
When a tough day leaves you with a tight, swollen belly, you may be experiencing Tympanites a condition marked by excess gas and abdominal distension. It’s not just what you ate; it’s also what’s happening in your mind. Stress the body’s response to perceived threats, releasing hormones such as cortisol can hijack your digestive system, turning a normal meal into a bloated nightmare.
Below, we’ll walk through how the gut‑brain axis a two‑way communication network between the central nervous system and the gastrointestinal tract works, why cortisol the primary stress hormone that influences metabolism and inflammation matters, and what practical steps you can take to keep stress and gut health on the same side.
Tympanites, often called abdominal bloating, happens when gas builds up faster than it can be expelled. Common triggers include:
Symptoms range from a mild, uncomfortable fullness to a visibly distended belly that can be painful. While occasional bloating is normal, chronic tympanites often signals an underlying imbalance.
Stress isn’t just a feeling; it’s a cascade of biochemical events. When you perceive a threat, the hypothalamus activates the HPA axis the hypothalamic‑pituitary‑adrenal system that regulates stress hormones. This triggers cortisol release, which does three things for your gut:
Meanwhile, the vagus nerve the main parasympathetic conduit linking brain and gut receives stress signals and reduces its normal “rest‑and‑digest” tone. The outcome? Spasms, slower peristalsis, and more gas trapped in the intestines.
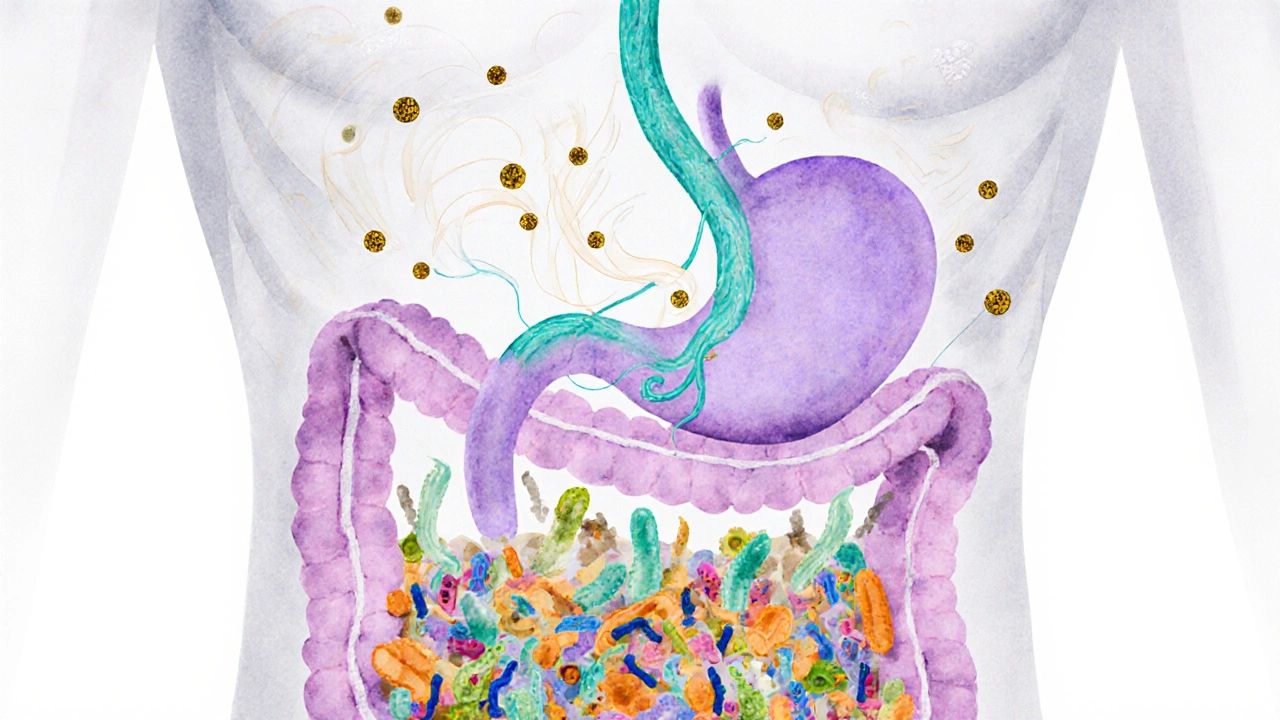
Think of the gut‑brain axis as a highway with multiple lanes. One lane carries neural signals via the vagus nerve, another carries hormonal messages like cortisol, and a third moves chemical messengers such as serotonin a neurotransmitter largely produced in the gut that regulates mood and motility. When stress floods the system, each lane gets jammed:
The result is a feedback loop: bloating makes you feel uncomfortable, which raises stress, and the cycle repeats.
It’s easy to blame the dinner you ate, but notice these patterns that point to a mental‑physical link:
If you can match at least two of these clues, stress is likely a major player in your tympanites.
Here’s a toolbox you can start using today. Each tip tackles a different part of the stress‑to‑bloat pathway.

| Stress Level | Gut Motility | Gas Production | Microbiome Diversity |
|---|---|---|---|
| Low | Normal | Baseline | High |
| Moderate | Slightly slowed | Increased | Reduced |
| High | Significantly slowed | High | Low |
Use this table as a visual cue: as stress climbs, the gut’s ability to move food and gas efficiently drops, while harmful bacterial overgrowth rises.
If you experience any of the following, book a visit:
These could signal conditions like celiac disease, inflammatory bowel disease, or gallbladder issues-each requiring medical diagnosis.
Yes. Anxiety spikes cortisol and speeds up breathing, both of which increase swallowed air and alter gut motility, leading to gas buildup.
Research shows specific strains-like Bifidobacterium infantis-reduce cortisol‑induced gas by up to 30% after four weeks of daily use.
A strict low‑FODMAP diet can limit beneficial fibers. Use it as a short‑term test (2‑6 weeks) and then reintroduce foods to find your personal tolerance.
Many people feel relief within 5‑10minutes as the vagus nerve shifts back to “rest‑and‑digest,” easing sphincter tension and helping gas pass.
Poor sleep raises baseline cortisol, which in turn slows digestion and encourages bacterial overgrowth, making bloating more likely.
The intricate neuroendocrine circuitry governing the gut‑brain axis operates via a symphony of afferent vagal pathways, hypothalamic‑pituitary‑adrenal feedback loops, and microbiota‑derived metabolomic signaling.
When cortisol concentrations surge, they engage glucocorticoid receptors on enteric neurons, attenuating peristaltic rhythm and fostering an anaerobic milieu conducive to gas‑producing taxa.
Concomitantly, the vagus nerve experiences diminished tonic activity, precipitating sphincter hypertonicity that entraps luminal gases.
Such physiologic dysregulation manifests clinically as tympanites, wherein intraluminal pressure exceeds the viscerosensory threshold.
Empirical studies employing functional magnetic resonance imaging have corroborated a bidirectional modulatory effect between prefrontal cortical stress processing and myenteric plexus excitability.
Notably, the insular cortex integrates interoceptive cues, thereby amplifying the affective experience of bloating.
From a molecular perspective, stress‑induced alterations in tight junction protein expression augment intestinal permeability, facilitating translocation of endotoxins that further exacerbate dysbiosis.
The resultant dysbiotic profile is typified by an overrepresentation of methanogenic archaea and fermentative Firmicutes.
Interventionist paradigms therefore necessitate a multimodal approach targeting both neurohormonal and microbial axes.
Evidence‑based modalities include diaphragmatic breathing techniques that restore vagal tone, targeted probiotic supplementation with strains such as Bifidobacterium infantis, and low‑FODMAP dietary modifications to reduce fermentable substrate availability.
Chronobiological alignment of sleep cycles also mitigates basal cortisol output, thereby normalizing gut motility.
In clinical practice, a composite assessment integrating psychometric stress scales with stool microbiome profiling yields the most predictive appraisal of tympanites risk.
Future translational research ought to elucidate the epigenetic imprint of chronic stress on enteric glial cell function.
In sum, the pathophysiology of stress‑related abdominal distension is a confluence of endocrine, neural, and microbial perturbations, each of which offers a therapeutic foothold.
By adopting an integrative regimen that harmonizes mind‑body practices with microbiota‑centric interventions, patients can effectively attenuate the visceral sequelae of chronic stress.
Yo, stress makes my belly feel like a busted balloon 🎈😅.
The relationship between our mental state and digestive function is a profound illustration of the unity of body and mind.
When we dwell in anxiety, the cascade of cortisol and adrenaline subtly reshapes the rhythm of our intestines.
This physiological shift often manifests as uncomfortable bloating, a reminder that our emotions are not confined to the brain.
Understanding this connection can empower us to adopt practices that calm the nervous system, such as mindful breathing.
In turn, a calmer gut can foster a more tranquil mind, creating a virtuous circle.
It is through such reciprocal awareness that we can reclaim balance in both realms.
Totally agree!!
Mindful breathing really does the trick ;)
Stop blaming food; the mind is the real culprit.
One practical tip is to set a timer for a 5‑minute walk after each meal.
This light activity stimulates peristalsis and helps move gas along.
Another simple habit is to sip warm water infused with lemon instead of carbonated drinks.
Both approaches are low‑effort yet can noticeably reduce bloating episodes.
Consistency is key; small daily actions compound over time.
Honestly the article overcomplicates simple gut stuff.
Just eat, sleep, and chill.
From a clinical perspective, integrating a short breathing exercise like 4‑7‑8 before meals can directly modulate vagal tone.
Coupled with a low‑FODMAP meal plan on high‑stress days, patients often report reduced gas retention.
Probiotic supplementation, particularly strains targeting inflammation, further supports microbiome balance.
Ensuring at least seven hours of quality sleep each night helps keep baseline cortisol low, preventing chronic dysmotility.
Regular post‑lunch walks of ten minutes are an inexpensive yet effective way to stimulate peristalsis.
Finally, consider a brief journaling session to identify stress triggers, enabling targeted behavioral adjustments.
Oh great, another 6‑step miracle cure 🙄.
Everyone reading this should feel empowered to take small, sustainable steps toward better gut health.
Start with a single habit, like a nightly breathing routine, and observe how your digestion responds.
When you notice improvement, add another layer such as a brief walk after lunch.
Over weeks, these micro‑changes accumulate, leading to noticeable reductions in bloating and discomfort.
Remember, consistency beats intensity; a modest daily practice is more valuable than an occasional marathon effort.
Support from friends or a community can also reinforce accountability.
Stay patient, stay kind to yourself, and celebrate each incremental victory.
Honestly i think all this gut‑brain hype is just a marketing ploy to sell supplements.
People ignore basic diet and blame stress for everything.
It’s simple: eat less junk and you’ll be fine.
Don’t overcomplicate it.