Hypoglycemia isn’t just a buzzword for people with diabetes-it’s a real, daily risk that can turn a normal morning into an emergency in minutes. When your blood sugar drops below 70 mg/dL (3.9 mmol/L), your body starts sending warning signals. But if you miss them, you could end up confused, shaking, unconscious, or worse. The good news? Almost every episode of low blood sugar can be stopped, reversed, and prevented with the right knowledge.
People often think low blood sugar means you’re just hungry. But it’s more than that. Your brain runs on glucose. When levels drop, your body panics. You might feel your heart race, your hands shake, or break out in a cold sweat. These are your body’s alarm systems-adrenergic symptoms-triggered by adrenaline rushing to raise your blood sugar.
But if it keeps dropping, your brain starts to starve. That’s when neuroglycopenic symptoms kick in: blurry vision, trouble speaking, dizziness, confusion, or even seizures. At 50 mg/dL or lower, you might not even realize you’re in danger. That’s called hypoglycemia unawareness, and it affects nearly 1 in 4 people who’ve had Type 1 diabetes for more than 15 years.
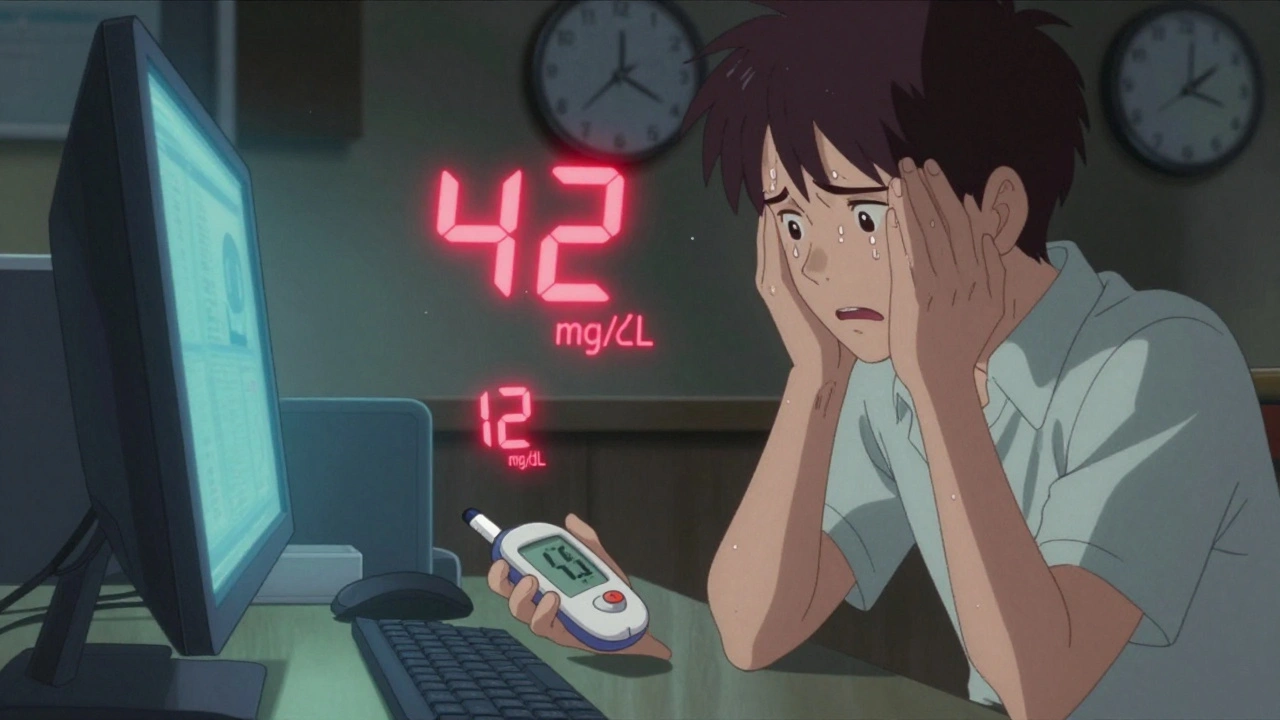
One user on a diabetes forum described it like this: “I was at work, and my hands were shaking so hard my glucose meter rattled. I thought I was having a panic attack-until I checked and saw 42 mg/dL.” That’s not anxiety. That’s your brain screaming for fuel.
In people with diabetes, most hypoglycemia episodes come down to three things: too much insulin, not enough food, or too much movement.
Non-diabetics can get low blood sugar too, but it’s rarer. Reactive hypoglycemia happens after meals-often after gastric bypass surgery-and fasting hypoglycemia can signal something more serious, like an insulin-producing tumor (insulinoma) or liver or kidney failure.
If you’re alert and able to swallow, the standard fix is the 15-15 rule: eat or drink 15 grams of fast-acting carbs, wait 15 minutes, then check your blood sugar again.
Good choices:
Don’t use candy bars or whole meals. Fat and protein slow down sugar absorption, and you need speed.
After 15 minutes, retest. If you’re still below 70 mg/dL, repeat. Once you’re back above 70, eat a snack with protein and complex carbs-like peanut butter on crackers-to keep your levels steady.
But here’s the catch: the 15-15 rule fails in about 22% of cases. If you’re confused, vomiting, or unconscious, you can’t swallow safely. That’s when you need glucagon.
Glucagon is a hormone that tells your liver to dump stored glucose into your blood. It comes as an injection or nasal spray. The new nasal version (Dasiglucagon) works in under 10 minutes and doesn’t need mixing. It’s now FDA-approved and easier for family members to use.
Every person with diabetes on insulin should have glucagon on hand-and so should their family, coworkers, or friends. Train them. Keep it in your bag, your car, your desk drawer. Don’t wait for a crisis to find out where it is.

Checking your blood sugar is necessary-but not enough. Prevention means planning ahead.
1. Know your patterns. Do you always dip after afternoon walks? Do you crash if you skip breakfast? Keep a log. Over time, you’ll spot your personal triggers.
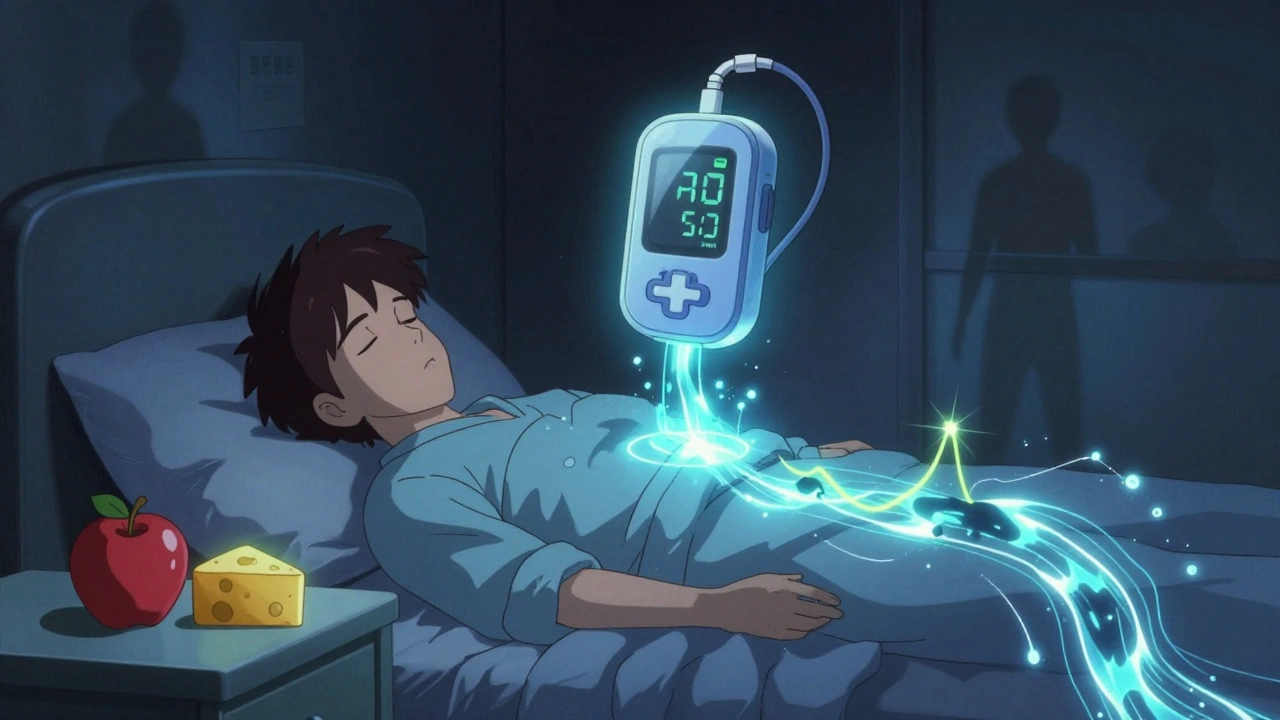
2. Use technology. Continuous glucose monitors (CGMs) are game-changers. They don’t just tell you your current level-they show trends. A CGM that alerts you when your sugar is dropping fast gives you time to act before you feel sick. The latest systems even pause insulin automatically if your sugar starts to plummet. Studies show this cuts nighttime lows by nearly half.
3. Adjust for exercise. If you’re going to be active for more than 45 minutes, reduce your basal insulin by 20-50% or eat 15-30 grams of carbs before starting. Recheck every 30 minutes during longer workouts.
4. Eat consistently. Don’t skip meals. If you’re on insulin, your carb intake should match your dose. A general rule: 1 unit of insulin covers 10-15 grams of carbs, but that varies by person. Work with your doctor to find your ratio.
5. Sleep smart. Nocturnal hypoglycemia is dangerous because you’re asleep and can’t react. Set your CGM alarm for 55 mg/dL at night. Some people eat a small bedtime snack with protein and slow-digesting carbs-like cheese and an apple-to prevent drops.
Not every low blood sugar needs an ambulance-but some do.
Call 999 or go to the ER if:
Emergency rooms see about 100,000 hypoglycemia cases a year in the U.S. alone-and nearly a third of them are misdiagnosed as strokes or drunkenness. If you’re with someone who looks “drunk” but isn’t, check their blood sugar. It could save their life.
Older adults often don’t show classic symptoms. Instead of shaking or sweating, they might fall, get confused, or seem “out of it.” These episodes are linked to higher dementia risk and increased death rates. If you’re caring for an elderly person with diabetes, watch for subtle changes in behavior.
For children, hypoglycemia can look like tantrums, crying, or refusal to eat. Parents often think it’s just moodiness. But if a child suddenly becomes unusually irritable after school or during play, check their sugar. Kids’ brains are especially sensitive to drops in glucose.
Technology is moving fast. The latest artificial pancreas systems now predict lows before they happen-using AI to analyze glucose trends, activity, and meals. One system, Tandem Control-IQ, reduces time spent below 54 mg/dL by over three hours a week.
Researchers are also testing glucose-responsive insulin-insulin that turns itself off when blood sugar drops below 70 mg/dL. Early trials show it cuts hypoglycemia by more than 60% compared to traditional insulin.
And if cost is a barrier, telehealth programs are proving effective. One study showed a 41% drop in severe episodes among Medicaid patients who got regular virtual coaching.
Yes, but it’s rare. Non-diabetic hypoglycemia usually falls into two types: reactive (after eating) or fasting (during long gaps between meals). Reactive hypoglycemia can follow bariatric surgery, while fasting hypoglycemia may signal tumors, liver disease, or hormone disorders. If you’re not diabetic and keep getting low blood sugar, see a doctor for testing.
This is called hypoglycemia unawareness. It happens when your body gets used to frequent lows and stops releasing adrenaline-the hormone that causes shaking, sweating, and racing heart. It’s common after 15+ years of Type 1 diabetes. The only way to regain awareness is to avoid lows for several weeks, which often means raising your target blood sugar range temporarily under medical supervision.
Yes-but only if your blood sugar is above 70 mg/dL. At 50 mg/dL, your reaction time and judgment are as impaired as someone with a 0.08% blood alcohol level-the legal limit for driving in most places. Always check your sugar before driving. Keep fast-acting carbs in the car. If you feel symptoms while driving, pull over immediately. Don’t wait.
There’s no single “best” snack-it depends on timing. For a quick fix, use 15g of fast carbs. To prevent a crash later, pair that with a slow-digesting carb and protein: apple with peanut butter, cheese with whole-grain crackers, or yogurt with a handful of nuts. This combo gives you immediate energy and keeps your blood sugar steady for hours.
Stress usually raises blood sugar-but in some people, especially those with Type 1 diabetes, it can trigger a drop. This happens when stress causes you to skip meals, over-exercise, or forget insulin doses. Emotional stress can also make you less aware of early symptoms. Managing stress through sleep, routine, and support networks helps reduce hypoglycemia risk.
If you’re on insulin or prone to lows, check before meals, before bed, before driving, and after exercise. If you’ve had a recent low, check again 15-30 minutes after treating it. People with hypoglycemia unawareness should check even more often-every 2-3 hours during high-risk times. CGMs reduce the need for fingersticks but don’t eliminate the need to verify with a meter if symptoms don’t match the reading.
Hypoglycemia is scary-but it’s not inevitable. Millions of people manage it every day. The key isn’t perfection. It’s preparation. Know your signs. Carry treatment. Teach others. Use your tools. And if you’ve had a scary episode, talk to your healthcare team. There are better ways to prevent it than just hoping for the best.
Just had a scary low at work last week. Shaking like a leaf, thought I was having a panic attack. Checked my CGM-48 mg/dL. Ate 4 glucose tabs, sat down for 15 mins. Still felt weird but didn’t crash. Never ignoring symptoms again.
Also-glucagon in my purse now. No excuses.
I’ve been managing Type 1 for 22 years and hypoglycemia unawareness hit me hard around year 15. I stopped feeling the shakes, the sweat, the racing heart-until I passed out in the grocery store. No warning. Just black.
My endo had me raise my targets to 120-160 for six months. It was brutal. No more midnight lows, no more 3 a.m. panic. Slowly, my body relearned how to scream. Now I get the warning signs again-just not as loudly. It’s a trade-off, but worth it. If you’re unaware, talk to your doctor about this. Don’t wait for a seizure.
This post made me tear up a little. My sister’s 12-year-old had a low at school last month. Teacher thought she was being dramatic. Turned out she was at 39. They didn’t have glucagon.
Now I’m pushing our PTA to train staff. No kid should be left helpless because adults don’t know what a low looks like. 😔
I just want to say… I know this is a lot of info. But please, if you’re reading this and you’re new to this-don’t feel overwhelmed. You don’t have to do it all at once. Start with one thing. Maybe just keep juice in your car. Or check your sugar before you drive. Tiny steps matter. You’re doing better than you think.
I’ve seen so many people on here act like they’re victims of their own bodies. Look, if you’re diabetic and you’re constantly low, maybe you’re not managing it right. I’ve been on insulin for 10 years and I haven’t had a single severe low since I stopped eating junk and started tracking my carbs like a scientist. Stop blaming the disease. Take responsibility.
The 15-15 rule? Pathetic. If you’re relying on glucose tabs and juice, you’re already behind. Real prevention is about basal rate tuning, carb ratios, and predictive algorithms. Why are people still using fingersticks in 2025? If you don’t have a CGM and an AI-driven pump, you’re basically flying blind. And no, your ‘snack with peanut butter’ isn’t going to save you from a 3 a.m. crash. Get with the times. 💪📱
Thank you for this comprehensive and well-researched guide. I especially appreciate the emphasis on glucagon accessibility and the distinction between neuroglycopenic and adrenergic symptoms. As a healthcare provider, I share this with all my patients on insulin therapy. Prevention through pattern recognition and technology is not just ideal-it is essential. Keep sharing knowledge like this.
Everyone’s acting like this is new info. I’ve been screaming about CGMs since 2018. If you’re still finger-sticking every 2 hours, you’re wasting your life. Also, if you think chocolate helps, you’re not just wrong-you’re dangerous. Stop being lazy. Get a Dexcom. Period.
I used to think I was just clumsy. Then I started blacking out after lunch. Turns out I was crashing hard. My doc said it was reactive hypoglycemia. Cut out the white bread, started eating protein with every meal. No more dizzy spells. It’s not diabetes, but it’s still real. If you feel off after eating, get tested.
My dad’s 74 and has Type 2. He doesn’t get the shakes. Just gets quiet. Stops talking. Looks confused. We thought it was aging. Then he fell once and they checked his sugar-38. We started checking before meals. Now he has a CGM. He’s back to telling his stories. Don’t ignore the quiet ones. They’re screaming.
I’ve been using the new nasal glucagon since it came out. My wife gave it to me after I passed out last year. She didn’t even need to read the instructions. Just sprayed it in. I woke up 10 minutes later. Best $150 I ever spent. Also, I now keep it in my glovebox, my backpack, and my desk. No more ‘I didn’t know where it was.’ 🙏
i had a low at the gym last week and thought i was just tired… turned out i was at 41. my trainer had no idea what to do. i had to pull out my meter and scream for juice. dont let this happen to you. always have something with you. even if you think you’re fine.