t the same for everyone. For ALT, the usual range is 7-55 U/L, and AST is 8-48 U/L. But those numbers shift based on your body. Men typically have higher levels than women. People with a BMI over 30 often have ALT and AST levels 10-15% higher than those with a normal weight. A 2022 study in JAMA Internal Medicine found that primary care doctors often overreact to ALT levels between 41-80 U/L, ordering scans or referrals when no real problem exists.
Bilirubin is different. Normal total bilirubin is between 3-17 μmol/L. This is the yellow pigment your liver processes from old red blood cells. If it builds up, you get jaundice-yellow skin or eyes. But even small increases can mean trouble. The key is whether it’s conjugated (direct) or unconjugated (indirect). Conjugated bilirubin rising usually means bile flow is blocked-think gallstones or liver disease. Unconjugated bilirubin rising might mean you’re breaking down too many red blood cells.
Doctors don’t look at one number in isolation. They look at the pattern. That’s where the real diagnosis begins.
If ALT and AST are both high-especially ALT more than AST-it’s usually a sign of hepatocellular injury. That means liver cells are dying. This happens in:
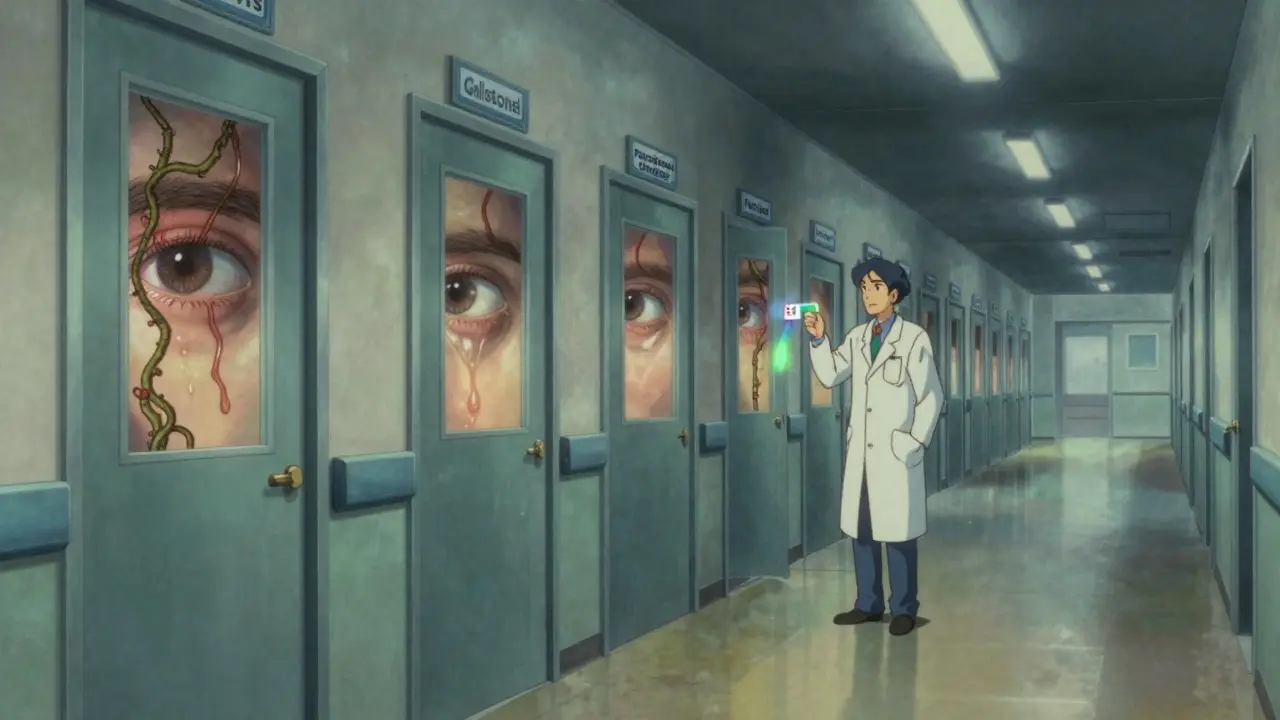
If ALP and bilirubin are high, but ALT and AST are only slightly up, that’s cholestatic injury. That means bile isn’t flowing right. This points to:
Here’s the trick: if ALP is high but GGT is normal, the problem might not be your liver at all. ALP is also made in bones. So if you have a broken bone or bone cancer, ALP can rise without liver damage.
The ratio of AST to ALT is one of the most powerful tools in interpreting liver tests. Most people don’t know this, but it can tell you whether alcohol is the culprit.
If AST is more than twice as high as ALT (a ratio over 2:1), there’s a 90% chance it’s alcohol-related liver disease. In alcoholic hepatitis, AST often hits 2-6 times the upper limit, while ALT only goes up 1-2 times. That’s because alcohol damages liver cells differently than viruses or fat.
But if ALT is higher than AST, that’s the classic pattern of MASLD (fatty liver disease linked to obesity or diabetes). It’s also common in viral hepatitis.
And if AST is above 500 U/L? That’s a red flag. Alcohol alone rarely causes that kind of spike. It’s more likely a drug overdose-especially paracetamol. In heavy drinkers, this could mean acute liver failure.
ALT and AST tell you about damage. But albumin and prothrombin time tell you if your liver is still working.
Albumin is a protein your liver makes. Normal levels are 35-50 g/L. If albumin drops slowly over months, it means your liver is struggling to make proteins-usually a sign of advanced cirrhosis. The half-life of albumin is 20 days, so it doesn’t change fast. A low albumin today means your liver has been weak for a while.
Prothrombin time (PT) measures how fast your blood clots. Your liver makes clotting factors. If PT is prolonged, your liver isn’t making those proteins anymore. This is a red flag for acute liver failure. PT changes quickly-within hours-so it’s a better sign of sudden, severe damage than albumin.
Here’s how this looks in real life:
Not every high number needs action. The American Association for the Study of Liver Diseases (AASLD) says if ALT or AST is only slightly elevated-under 2 times the upper limit-and you feel fine-you can wait. Monitor it in 3-6 months. Lifestyle changes like losing weight, cutting alcohol, or controlling diabetes can reverse early damage.
But if your ALT or AST is over 500 U/L, or if it’s rising fast-more than 100 U/L per week-you need to see a specialist right away. Same if you have jaundice, confusion, swelling in your belly, or bleeding gums. These are signs of serious liver failure.
And don’t forget: some things look like liver disease but aren’t. A hard workout can raise AST. Muscle injury can raise ALT. A recent infection can spike bilirubin. That’s why doctors always ask about your symptoms, meds, alcohol use, and recent illnesses.
A 2021 study of over 12,000 patients showed that using liver tests alone to spot advanced scarring (fibrosis) was only 68% accurate. But when doctors added a simple score called FIB-4-which uses age, platelets, ALT, and AST-the accuracy jumped to 89%. That’s why more clinics are using non-invasive scores now. They’re cheaper, safer, and more reliable than jumping straight to a liver biopsy.
Future tools are even better. The ELF test (Enhanced Liver Fibrosis) combines three blood markers to detect early scarring before it shows up on regular tests. In 2024, a Lancet study showed it was 92% accurate at spotting advanced fibrosis when combined with AST/ALT ratios.
So if your doctor says your liver enzymes are high, don’t panic. Ask: What’s the pattern? Is it just a little up, or way out of range? Is it just ALT or both ALT and AST? Is bilirubin or albumin affected? And most importantly-what does my life look like? Alcohol? Weight? Medications? Because the answer isn’t in the lab report. It’s in your story.
If your liver tests are abnormal, your next steps depend on the pattern:
Most people with mildly elevated liver tests never develop serious disease. But catching it early-before scarring sets in-is the key. Your liver is strong. It can heal. But it needs time. And the right choices.
A high ALT level usually means liver cells are damaged or inflamed. ALT is mostly found in the liver, so when it rises, it’s a strong sign of liver injury. Common causes include fatty liver disease (MASLD), viral hepatitis, alcohol use, or certain medications. But mild elevations (under 2x the upper limit) can happen in healthy people, especially those with obesity or after intense exercise.
Yes. An AST/ALT ratio greater than 2 is strongly linked to alcohol-related liver disease. In alcoholic hepatitis, AST often rises 2-6 times the normal level, while ALT only goes up 1-2 times. This happens because alcohol affects liver cells differently than viruses or fat. If the ratio is below 1, fatty liver or viral hepatitis is more likely.
Yes. Unconjugated bilirubin can rise due to conditions like Gilbert’s syndrome-a harmless genetic condition that affects bilirubin processing. It’s common, affects up to 10% of people, and causes mild jaundice during stress or fasting. Conjugated bilirubin, however, usually means a problem with bile flow-like gallstones or liver disease.
ALP can rise even when ALT is normal if bile flow is blocked. This happens in gallstones, bile duct narrowing, or liver diseases like primary biliary cholangitis. But ALP is also made in bones, so if you have a fracture or bone disease, ALP can be high without liver issues. That’s why doctors check GGT too-if GGT is normal but ALP is high, they’ll look at bones instead of liver.
Not necessarily. Mild elevations (under 2x the upper limit) are common and often temporary. They can be caused by recent alcohol use, obesity, medications, or even a recent illness. Most people don’t need immediate scans or treatment. Instead, doctors recommend lifestyle changes-lose weight, stop drinking, control blood sugar-and repeat the test in 3-6 months. Only if levels stay high or keep rising does further testing become necessary.
Not always. In early cirrhosis, ALT and AST may be normal or only slightly raised. The real signs of advanced cirrhosis are low albumin and prolonged prothrombin time-because the liver can’t make these proteins anymore. That’s why doctors use other tools like FIB-4 scores, ultrasound, or elastography to check for scarring. LFTs alone aren’t enough to diagnose cirrhosis.
ALT and AST rise within 6-12 hours of liver injury and peak in 24-48 hours. ALT has a half-life of about 47 hours, so it stays elevated longer than AST (which lasts 18-24 hours). In acute injury, levels can stay high for 3-7 days. In chronic disease, they may stay mildly elevated for months or years. But if levels keep dropping after peaking, it’s a good sign the liver is healing.
If you’ve had abnormal liver tests, the most important thing isn’t the number-it’s what you do next. Cut back on alcohol. Lose weight if you’re overweight. Control your blood sugar. Don’t take unnecessary pills. And give your liver time to recover. It’s the most resilient organ you’ve got.
I swear, my doctor looked at my ALT and started talking about cirrhosis like I was already dead. I drink maybe once a month and I’m 28. I think they just wanna sell you an ultrasound.
Oh sweet baby Jesus, another person who thinks 'normal range' means 'you're fine.' 😭 The normal range is based on the dumbest 80% of the population who eat fast food and nap after soda. If your ALT is over 40 and you weigh more than your dignity, you're not 'slightly elevated'-you're one beer away from a liver transplant. Stop self-diagnosing with WebMD and go do a damn liver ultrasound before you turn into a walking jaundice billboard.
I’m so tired of people brushing off elevated liver enzymes like it’s just a cold. 😔 You think it’s ‘mild’? That’s your liver screaming into a pillow while you binge Netflix and eat chips. I had a friend who ignored her AST for 2 years-now she’s on the transplant list. Don’t be her. Cut the sugar. Cut the booze. Cut the denial. 💔
I appreciate the breakdown. I had a weird ALP spike last year and it turned out to be a stress fracture from hiking. My doctor didn’t even check GGT at first. Glad to know it’s not always liver-related. Took me 3 months to get answers though...
It is imperative to underscore that the AST/ALT ratio, when exceeding a threshold of 2.0, constitutes a statistically significant biomarker indicative of alcoholic hepatocellular injury, with a specificity of approximately 90% in controlled cohort studies (AASLD, 2023). Further, the diagnostic utility of FIB-4 indices should be prioritized over non-specific enzymatic elevations in primary care settings.
I’ve been trying to understand my own numbers since my last checkup. My ALT was 62 and AST was 58. I don’t drink, I’m not overweight, and I eat clean. I thought it was just stress or maybe some supplement I took. I’m waiting on the follow-up. It’s scary how much your body can be screaming and you feel fine.
liver dont care if u r rich or famous. it just wants u to stop drinking soda and eating pizza at 2am. mine was high for 6 months. i lost 20lbs. now its normal. no meds. just food. its that simple.
My mom had fatty liver and she didn’t even know it till she got dizzy and passed out. I started drinking lemon water and walking daily. Now her numbers are normal. It’s not magic, it’s just consistency. You can heal if you try 💪
I went to the doctor with a high AST and she said 'maybe you’re just stressed' 😒 I cried in the parking lot. I didn’t know if I was dying or just lazy. But I cut out alcohol, started sleeping 8 hours, and guess what? My ALT dropped 40 points in 3 months. Your liver is a warrior. Treat it like one. 🙏
The AST/ALT ratio is underutilized in primary care. I’ve reviewed over 300 cases in my practice. When the ratio exceeds 2:1, alcohol is the most probable etiology-regardless of patient denial. Early intervention is critical.
I come from a family where everyone has fatty liver. We never talk about it. But after reading this, I think I’ll start a small group-just people checking in on each other’s numbers. Maybe we can help each other before it’s too late.
i had bilirubin high once and thought i had hepatitis. turned out i was just dehydrated and ate too much beetroot. lol. my doc laughed. liver is weird.
Wow. A 10-page essay on how to read a blood test. Congrats. You just invented the world’s most expensive Wikipedia page.