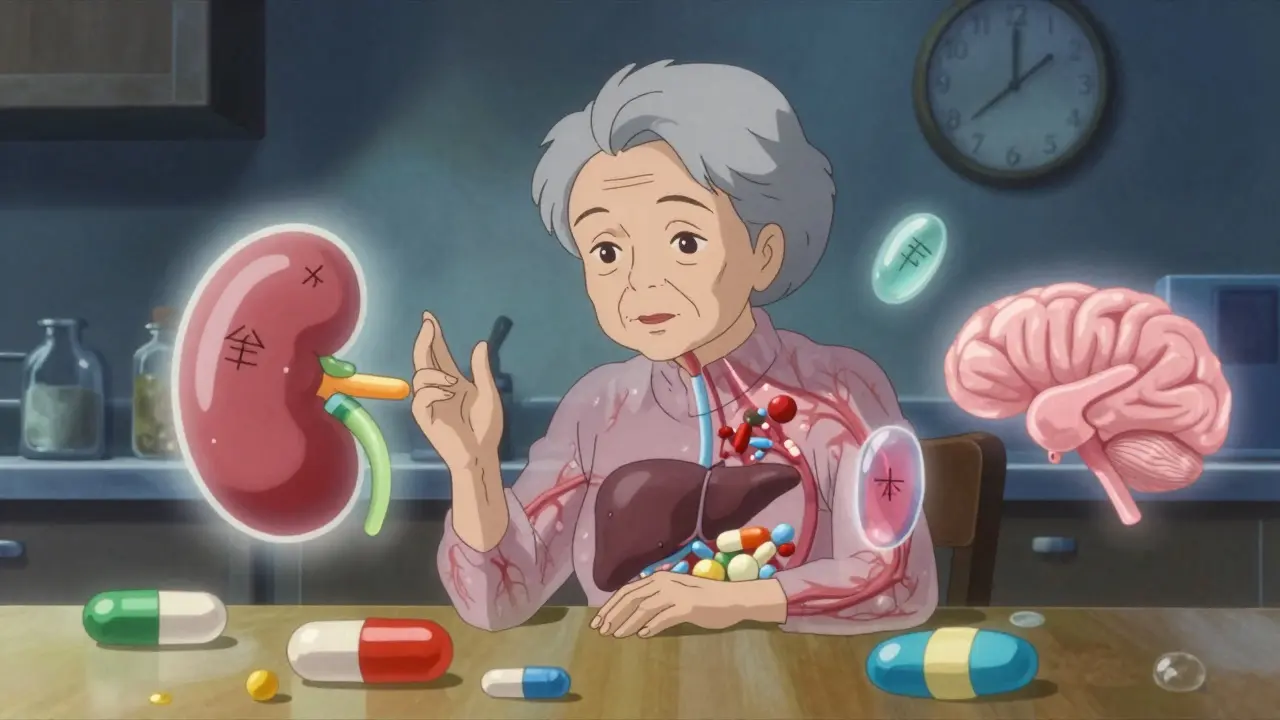
By the time you hit 65, your body doesn’t process medicine the same way it did at 35. It’s not just about taking more pills-it’s about how those pills work inside you. Many older adults take five or more prescriptions daily, and for good reason: high blood pressure, arthritis, diabetes, heart conditions. But what most people don’t realize is that the same dose that worked perfectly at 50 might cause serious side effects at 80. This isn’t guesswork. It’s science. And it’s why so many seniors end up in the hospital-not because they took too many pills, but because their bodies changed, and no one adjusted the dose.
Your body isn’t just getting older-it’s rewiring how it handles drugs. Two major systems take the hit: how your body absorbs and moves medicine (pharmacokinetics), and how your cells respond to it (pharmacodynamics). Both shift dramatically with age.
Take your kidneys. After age 40, your kidney’s filtering power drops by about 0.8 mL per minute every year. By 80, that’s a 30-50% drop. That means drugs like digoxin, warfarin, or antibiotics that your kidneys flush out? They stick around longer. Build up. And that’s when you start feeling dizzy, confused, or nauseous-not because you’re overdosing, but because your body can’t clear the drug like it used to.
Your liver doesn’t fare much better. Blood flow to the liver drops by 30-40% in older adults. That affects drugs like propranolol or lidocaine that rely on liver blood flow to break down. Slower breakdown = longer half-life = higher risk of toxicity. Even if you take the same amount, your body holds onto it longer.
Then there’s body composition. As you age, muscle mass shrinks and fat increases. That changes where drugs go. Lipid-soluble drugs like diazepam or antidepressants? They settle into fat tissue and release slowly. That’s why a 10 mg dose of diazepam at 70 might feel like 20 mg at 30. The drug lingers, and the sedation lasts longer.
Protein levels in your blood drop too. Albumin, the main carrier for drugs like warfarin or phenytoin, declines from 4.5 g/dL to 3.8 g/dL by age 80. Less albumin means more free, active drug floating around-increasing effects and side effects. You’re not taking more. Your body is just letting more of it do its job.
It’s not just about how your body moves the drug-it’s about how your cells react to it. This is pharmacodynamics, and it’s where things get even trickier.
Your brain becomes more sensitive to central nervous system depressants. Benzodiazepines, sleep aids, even antihistamines like diphenhydramine (Benadryl) can cause confusion, falls, or memory lapses in older adults. Why? Blood-brain barrier changes, fewer neurons, and less natural neurotransmitter balance. One study found that 25% of adults over 75 develop confusion from diphenhydramine, compared to just 5-8% in younger people. That’s a fivefold increase.
Your heart responds differently too. Beta-adrenergic receptors-those that respond to adrenaline and medications like albuterol or beta-blockers-lose up to 50% of their function by age 70. That means a standard dose of a beta-blocker might not slow your heart enough. But here’s the catch: your body still responds to alpha-receptors, which control blood pressure. So you might stay hypertensive, but get dizzy from low blood pressure. It’s a mismatch.
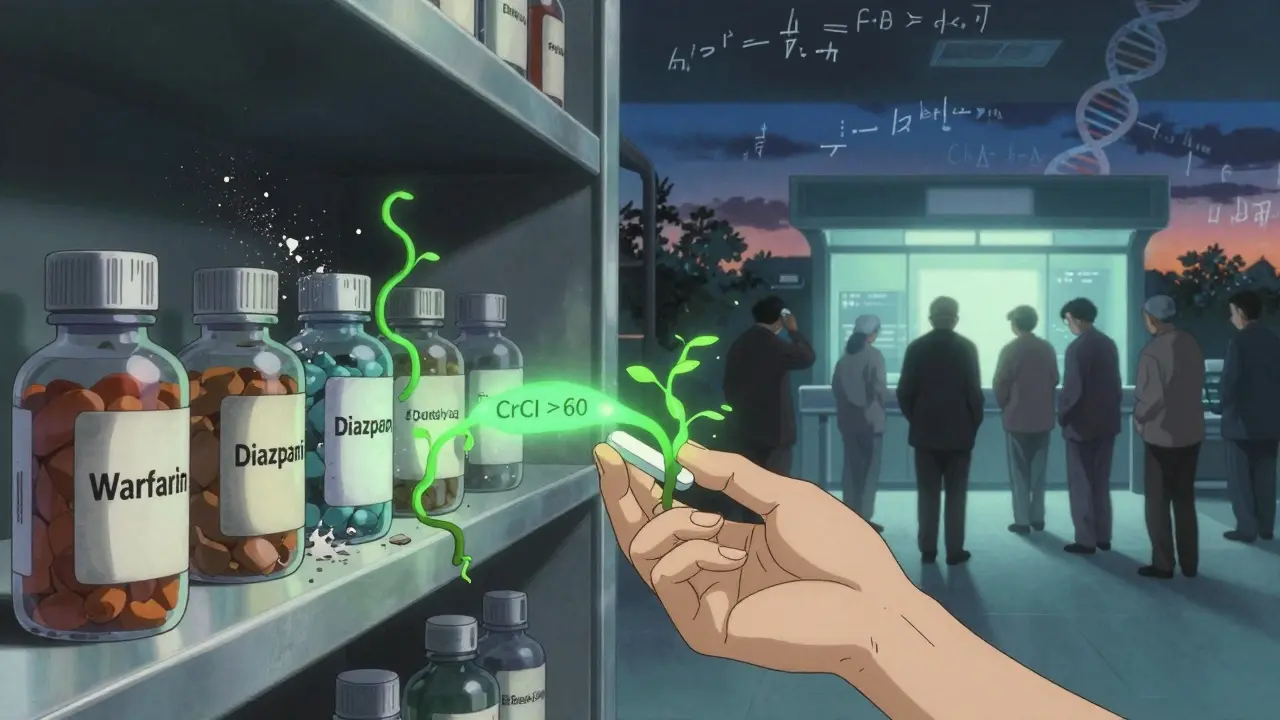
Anticoagulants like warfarin? Older adults need 20-30% less. Why? Your liver makes fewer clotting factors, and vitamin K metabolism slows. A dose that’s perfect for a 50-year-old could cause dangerous bleeding in someone 80. In fact, warfarin alone causes over 125,000 emergency room visits each year in older adults in the U.S.
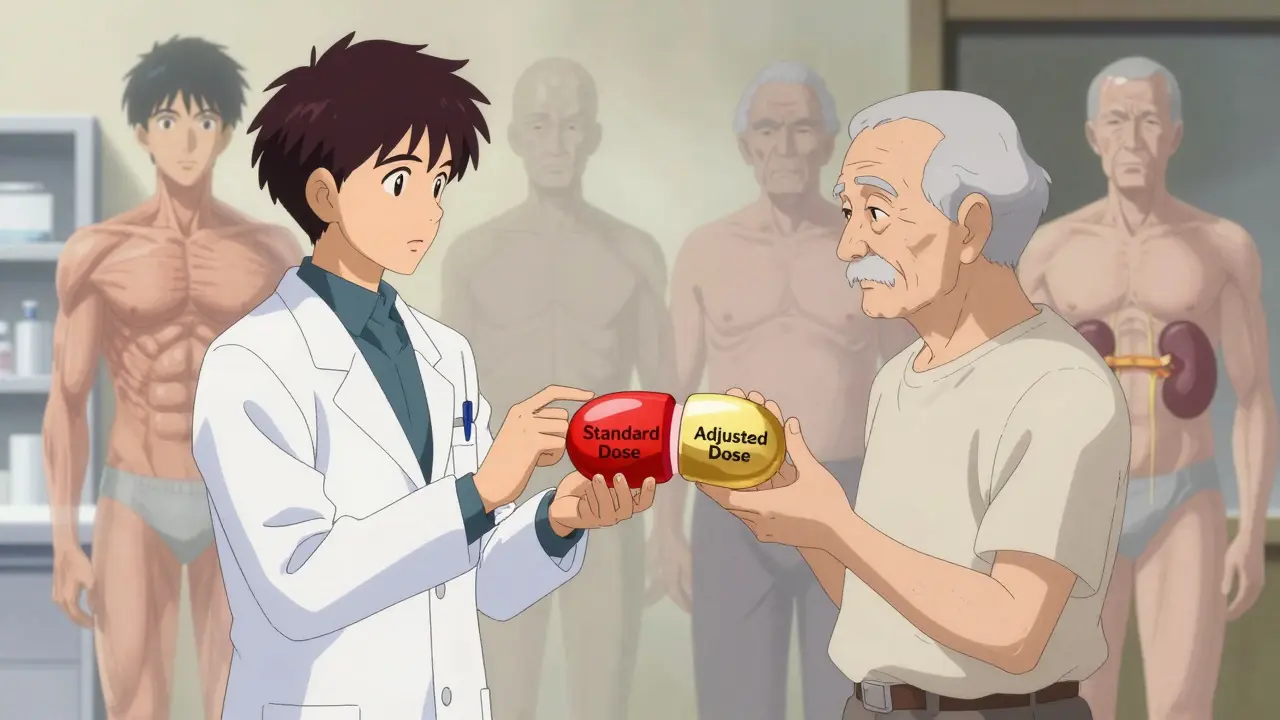
Most drug labels still list doses based on trials done mostly on people under 65. That’s a problem. In 2022, the FDA found that 73% of new drugs approved between 2018 and 2022 had to include geriatric dosing adjustments because clinical trials showed older adults reacted differently. But most prescriptions still follow the old labels.
Doctors often don’t adjust doses because they’re not trained to. A 2021 JAMA study found that 60% of adverse drug events in seniors happened simply because prescribers didn’t account for reduced kidney function. Serum creatinine alone doesn’t tell the story-you need to calculate creatinine clearance using the Cockcroft-Gault equation. Many clinics still skip this step.
And then there’s the ‘start low, go slow’ rule. It’s not a suggestion-it’s a necessity. Pharmacists report that 68% of them begin with 25-50% of the standard dose for seniors over 75, especially for kidney-cleared drugs. And 82% say it leads to fewer side effects and hospital visits. Yet, many doctors still start at the full dose.
Some drugs are more dangerous for older adults than others. The American Geriatrics Society’s Beers Criteria (2023 update) lists 30 classes of medications that should be avoided or adjusted. Here are the big ones:
Even common OTC meds like sleep aids or allergy pills can be dangerous. Many seniors don’t realize they’re taking anticholinergics every night. That’s why tools like the Anticholinergic Cognitive Burden Scale are now used in 65% of VA hospitals-to quantify risk and guide changes.
You don’t need to be a doctor to protect yourself or a loved one. Here’s what actually works:
Things are starting to shift. The FDA now requires pharmacokinetic studies in adults over 65 for all new drugs. In 2023, they approved the first age-adjusted dosing algorithm for dabigatran (Pradaxa), cutting major bleeding in seniors over 80 by 31%. That’s huge.
Researchers are also looking at cellular aging. Senescent cells-old, damaged cells that don’t die-release inflammatory chemicals that mess with how drugs work. In trials, drugs that clear these cells (like dasatinib and quercetin) restored drug responsiveness in aged tissue. It’s early, but it’s proof that aging isn’t just a number-it’s a biological process that changes how medicine works.
The future of geriatric dosing is personalized. Platforms like DosemeRx are already using kidney function, weight, age, and genetics to calculate exact doses. And the National Institute on Aging is investing $85 million to study how aging affects drug metabolism genes. This isn’t science fiction. It’s the next step in safe care.
But here’s the hard truth: only 12% of clinical trial participants are over 75. That means most dosing rules are based on data from people who aren’t like you. If you’re over 65, you’re not just a patient-you’re part of the solution. Ask questions. Demand reviews. Push for testing. Your body doesn’t work like it used to. Your medicine shouldn’t either.
Older adults need lower doses because their bodies process drugs differently. Kidneys and liver work slower, fat increases while muscle decreases, and proteins that carry drugs in the blood decline. This means drugs stay in the body longer and at higher active levels. Even a standard dose can become toxic. For example, a drug cleared by the kidneys might build up to dangerous levels if kidney function has dropped by 40%.
No. Stopping suddenly can be dangerous-especially for blood pressure, heart, or seizure medications. Instead, write down your symptoms, when they started, and what you’re taking. Then talk to your doctor or pharmacist. They can help you taper safely or switch to a safer alternative. Never adjust doses on your own.
Not always. Many OTC meds contain anticholinergics (like diphenhydramine in sleep aids or allergy pills) or NSAIDs (like ibuprofen), which are risky for older adults. These can cause confusion, falls, kidney damage, or bleeding. Always check the active ingredients. If you see ‘antihistamine,’ ‘drowsiness,’ or ‘NSAID,’ ask your pharmacist if there’s a safer option.
Serum creatinine alone doesn’t tell you. You need the estimated creatinine clearance (CrCl), calculated using your age, weight, sex, and creatinine level. The Cockcroft-Gault formula is the standard. Ask your doctor for your CrCl number. If it’s below 60 mL/min, most medications need dose adjustments. Many clinics still don’t check this-so ask.
Use the American Geriatrics Society’s Beers Criteria app-it flags risky drugs for seniors. Use the Anticholinergic Burden Calculator to see how much anticholinergic load you’re carrying. Consider a pill organizer with alarms. And schedule a yearly medication review with your pharmacist. They’re trained to spot interactions and unnecessary prescriptions. Over 68% of pharmacists now use a ‘start low, go slow’ approach for seniors-ask them to apply it to your regimen.
The body isn't a machine you can just recalibrate with a dial. It's a living archive of every meal, every stress, every sleepless night. At 80, your liver isn't lazy-it's exhausted. Your kidneys aren't failing-they're conserving. And yet we keep prescribing like youth is the default setting. We treat aging like a bug in the system instead of the operating system itself. This isn't about dosage. It's about humility. The science is clear. The arrogance isn't.
I've seen this in my dad. He was on warfarin for atrial fibrillation. Dose never changed since he was 68. At 82, he started falling. Not because he was weak. Because his blood was too thin. No one checked his CrCl. Just assumed 'same dose, same result.' It took three ER visits and a pharmacist to finally say: 'We need to cut this in half.'
There’s a quiet tragedy in geriatric pharmacology: we optimize for clinical trials, not for lived experience. The same pill that stabilizes a 55-year-old’s BP can destabilize an 80-year-old’s equilibrium. It’s not just physiology-it’s dignity. Falling isn’t just a risk. It’s the loss of independence. A single dose adjustment isn’t medical-it’s a lifeline. And yet, we still treat it like an afterthought.
i just want to say thank you for writting this. my mom is 79 and she takes 7 pills a day. i never knew about the albumin thing. or how kidney function drops by 0.8 ml per min. i thought she was just getting 'old.' turns out, she's being poisoned by outdated dosing. i took her to her pharmacist yesterday. they did a full review. cut 2 meds, lowered 3. she's not dizzy anymore. i wish every family had this info.
So let me get this straight. We have the science, the data, the guidelines-and yet doctors still prescribe like we’re in 1995? The FDA says 73% of new drugs need geriatric adjustments. But your GP? Still using the same chart from the 80s. It’s not negligence. It’s willful ignorance wrapped in a white coat.
Every time I see my grandma take Benadryl for allergies, I cringe. She thinks it’s harmless. But it’s a silent thief-stealing her focus, her balance, her future. I showed her the Beers Criteria app. She laughed. Then she cried. Now she refuses anything with diphenhydramine. Small victory. But it’s a start.
my old man was on ibuprofen for years. said his knees felt better. then he got a GI bleed. turned out his kidneys were at 42 ml/min. no one ever checked. we switched to acetaminophen, checked his liver, and now he walks without pain. no magic pill. just a simple question: 'have you checked his clearance?'
This is the kind of info that changes lives. I work in a senior center and I hand out printouts of the Beers Criteria like candy. People light up when they realize they don’t have to live with dizziness, confusion, or falls just because they’re old. It’s not about being frail. It’s about being smart. And we owe our elders that much.
India has been doing this right for decades. We don’t blindly follow Western guidelines. Our elders take half-doses out of tradition, not trial data. They’ve been adjusting naturally for generations. Why do we need fancy algorithms when common sense and family care still work? The West is overcomplicating what our grandmothers knew instinctively.
Let’s be brutally honest: most doctors are clueless about geriatric pharmacology. They were taught in med school that aging = more pills. Not less. They don’t calculate CrCl because they don’t know how. They don’t ask about OTC meds because they’re too busy. And patients? They’re too scared to question. This isn’t a medical problem. It’s a systemic failure. We need mandatory geriatric pharmacology training. Not as an elective. As a requirement. Or people will keep dying from pills meant to save them.
Interesting. But let’s not pretend this is revolutionary. We’ve known about renal decline since the 70s. The real issue? Pharma doesn’t want to re-dose. It’s cheaper to keep selling the same bottle. And doctors? They’re incentivized to write scripts, not review them. This isn’t science. It’s profit.
I’m a nurse. I’ve seen 78-year-olds on full-dose beta-blockers because their chart says '5mg daily.' Their heart rate drops to 42. They’re fine. Until they’re not. Then they crash. We don’t need new studies. We need to stop pretending that a 70-year-old is just a 30-year-old with wrinkles. The science is old. The ignorance is new.