Imagine touching a doorknob and it feels like your skin is burning. Or someone brushing past you in a hallway sends sharp pain shooting through your arm-even though there’s no injury, no swelling, no visible damage. This isn’t imagination. It’s central sensitization.
What Exactly Is Central Sensitization?
Central sensitization is when your nervous system gets stuck on high volume. It’s not that something’s broken in your muscles or joints. It’s that your brain and spinal cord have become oversensitive. They start turning normal signals-like light touch, a breeze, or even normal movement-into pain signals. This isn’t just "feeling pain." It’s your nervous system rewiring itself to amplify pain, even when there’s no ongoing tissue damage.
This isn’t new. Back in 1983, neuroscientist Clifford J. Woolf first described it as a "wind-up" effect in the spinal cord. Think of it like an alarm system that keeps ringing even after the fire’s out. The original trigger might have been an injury, surgery, or infection. But once central sensitization kicks in, the alarm keeps going off on its own.
It’s a major reason why some people still hurt months or years after an injury has healed. About 35-45% of people with chronic low back pain that lasts longer than three months have central sensitization. Up to 90% of people with fibromyalgia show clear signs of it. And it’s not rare-roughly 2-4% of the global population lives with conditions driven by this mechanism.
How Your Nervous System Gets Tricked
Your body has two main systems for managing pain: the "go" system and the "stop" system. The go system sends pain signals up from your body to your brain. The stop system sends signals back down to calm things down.
In central sensitization, both systems go haywire. The go system gets louder. The stop system gets weaker. Here’s how:
- Neurons in your spinal cord become hyper-excitable. They fire more easily and more often.
- Chemical messengers like cytokines increase by 30-50% in nerve tissues, creating a low-grade inflammatory environment in your nervous system.
- Your brain’s pain-processing areas light up more on fMRI scans-up to 35% more than in people without this condition.
- Your body’s natural painkillers (like endorphins) don’t work as well. Mu-opioid receptor binding drops by 15-25%.
- Descending inhibition-the brain’s ability to dial down pain-falls by 30-50%.
This isn’t just theory. It’s measurable. In clinical tests, people with central sensitization have pain thresholds 20-30% lower than average. They feel pain from light pressure that most people wouldn’t notice. That’s called allodynia. They also feel pain more intensely from things that normally hurt a little-that’s hyperalgesia.
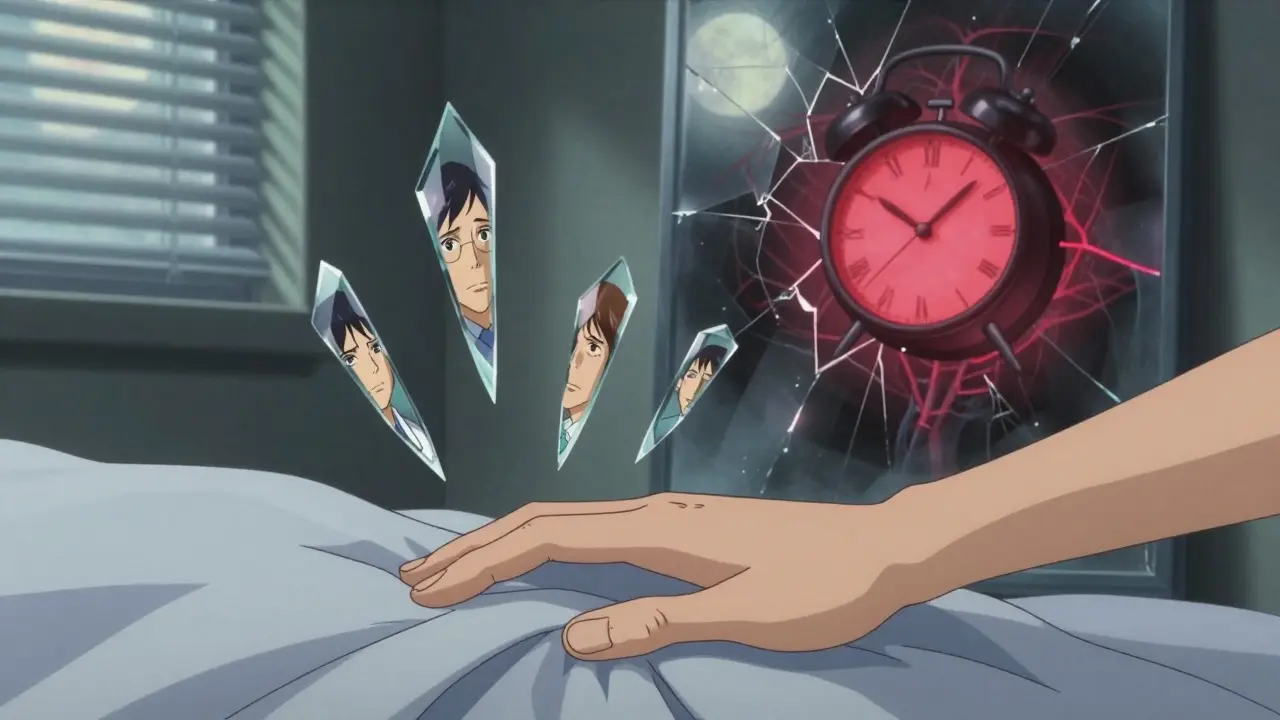
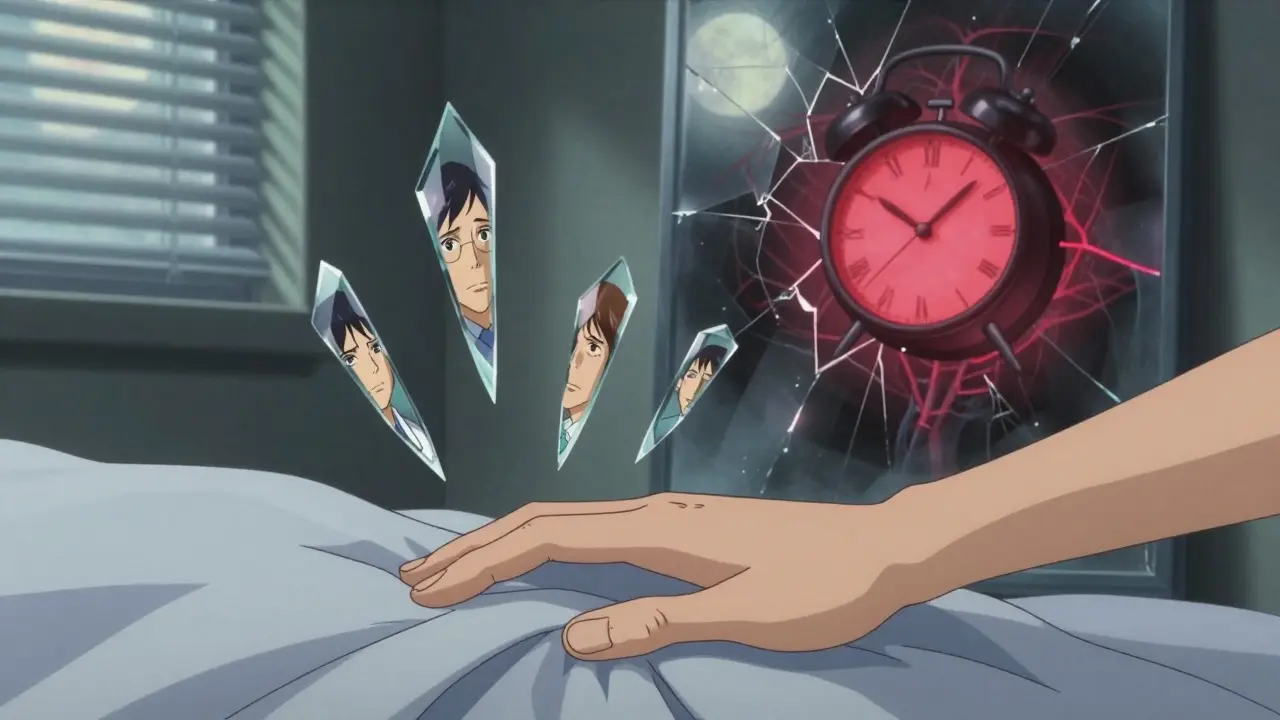
What Does It Feel Like?
People living with central sensitization describe it in similar ways:
- Pain that spreads beyond where the original injury happened.
- Light touch-like clothing or a blanket-feels painful or burning.
- Pain that moves around-today it’s your neck, tomorrow your knees.
- Being overwhelmed by noise, light, or smells.
- Brain fog-trouble focusing, remembering, or finding words.
- Sleep that doesn’t feel restful, even after eight hours.
A 2023 Reddit thread with over 140 comments from people with fibromyalgia found that 85% described pain from light touch as a burning sensation. Nearly 80% said their pain spread to areas that were never injured. These aren’t exaggerations. They’re clinical realities.
And here’s the cruel part: many people are told it’s "all in your head." That’s not just hurtful-it’s wrong. Central sensitization isn’t psychological. It’s neurophysiological. Your brain isn’t imagining pain. It’s processing it differently because of real, measurable changes in your nervous system.

How Is It Diagnosed?
There’s no single blood test or X-ray for central sensitization. Doctors use a mix of clinical signs and simple tests:
- Pain drawings: Patients mark where they hurt. In central sensitization, pain is often widespread-not following nerve paths or anatomical patterns. About 80% of cases show non-anatomical pain maps.
- Quantitative Sensory Testing (QST): A device applies controlled pressure, heat, or vibration. People with central sensitization feel pain at much lower levels than normal.
- Conditioned Pain Modulation: A second painful stimulus (like cold water) is applied elsewhere. In healthy people, this reduces the first pain. In central sensitization, it barely helps-showing the body’s natural pain-dampening system is broken.
These tests aren’t perfect. Only about 65% of clinicians agree on a diagnosis. But when you see widespread pain, allodynia, and no clear structural cause, central sensitization is the most likely explanation.
How It’s Different From Other Types of Pain
Not all chronic pain is the same.
- Peripheral pain comes from damaged tissue-like a sprained ankle or a torn tendon. It usually fades as the tissue heals, within 6-12 weeks.
- Neuropathic pain comes from nerve damage-like diabetic nerve pain or sciatica. It often follows a specific nerve path (dermatome), feels electric or tingling, and is localized.
- Central sensitization is different. Pain is widespread, not confined to one area. It doesn’t follow nerve pathways. It’s disproportionate to injury. And it persists long after healing.
For example, someone with a herniated disc might have sharp leg pain-that’s peripheral or neuropathic. But if that same person also feels pain all over their body, can’t wear a watch because it hurts, and gets overwhelmed by bright lights? That’s central sensitization.
What Treatments Actually Work?
You can’t fix central sensitization by popping more ibuprofen. You need to retrain the nervous system.
Medications:
- Pregabalin (Lyrica) and gabapentin calm overactive nerves. About 52% of patients report significant relief at doses of 150-300mg daily.
- Duloxetine (Cymbalta), an SNRI, helps restore the brain’s pain-dampening signals. Around 45% see a 30% reduction in pain.
- Low-dose naltrexone (LDN) at 4.5mg nightly reduces inflammation in the nervous system. Studies show 25-35% improvement in fibromyalgia patients.
- Nortriptyline, a low-dose tricyclic antidepressant (25-50mg at night), improves sleep and reduces pain in 47% of cases.
Non-drug approaches:
- Graded exercise therapy: Start slow-5 minutes of walking, then add 10% each week. It rebuilds tolerance without triggering flare-ups. Studies show 25-40% improvement in function.
- Pain neuroscience education: Teaching patients how their nervous system works reduces fear and catastrophizing. Pain scores drop by 20-30% after just a few sessions.
- Mindfulness and stress reduction: Chronic stress keeps the nervous system on high alert. An 8-week mindfulness program improves pain interference scores by 25%.
The key? It’s not about eliminating pain overnight. It’s about lowering the volume. Reducing sensitivity. Helping the nervous system stop shouting.
Why Diagnosis Takes So Long
Most people wait years to get diagnosed. A 2023 survey found 63% saw 4-6 doctors over 2-5 years before being told what was really going on.
Why? Because many doctors still think pain must come from visible damage. Orthopedists, for example, diagnose central sensitization in only 25% of chronic pain cases. Rheumatologists do better-65% of fibromyalgia patients get it right. But the gap is huge.
There’s also a lack of training. Effective management requires 40+ hours of continuing education in pain neuroscience. Most medical schools barely touch it.
What’s Next?
Research is accelerating. The NIH raised funding for central sensitization studies from $42 million in 2018 to $63 million in 2023. Five new drugs are now in Phase II trials targeting specific mechanisms-like reducing cytokine spikes or restoring opioid receptor function.
Standardized testing tools, like those from the German Research Network on Neuropathic Pain, are now 85% reliable. And by 2026, the International Association for the Study of Pain aims to have pain neuroscience education in half of all physical therapy programs.
The future? More precise diagnosis. Better-targeted treatments. And finally, recognition that pain without visible damage isn’t "in your head”-it’s in your nervous system, and it’s real.
What You Can Do Right Now
If you suspect you have central sensitization:
- Track your symptoms. Note what triggers pain-light touch, stress, weather changes, lack of sleep.
- Find a provider who understands central sensitization. Look for pain specialists, rheumatologists, or physiotherapists trained in pain neuroscience.
- Start gentle movement. Even 5 minutes a day of walking or stretching can help retrain your nervous system.
- Reduce stress. Sleep, breathing exercises, and mindfulness aren’t "nice to have"-they’re part of treatment.
- Don’t accept being told it’s all in your head. You’re not imagining this. Your nervous system is stuck in overdrive-and it can be reset.
Central sensitization isn’t a life sentence. It’s a malfunctioning alarm system. And like any alarm, it can be recalibrated.