
This assessment helps determine if you need medical attention based on the duration, symptoms, and impact of your hiccups.
Score: 0/10
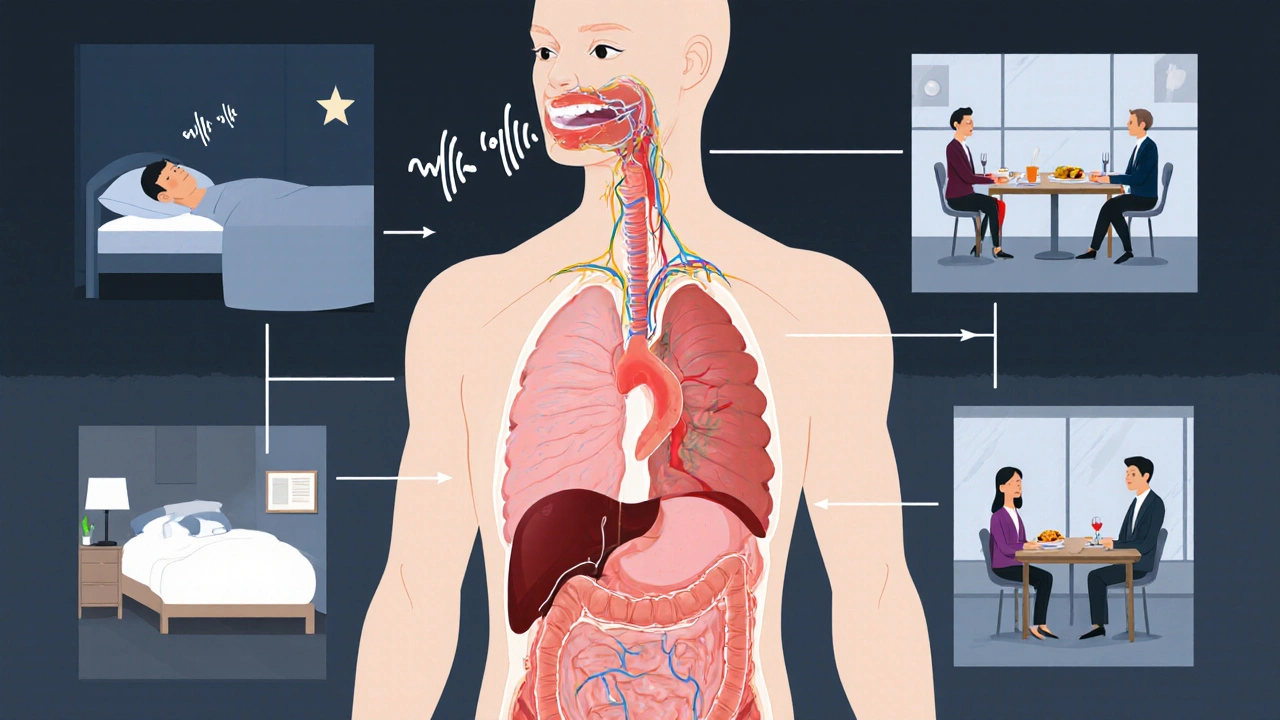
When a sudden hiccup is a brief, involuntary contraction of the diaphragm followed by a rapid closure of the vocal cords, creating the classic "hic" sound, most people brush it off as a harmless nuisance. Yet for a surprising number of individuals, especially when episodes linger, the impact can reach far beyond a momentary embarrassment. Below we explore how hiccups shape daily routines, sleep, social interactions, and even mental health, and we give you practical steps to regain control.
Understanding the root cause helps you predict and prevent trouble. The reflex arc that generates a hiccup involves three main players:
Common everyday triggers include:
Most hiccup bouts resolve within minutes. However, if an episode lasts longer than 48 hours, clinicians label it chronic hiccups is a persistent hiccup condition that can extend weeks, months, or even years. The real concern isn’t the sound; it’s the cumulative toll on quality of life.
Key ways chronic hiccups degrade daily living:
A 2023 study from a European gastroenterology journal found that patients with hiccups lasting over a week reported a 35% drop in self‑rated health‑related quality of life scores, comparable to chronic migraine sufferers.
Before jumping to treatments, a quick self‑assessment can tell you whether medical help is needed. Ask yourself:
If you answer “yes” to any of these, schedule a medical evaluation is a consultation with a primary‑care physician or gastroenterologist to rule out underlying disease. The doctor may order blood tests, imaging, or a referral to a neurologist if a nerve issue is suspected.
For most short‑term episodes, simple lifestyle tweaks offer relief. Below is a comparison of the most commonly recommended remedies, ranked by effectiveness based on a meta‑analysis of 12 clinical trials (2022‑2024).
| Remedy | Typical Success Rate | Side Effects | Practical Notes |
|---|---|---|---|
| Holding breath (30‑60seconds) | ≈45% | None | Easiest to try; works best early in an episode. |
| Cold water sip (½cup) | ≈38% | None | Stimulates vagus nerve; avoid if you have severe reflux. |
| Sugar cube (1g) | ≈30% | Possible spike in blood glucose | Effective for children; not ideal for diabetics. |
| Valsalva maneuver (pinch nose, blow) | ≈55% | None when performed correctly | Increases intra‑thoracic pressure, resetting diaphragm. |
| Acupressure (point LI4) | ≈22% | Mild skin irritation | Requires knowledge of pressure points. |
Even if a single technique doesn’t work, combining two (e.g., breath‑hold followed by a cold sip) lifts the success odds to around 70% in most reports.
If home methods fail and the hiccups linger, clinicians have a toolbox of pharmacologic and procedural interventions.
Any medication should be prescribed after a thorough assessment, especially because some drugs interact with common prescriptions like antihypertensives.

Even with occasional hiccups, small habit changes can keep them from spiraling.
Tracking episodes in a simple journal (date, duration, possible trigger) helps you spot patterns and discuss them with your healthcare provider.
Although rare, hiccups can signal serious underlying disease. Seek urgent care if you notice any of the following alongside the hiccups:
These symptoms may indicate myocardial infarction, stroke, or a central nervous system lesion, all of which demand rapid evaluation.
Prolonged hiccups usually stem from persistent irritation of the diaphragm or vagus nerve, often due to gastro‑esophageal reflux, central nervous system irritation, or certain medications. When the trigger isn’t removed, the reflex loop keeps firing.
Yes. Stress stimulates the autonomic nervous system, which can affect the vagus nerve and increase diaphragm spasm likelihood. Relaxation techniques often reduce frequency.
A teaspoon of sugar or a bite of dry toast can stimulate the throat muscles, interrupting the reflex. Cold water, ice chips, or a spoonful of peanut butter work similarly by changing swallowing patterns.
If hiccups persist beyond 48hours, interfere with nutrition, sleep, or cause significant distress, a physician may prescribe drugs like chlorpromazine, metoclopramide, or baclofen after evaluating risks.
In rare cases, persistent hiccups are linked to stroke, brain tumors, or heart attack. Any accompanying chest pain, neurological deficits, or severe shortness of breath warrants emergency assessment.
Chronic hiccups, while often dismissed as a trivial nuisance, can in fact exert a profound influence on a patient’s quality of life. Recent epidemiological reviews demonstrate that episodes persisting beyond 48 hours are associated with measurable declines in functional status. The diaphragmatic spasm interferes with normal ventilation patterns, which leads to subtle hypoxia during sleep. This nocturnal disturbance frequently results in fragmented sleep architecture and daytime somnolence, a cascade that compounds existing fatigue. Moreover, the repetitive convulsions can impair esophageal motility, precipitating dysphagia and subsequent weight loss. Studies from tertiary care centres report that up to 20% of chronic hiccup patients develop clinically significant malnutrition. Psychological ramifications are equally salient; the involuntary nature of hiccups fosters social embarrassment and can precipitate avoidant behaviours. In a 2023 multi‑centre cohort, participants with persistent hiccups scored an average of 12 points lower on the SF‑36 mental health subscale compared to matched controls. The persistent auditory disruption also strains interpersonal communication, often prompting patients to withdraw from group settings. From a pathophysiological standpoint, the afferent loop involving the vagus nerve and phrenic nerve demonstrates heightened sensitivity to gastric acidity, especially in gastro‑oesophageal reflux disease (GERD). Targeted pharmacologic therapy, such as low‑dose baclofen, has been shown to attenuate this reflex arc and improve symptom control in 58% of cases. Nevertheless, the evidence base remains limited and largely derived from small case series, underscoring the need for robust randomised trials. Clinicians should maintain a high index of suspicion for underlying neurological or metabolic disorders when hiccups persist beyond a week. Imaging studies, including MRI of the brainstem, may be indicated in refractory cases to exclude structural lesions. Ultimately, a multidisciplinary approach involving gastroenterology, neurology, and behavioural therapy yields the best outcomes for patients navigating this obscure yet debilitating condition. The goal is not merely to silence the hiccup but to restore the patient’s functional autonomy and psychosocial wellbeing. While the literature is still evolving, practitioners must remain vigilant and proactive in addressing this often‑overlooked symptom complex.
It’s truly heartbreaking, how something as innocuous‑looking as a hiccup can cascade, creating ripples of distress, especially when someone is already juggling work, family, and health concerns, and the manner in which these involuntary spasms infiltrate sleep cycles, leading to chronic fatigue, is a matter that deserves our undivided attention, and let’s not forget the social stigma attached, which can exacerbate feelings of isolation, particularly in cultures where uninterrupted conversation is valued, and the medical community must therefore adopt a more empathetic stance, offering not just pharmacological solutions but also comprehensive lifestyle guidance, such as mindful eating practices, stress‑reduction techniques, and thorough medication reviews, because each of these elements plays a pivotal role in mitigating triggers and fostering overall wellbeing.
I swear the hiccups felt like a tiny army marching in my chest.
Wow, the sheer drama of a relentless hiccup attack is like a Broadway show that never ends! 🎭✨ It’s astonishing how the body can turn a simple “hic” into an epic saga that disrupts meals, meetings, and even romantic moments. If you’re stuck in this loop, remember that you’re not alone, and there are tricks-like the good ole Valsalva maneuver-that can steal the spotlight from those pesky spasms. 🌟💪
Sleep loss from hiccups is a real issue.
Hey folks, don’t lose hope! 🌈 Even if hiccups stick around, a mix of breath‑holding, a cold sip, and a pinch of humor can often break the cycle. Keep a journal, stay hydrated, and remember that you’ve got this!
Honestly, the literature makes it clear that chronic hiccups aren’t just a quirky footnote in gastroenterology-they’re a legitimate clinical entity demanding nuanced management, and the consensus among seasoned practitioners is to first eliminate reversible triggers before escalating to pharmacotherapy, which, while effective in a subset of patients, carries its own risk profile that must be weighed against the severity of the hiccup burden.
Let’s get precise: the vagus nerve’s afferent pathway can be irritated by acidic reflux, leading to a feedback loop that manifests as hiccups. If you’re experiencing this, consider a trial of a proton‑pump inhibitor combined with diaphragmatic breathing exercises. Also, watch for medication side‑effects-some steroids and chemotherapeutics are known culprits.
Another day, another hiccup saga-sure, the remedies sound like old wives’ tales, but if the Valsalva doesn’t work, maybe it’s time to see a doc. The last thing we need is to keep shrugging it off while the underlying issue lurks.
From a cultural perspective, it’s interesting how different societies have distinct folk remedies for hiccups-ranging from sipping water upside down in Japan to breathing into a paper bag in the US. While many lack rigorous scientific backing, some may offer placebo benefits that aid in symptom relief.
Oh great, another “miracle cure” thread-let’s just skip the hype and stick to the evidence. If you’ve tried sugar and water without luck, it’s time for a proper evaluation rather than scrolling through endless anecdotal tips.
The data clearly shows that persistent hiccups are a sign of underlying pathology-nothing to brag about. If you’re using this as a badge of honor, you’re missing the point: seek proper medical attention before you turn this into a chronic joke.
In many places the cure is simple a sip of cold water but also consider the diet a lot of spicy food can trigger the reflex ignore it if you cant change it
Yo! If you’re stuck in hiccup hell, try mixing a spoonful of peanut butter with a cold drink-makes your throat muscles do a little dance and can break the loop. Also, don’t forget to keep a smile on-your brain likes a good vibe. 🌟
Nice points above-just add that staying positive and keeping a routine can really help. Keep it up!