
When you have asthma, inhaled corticosteroids (ICS) are often the most effective way to keep your lungs calm and prevent flare-ups. But for many people, the fear of side effects is real - and it’s not just a myth. Oral thrush, hoarse voice, bruising, even bone thinning - these aren’t rare. They happen. And if you’re on a high dose for years, the risks add up. The good news? Most side effects are preventable. You don’t have to choose between breathing well and feeling sick from your medicine. With the right technique, dose, and monitoring, you can use these drugs safely - even long-term.
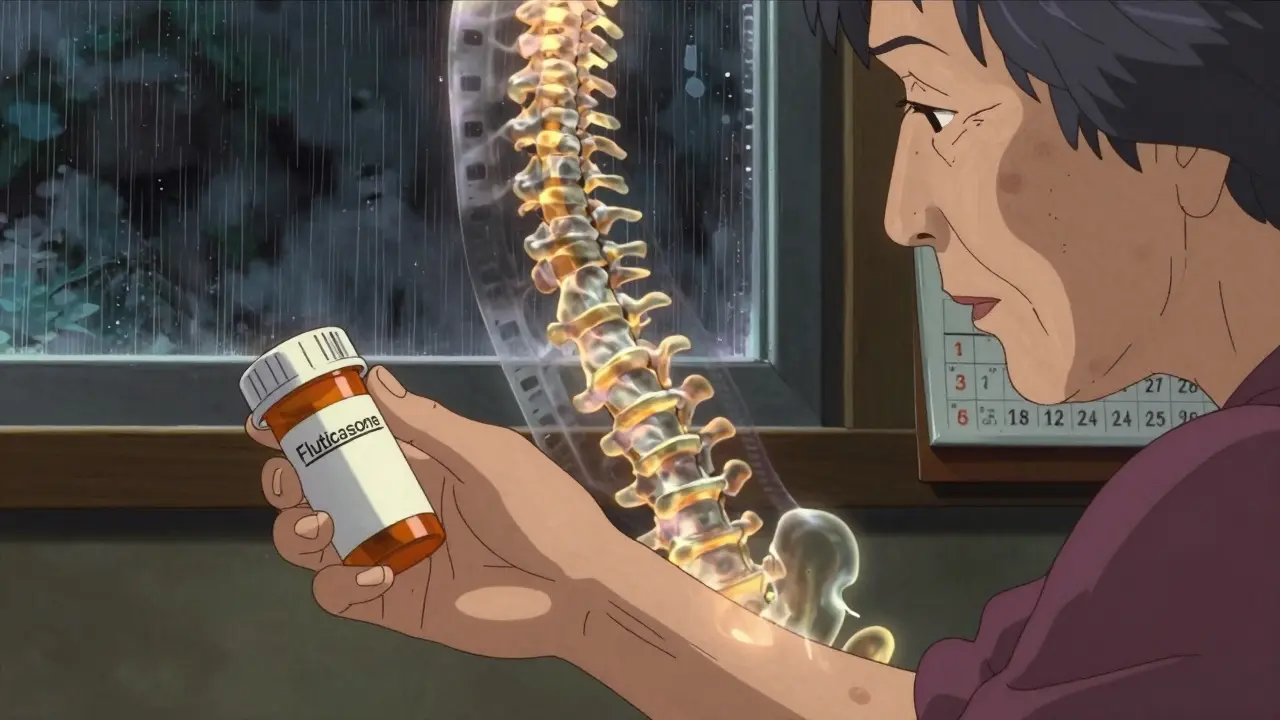
Inhaled corticosteroids aren’t the same as the oral steroids athletes take. They’re designed to work right where you need them: in your airways. Brands like fluticasone, budesonide, mometasone, and ciclesonide all target inflammation in your lungs. That’s what stops wheezing, coughing, and tightness before it starts. The key word here is inhaled. When you use them correctly, less than 10% of the dose even gets into your bloodstream. The rest stays put in your lungs, doing its job without causing widespread harm.
But here’s the catch: if you don’t rinse your mouth after using your inhaler, or if you don’t use a spacer, you’re swallowing a lot of that medicine. That’s when side effects start. It’s not the drug itself that’s dangerous - it’s how it’s delivered.
Most side effects from inhaled steroids are local - meaning they happen right in your mouth and throat. The most common ones?
These aren’t signs your body is failing. They’re signs your technique needs fixing.
Here’s what actually works:
One patient on Reddit said: "I had thrush every month until I got a spacer. Now it’s been 18 months without one. It’s not the medicine - it’s how I used it." That’s the story for most people.
When you’re on low or moderate doses (under 400 mcg/day of beclomethasone equivalent), systemic side effects are rare. But if you’re on high doses - say, 1000 mcg/day or more - the risk changes.
High-dose ICS can lead to:
But here’s the key: these aren’t automatic. They’re dose-dependent. A 2021 study found fluticasone at 500 mcg/day carried nearly 3 times the risk of adrenal suppression compared to budesonide at the same dose. Why? Because budesonide and ciclesonide break down faster in the body. They’re designed to be safer.
If you’re on high-dose ICS, your doctor should check:
And if you’re a parent of a child on ICS? Don’t panic. Growth delays are real, but small. On standard doses, kids grow about 0.7 cm less per year than peers - but catch up by adulthood. High doses (>800 mcg/day) are where you need to be more careful.
Not all inhaled steroids are the same. Some are designed to be safer than others.
| Medication | Systemic Bioavailability | Typical Daily Dose | Relative Risk of Side Effects |
|---|---|---|---|
| Fluticasone propionate | 30-40% | 100-500 mcg | Higher |
| Budesonide | 10-15% | 200-800 mcg | Moderate |
| Ciclesonide | 2-3% | 80-320 mcg | Lowest |
| Mometasone furoate | 8-12% | 100-400 mcg | Low |
Ciclesonide and mometasone are newer and designed to activate only in the lungs. They’re often better choices if you’re on long-term therapy or worried about side effects. Budesonide is a solid middle ground - effective and well-studied. Fluticasone works, but it’s more likely to cause problems at higher doses.
For pregnant women, budesonide is the only ICS with strong safety data. It’s classified as Category B - meaning no increased risk of birth defects after 15+ years of tracking. Fluticasone is Category C - meaning we don’t have enough data to say it’s safe. If you’re pregnant or planning to be, talk to your doctor about switching.
Most people never get a full side effect check. A 2023 report found only 39% of primary care providers routinely ask about thrush, voice changes, or bruising during asthma visits. That’s unacceptable.
Here’s what a good asthma review should include every 3-6 months:
If you’re on more than 300 mcg/day of fluticasone equivalent for over 6 months, your doctor should consider a cortisol test. Fatigue, dizziness, nausea - these aren’t "just stress." They could mean your adrenal glands are tired.
And don’t ignore your own body. If you notice:
- tell your doctor. Don’t wait for your next appointment.
There’s good news on the horizon. Newer ICS drugs like AZD7594 are being tested and show 90% less adrenal suppression than fluticasone. They’re not on the market yet, but they’re coming.
For people with severe asthma, biologics like dupilumab and mepolizumab are already changing the game. In one study, patients on these drugs reduced their ICS dose by 70% - without losing control. If you’re still on high-dose steroids and having flare-ups, ask your specialist if a biologic might help you cut back.
And don’t forget smart inhalers. These devices track when you use your inhaler and whether you’re using it right. One study found they improved technique in 85% of users within 3 months. If your inhaler doesn’t have a smart chip, ask if your clinic offers one.
Inhaled steroids save lives. They prevent ER visits, hospital stays, and missed work. But they’re not harmless. The side effects aren’t scary if you know how to manage them.
Here’s your simple plan:
You don’t have to choose between breathing well and feeling bad. With the right tools and awareness, you can do both.
Unlike oral steroids, inhaled steroids rarely cause weight gain. The dose that reaches your bloodstream is too low to affect metabolism or appetite. If you’ve gained weight while using an inhaler, it’s more likely due to reduced activity from asthma symptoms improving, or other factors like diet or hormones. Weight gain is not a typical side effect of properly used inhaled steroids.
No. Asthma is a chronic condition, even when you feel fine. Stopping your inhaler can lead to worsening inflammation, which may cause a severe flare-up. Always talk to your doctor before making any changes. They may lower your dose gradually, but never stop abruptly. Many people can reduce their dose over time - but only under medical supervision.
Yes, if you’re on the lowest effective dose and use proper technique. Millions of people use inhaled steroids for decades with no major issues. The risks increase with high doses and poor technique, not with time alone. Regular monitoring - like checking for bone thinning or adrenal function - helps keep long-term use safe. The benefits of preventing asthma attacks far outweigh the risks when managed correctly.
Hoarseness happens when steroid particles settle on your vocal cords, causing mild irritation or fungal overgrowth. It’s not damage - it’s a sign your medicine isn’t reaching your lungs. Using a spacer and rinsing your mouth after each puff cuts this risk by more than half. If it persists after 2 weeks of proper technique, see your doctor - you may need a different inhaler or treatment for thrush.
Children on standard doses (under 400 mcg/day) show only a tiny, temporary slowdown in growth - about 0.7 cm per year. This catches up by adulthood. High doses (>800 mcg/day) may increase cataract risk slightly and should be avoided unless necessary. Always use a spacer and rinse after use. Regular growth checks are part of good asthma care for kids. The risk of uncontrolled asthma - missed school, hospital visits, long-term lung damage - is far greater than the risk from proper steroid use.
Don’t stop taking it. Call your doctor or asthma nurse. Bring your inhaler to the appointment so they can watch you use it. Ask: "Can I lower my dose?" and "Should I switch to a different steroid?" They may recommend a spacer, a rinse routine, or a different medication like ciclesonide or budesonide. Most side effects are reversible once the cause is fixed. The goal isn’t to avoid steroids - it’s to use them smarter.
I used to skip rinsing after my inhaler. Ended up with thrush so bad I couldn't eat spicy food for weeks. Spacers changed everything. No more white patches, no more hoarse voice. Just breathe.
The data on systemic absorption differences between budesonide and fluticasone is critical. Many clinicians still default to fluticasone due to cost or habit, but the pharmacokinetic profile of budesonide and especially ciclesonide makes them far preferable for long-term use. This is not just anecdotal-it's evidence-based practice.
I've been on budesonide for 8 years. Used to get thrush every other month until my asthma nurse showed me how to use a spacer properly. Now I rinse, spit, brush, and go. No issues. It's not the drug-it's the delivery. Simple as that.
If you're on high-dose ICS and feeling tired all the time, don't just blame stress. Adrenal fatigue is real. I had mine checked after months of exhaustion-turns out my cortisol was barely detectable. Switched to ciclesonide, dropped my dose, and now I have energy again. Talk to your doctor. Seriously.
My daughter's been on inhaled steroids since she was 4. She's 14 now. Grew 0.5 cm less per year than her siblings-but caught up by 16. No cataracts, no bruising, no thrush. Spacers + rinsing = magic. Don't fear the inhaler. Fear the asthma attack more.
It's fascinating how the body's response to localized vs systemic delivery creates such a stark contrast in risk profiles. The fact that less than 10% of the dose enters circulation when used correctly suggests that the real enemy isn't the pharmacology-it's the human error in technique. We've built incredibly precise tools, yet our adherence to basic steps remains shockingly inconsistent. Is this a failure of education? Or of motivation? Or both?
I think the pharmaceutical companies are hiding the real risks. Why do you think they push fluticasone so hard? It's cheaper for them. I read a paper once that said steroid inhalers cause infertility in men. I didn't see it on the label. That's why I stopped using mine. My asthma is fine now anyway. I breathe through my nose and meditate. It works.
This post is just pharma propaganda. Everyone knows steroids make you fat and weak. Why are you still using them? Just go to a chiropractor or drink apple cider vinegar. It's cheaper and no side effects.
In India we don't even have spacers in most clinics. People just spray and swallow. And you wonder why we have so many lung problems? This is why western medicine is overrated. We need better training, not more pills.
I work with elderly patients who’ve been on fluticasone for a decade. Bruising like they’ve been in a boxing match. One woman had three hip fractures in two years. We switched her to ciclesonide, added a spacer, started vitamin D, and now she’s hiking again. It’s not about avoiding meds-it’s about choosing smarter ones. The system fails people when it doesn’t teach them how to use what they’re given.
I think the real problem is doctors don’t check your technique. I’ve been using my inhaler wrong for 10 years and no one ever said a word. I just thought I was supposed to cough after I sprayed it. My throat is always sore. Maybe I’m not alone?
I used to think I was allergic to steroids until I learned to rinse. Now I’m on ciclesonide with a spacer and I feel like I’ve been reborn. No more hoarseness. No more thrush. No more fear. Just air. Just life. Just breathe.